● UNIVENTRICULAR ATRIOVENTRICULAR CONNECTION
Univentricular atrioventricular connection describes a group of cardiac malformations where the atrioventricular connection is completely or predominantly to a single ventricular chamber. Embryologically, this malformation is thought to result from failure of the development of the bulboventricular loop stage. Much debate still exists today on the various subclassifications of cardiac anomalies within this group and what should be included or excluded (1–4). From a clinical point of view, a congenital heart defect with a univentricular atrioventricular connection, single ventricular physiology, describes a heart with one functioning ventricle with inflow from one or both atria. Numerous terms were used to describe this malformation, including univentricular heart, primitive ventricle, common ventricle, single ventricle, cor triloculare biatriatum, cor biloculare, dominant ventricle, and double inlet ventricle (DIV) (3). The classic Van Praagh classification (5), which was later modified by Hallermann et al. (6), described one or two atrioventricular valves that empty into a single ventricle and excluded mitral or tricuspid atresia (TA). Anderson’s simpler classification described a single ventricular mass with or without a rudimentary chamber and allowed for the inclusion of mitral or TA (7, 8). In Anderson’s classification, the rudimentary chamber, if present, should not have an inlet but may have an outlet (7, 8). Within univentricular atrioventricular connection, three subgroups can be identified: double inlet, where two atria connect to a single ventricle through two patent atrioventricular valves; single inlet, where one atrium connects to a single ventricle through a single atrioventricular valve; and common inlet, where both atria connect to a single ventricle through a single atrioventricular valve (1). The morphology of the ventricle is generally a left ventricular morphology with a rudimentary right chamber. On rare occasions, a right ventricular morphology with a rudimentary left chamber, or a ventricle of indeterminate morphology without a rudimentary chamber, can be seen. A single ventricle heart, which results from a surgical repair of a congenital heart anomaly, should not be classified as univentricular atrioventricular connection. Table 19.1 lists several cardiac anomalies that may show a single ventricle on fetal echocardiography. Of those, DIV and TA with ventricular septal defect (VSD) have been commonly classified in the univentricular atrioventricular connection and will be discussed in this chapter. Figure 19.1 represents four-chamber views in fetuses with different cardiac defects and a single ventricle anatomy.
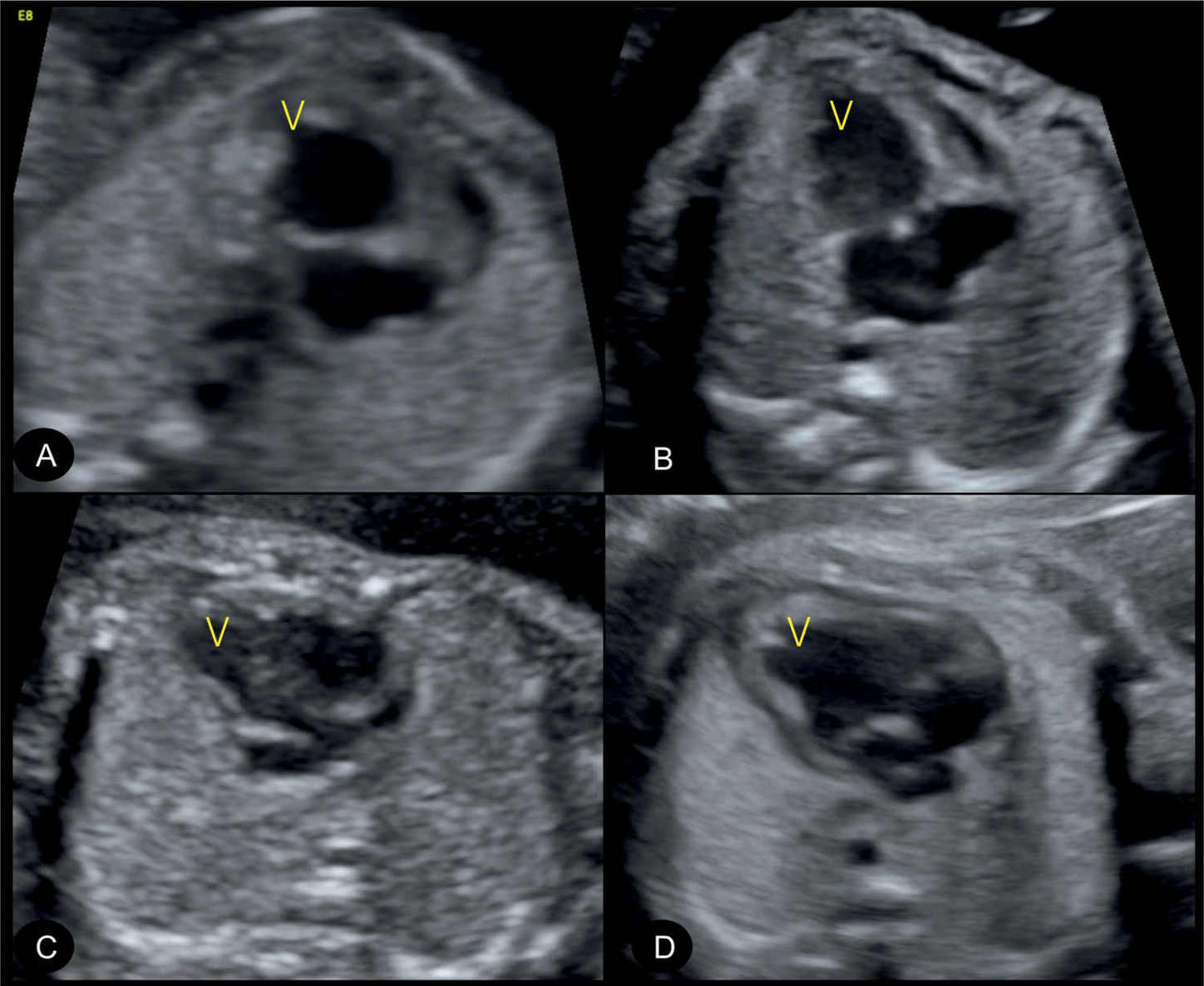
Figure 19.1: Spectrum of univentricular atrioventricular connection: four different fetal heart defects showing a “single ventricle” (V) in the four-chamber view. The detection of one ventricle on fetal echocardiography is not synonymous with a single ventricle. A: Fetus with a hypoplastic left heart with absent left ventricle in mitral and aortic atresia. B: Fetus with a hypoplastic right ventricle in pulmonary atresia with intact septum. C: Common inlet single ventricle in a fetus with right isomerism and other complex anomalies and (D) double inlet ventricle. See text and Table 19.1 for details.
Cardiac Anomalies That May Show a Single Ventricle on Fetal Echocardiography |
• Hypoplastic left heart syndrome • Pulmonary atresia with intact septum • Atrioventricular septal defect (large or unbalanced) • Single ventricle in right and left isomerism • Corrected transposition with tricuspid atresia • Mitral atresia with ventricular septal defect • Double inlet ventricle • Tricuspid atresia with ventricular septal defect |
● DOUBLE INLET VENTRICLE
Definition, Spectrum of Disease, and Incidence
DIV is considered a classic and most common form of univentricular atrioventricular connection (1). It is characterized by two normally developed right and left atria that connect via separate right and left atrioventricular valves to a common ventricle (Fig. 19.2). The most common form of DIV is a double inlet to a morphologic left ventricle, representing about 80%, and the anomaly is also called double inlet left ventricle (DILV) (5). In DILV, a small underdeveloped right ventricle (not shown in Fig. 19.2) is commonly present and connects to the single ventricle with a VSD. This “remnant” ventricle is a small outlet chamber and the septal defect is usually called bulboventricular foramen. The aorta and pulmonary arteries usually arise in D- or L-malposition, and depending on the looping, one or both vessels (double outlet) may commonly arise from the small outlet chamber. In cases where the bulboventricular foramen (septal defect) is restrictive, the corresponding arising vessel(s) from the remnant chamber may be diminutive (pulmonary stenosis or aortic coarctation). Other forms of DIV include a double inlet right ventricle, a DIV of mixed morphology, and a DIV of undetermined or undifferentiated morphology (5). DIV is rare and is found in 0.1 per 1,000 live births (9). The prevalence is more common in fetal series due to the easy detection of DIV on the four-chamber view of the heart.
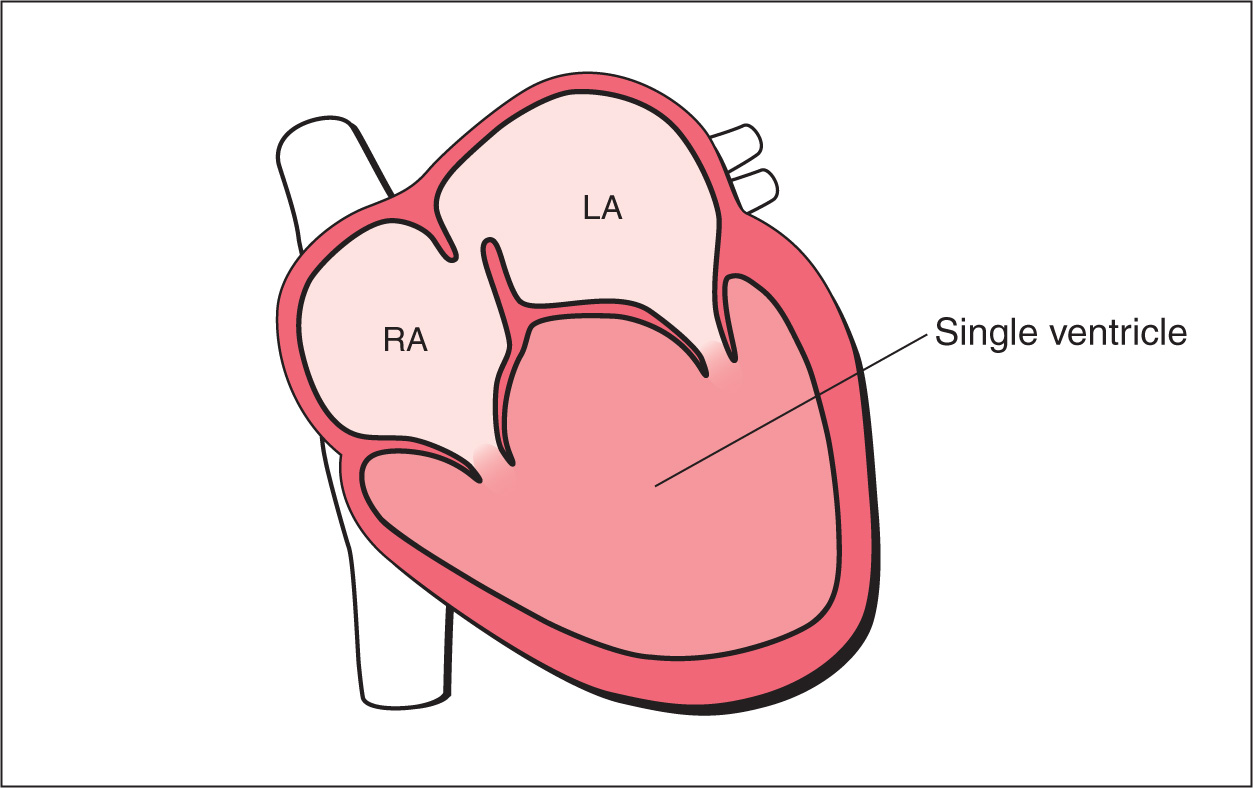
Figure 19.2: Schematic drawing of double inlet ventricle. Note the presence of right (RA) and left (LA) atria, two patent atrioventricular valves, and both atria drain into a single ventricle. In most cases, the single ventricle is morphologically a left ventricle. A rudimentary ventricle can occasionally be seen (not shown in this scheme).
Ultrasound Findings
Gray Scale
The four-chamber view is abnormal in DIV as it shows a single ventricle with a missing ventricular septum (Fig. 19.3). Identifying the morphology of the single ventricle on ultrasound is based on the anatomic characteristic of the morphologic right and left ventricles as discussed in Chapter 5. The left ventricular myocardium appears smooth with fine trabeculations, whereas the right ventricular myocardium is coarse with an irregular surface. Assessment of atrioventricular valve anatomy and/or insertion of papillary muscles cannot be used to determine ventricular morphology in univentricular atrioventricular connection. Occasionally, the rudimentary right ventricle is seen in the four-chamber plane (Fig. 19.4) but in most cases the septal defect (bulboventricular foramen) and the rudimentary right ventricle in DILV are often not visualized in the four-chamber plane but in a more cranial plane, when an attempt to visualize the great vessels is made (Fig. 19.5). The rudimentary outlet chamber in DILV is more commonly located on the left side of the main ventricle (L-looping) but can be located on the right side (D-looping) (2). The great arteries are generally in L-malposition if the small outlet chamber is on the left side of the ventricle. When the small outlet chamber is localized on the right side, the great arteries arise either in D-malposition or are normally related with the pulmonary artery arising from the small outlet chamber (2). Outflow tract obstructions are recognized due to size discrepancy rather than flow disturbances, which may be absent. A narrow pulmonary artery suggests the presence of pulmonary stenosis or atresia, whereas a narrow ascending aorta may be associated with coarctation of the aorta or tubular aortic arch hypoplasia.
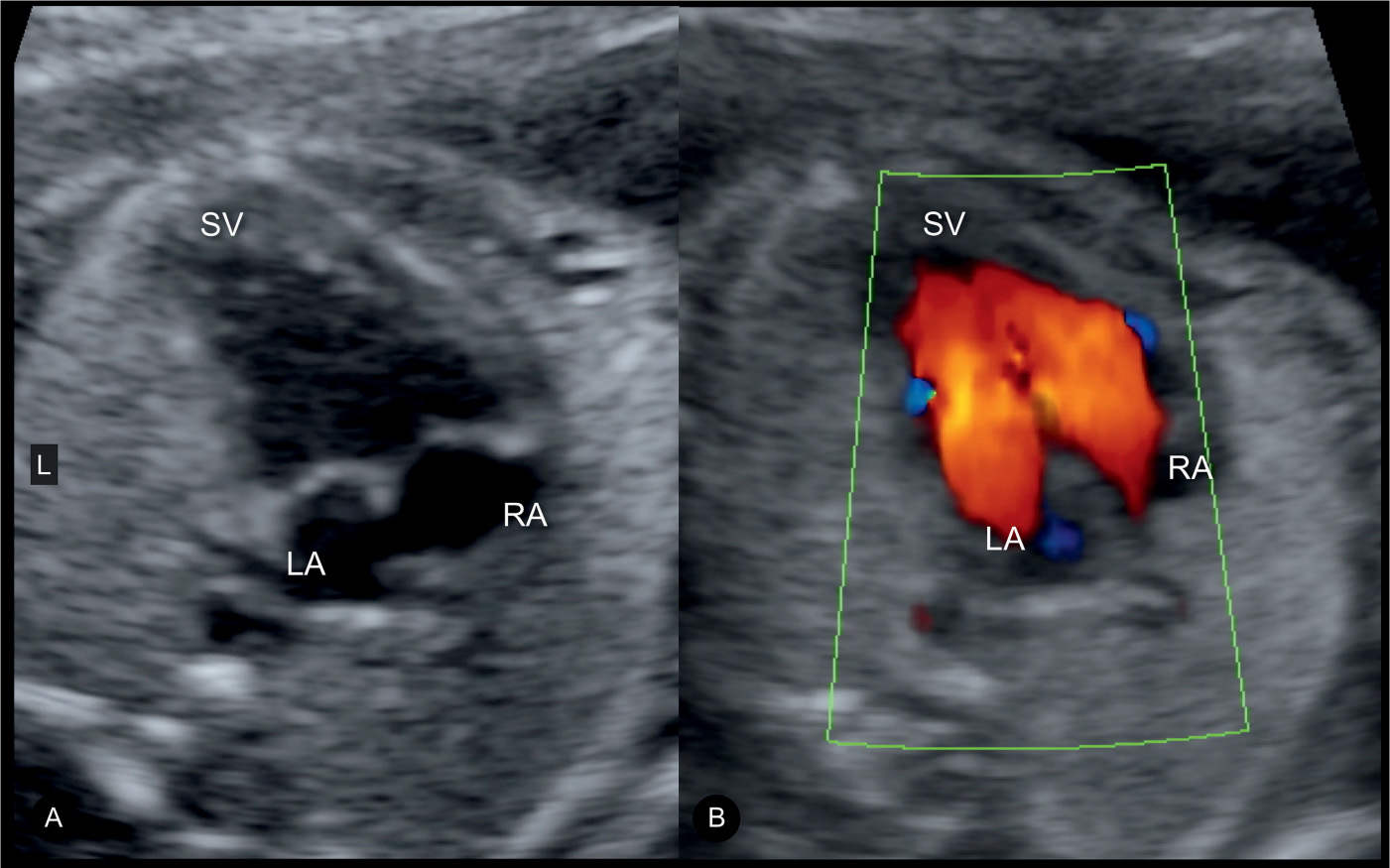
Figure 19.3: Four-chamber views in gray scale (A) and color Doppler (B) in a fetus with a double inlet ventricle. Note the presence of right (RA) and left (LA) atria and a single ventricle (SV) in A. B shows, in color Doppler, blood flow from the RA and LA through two respective atrioventricular valves into the SV. L, left.
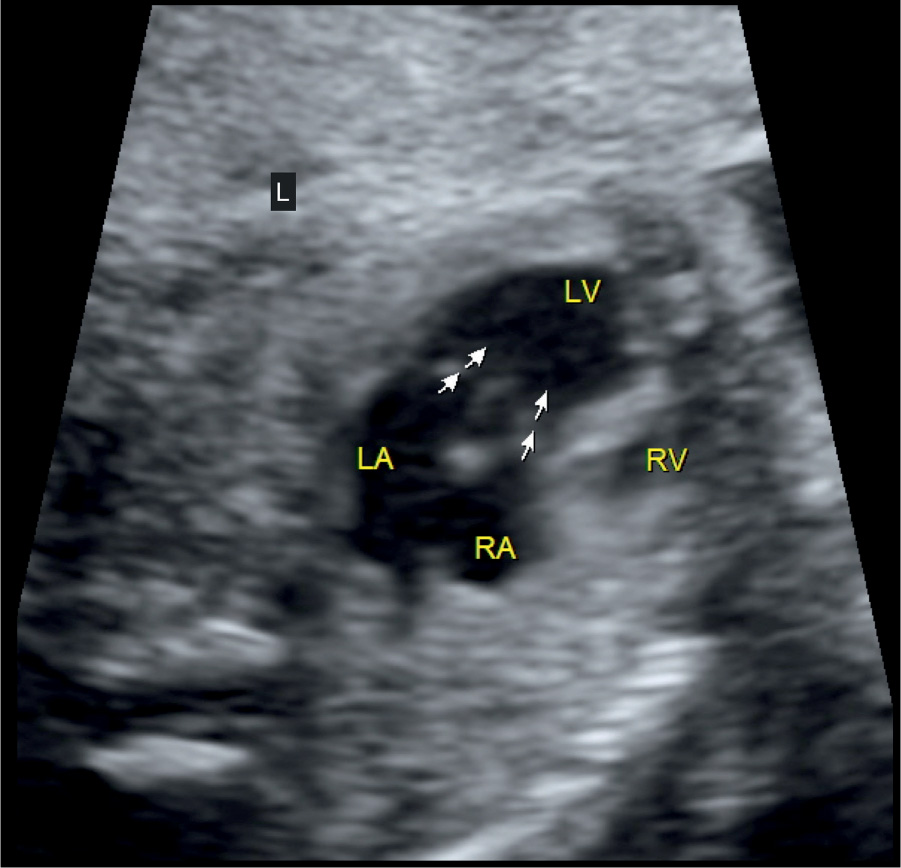
Figure 19.4: Four-chamber view in gray scale in a fetus with a double inlet ventricle. Note that the right (RA) and left (LA) atria drain through two distinct atrioventricular valves into the left ventricle (LV). There is a rudimentary right ventricle (RV) as an outlet chamber drained from the LV. L, left.
Color Doppler
Color Doppler may be misleading since two atrioventricular valves are patent and two color stripes are visualized, thus mimicking the virtual presence of a separation or septum (10) (Figs. 19.3 and 19.6). Diagnosis is typically made on grayscale ultrasound, and color Doppler provides additional information on the patency of the left and right atrioventricular valves, flow across the VSD, and great vessels (Fig. 19.5), especially to detect stenosis or atresia (Fig. 19.7). Restrictive VSD, which may occur in this condition, is better evaluated using color Doppler.
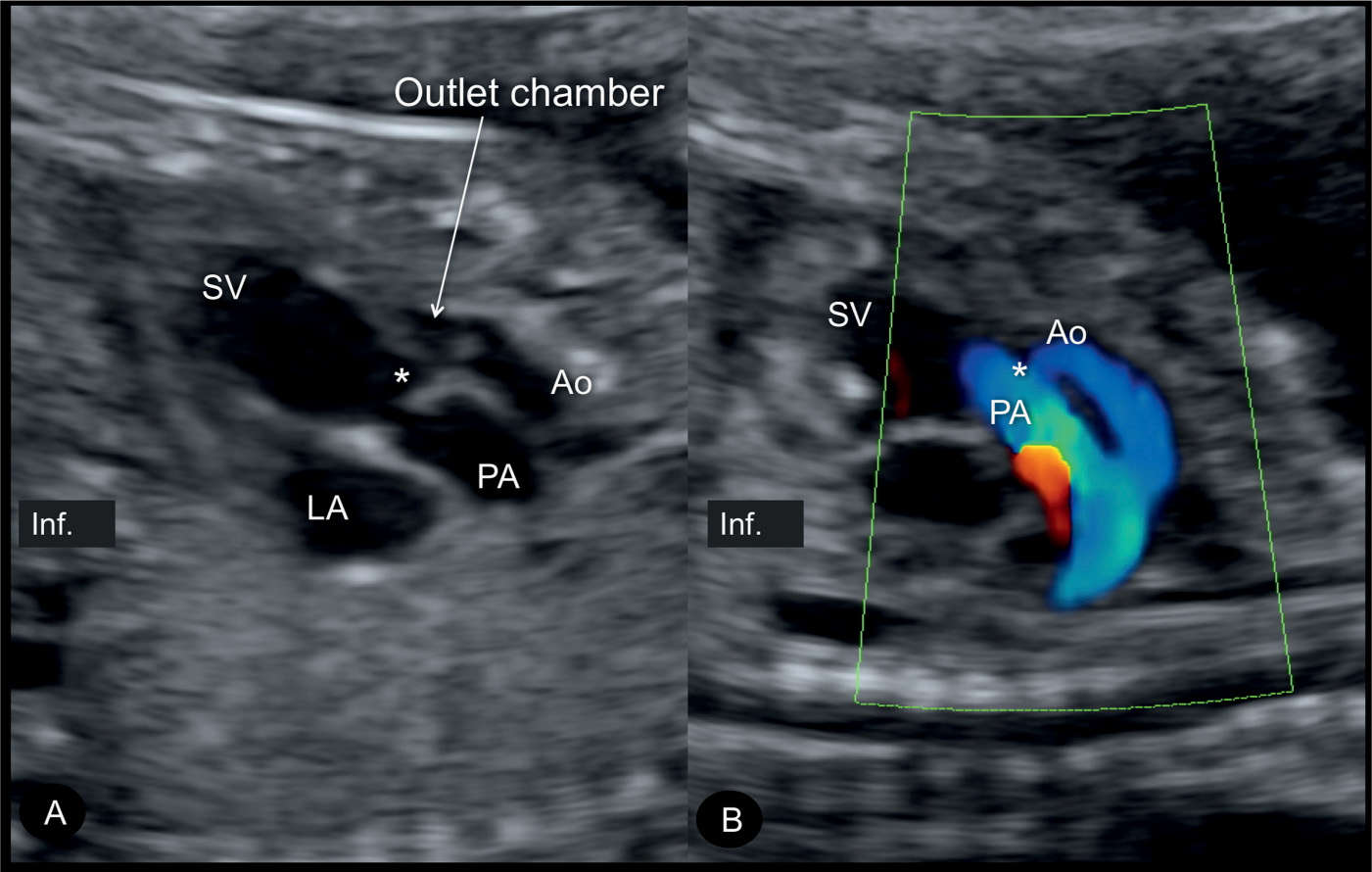
Figure 19.5: Long-axis views in gray scale (A) and color Doppler (B) in the same fetus shown in Figure 19.4 with a double inlet ventricle (SV) and a rudimentary outlet ventricle. The rudimentary outlet ventricle is connected with the SV through a ventricular septal defect (asterisk), called bulboventricular foramen. Aorta (Ao) and pulmonary artery (PA) arise in parallel orientation. Note that the Ao is smaller than the PA, due to the small size of the ventricular septal defect. Aortic coarctation was diagnosed after birth. Inf., inferior.
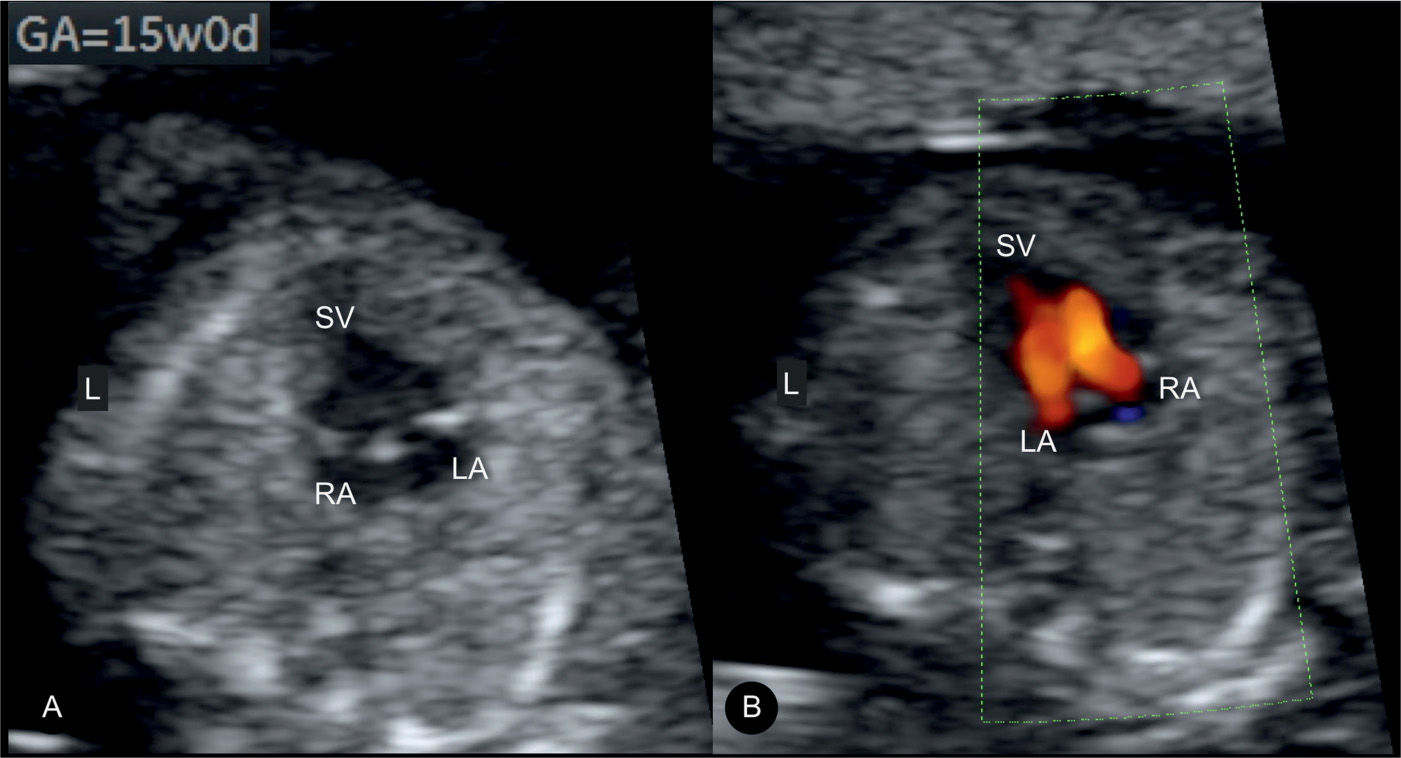
Figure 19.6: Fetus at 15 weeks’ gestation with a double inlet ventricle, with both right (RA) and left (LA) atria draining through two respective atrioventricular valves into a single ventricle (SV). A is in gray scale and B is in color Doppler. L, left.
Early Gestation
DIV can be detected in early gestation (Figs. 19.6 and 19.7) by detecting the absence of a ventricular septum on the four-chamber view as well as abnormally arising great vessels.
Three-Dimensional Ultrasound
The combination of three-dimensional (3D) ultrasound with tomographic imaging permits the simultaneous visualization of the abnormality in the four-chamber plane and the demonstration of the rudimentary ventricle with the course of the great vessels. Navigating through the volume in an offline setting may facilitate the evaluation of the spatial orientation of the great arteries. Surface rendering shows the large ventricle with inflow from two atrioventricular valves and a rudimentary outlet chamber (Fig. 19.8) and may help in identifying the spatial relationship of the great vessels.
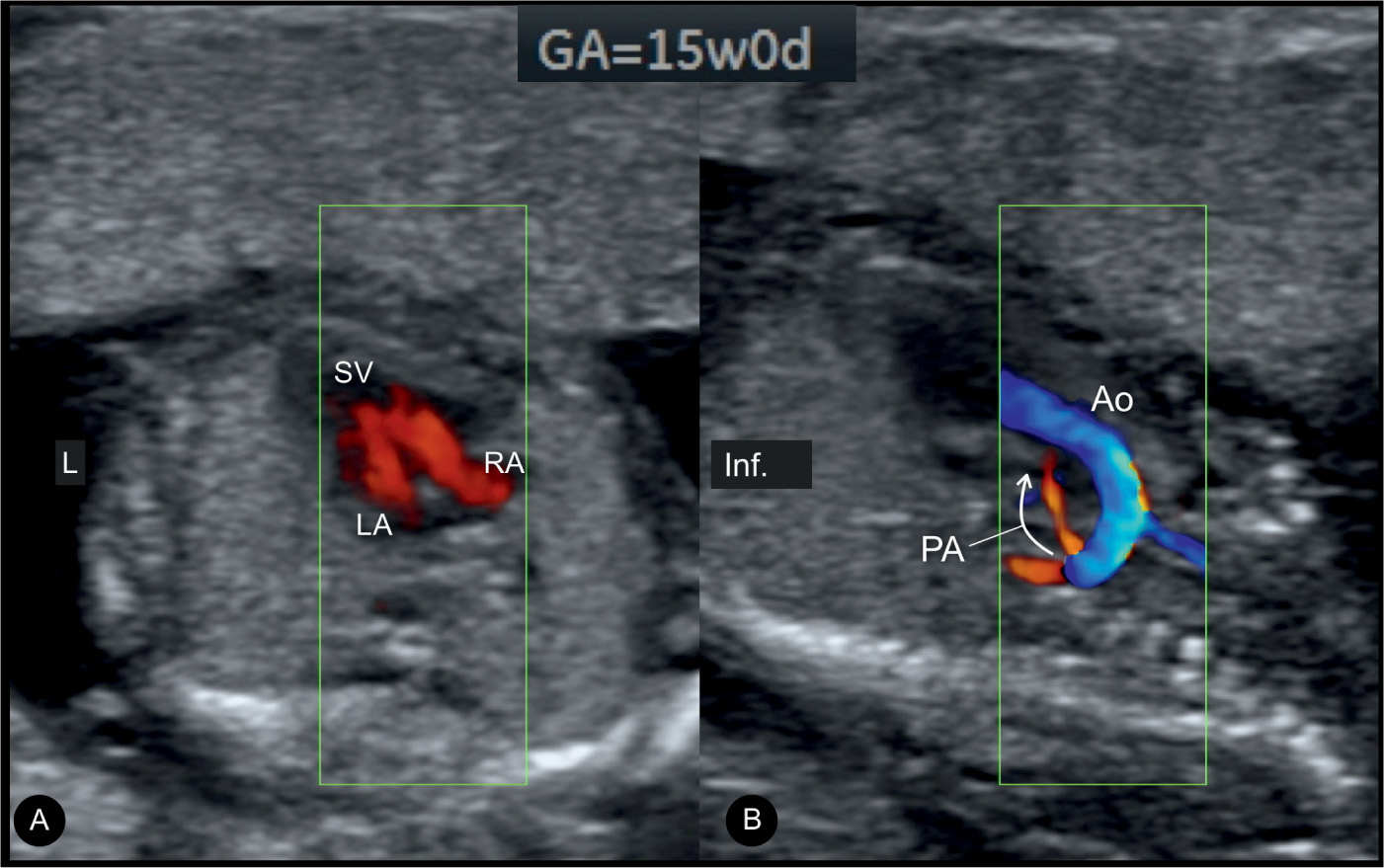
Figure 19.7: Four-chamber (A) and longitudinal (B) views in color Doppler in a fetus at 15 weeks’ gestation with a double inlet ventricle (same fetus as in Fig. 19.6). Note in A that the right (RA) and left (LA) atria drain through two respective atrioventricular valves into a single ventricle (SV). The longitudinal plane in B reveals the presence of pulmonary atresia. The pulmonary artery (PA) is hypoplastic, demonstrates retrograde flow (arrow), and is located posterior to the aorta (Ao). Inf., inferior; L, left.
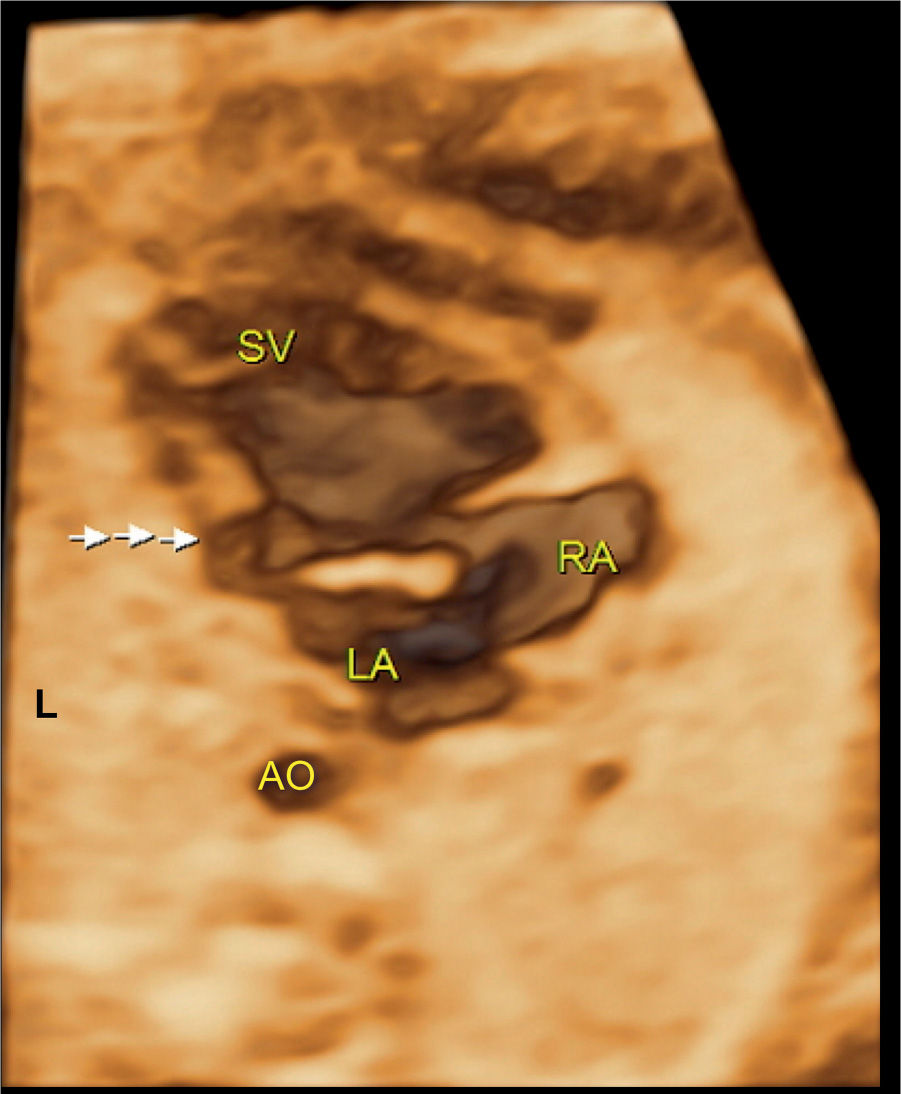
Figure 19.8: Surface-rendering mode of the four-chamber view in a fetus with double inlet ventricle showing the right (RA) and left (LA) atria as well as the single ventricle (SV). A small rudimentary ventricle can also be identified (arrows). L, left; AO, descending aorta.
Associated Cardiac and Extracardiac Findings
Associated malformations in DIV are atresia, hypoplasia or straddling of the atrioventricular valves, pulmonary (or subpulmonic) outflow obstruction, (sub)aortic outflow obstruction, and conduction abnormalities, primarily due to the anatomic disruption of the conduction system (1).
The most important extracardiac abnormality to rule out is the presence of right or left isomerism (see Chapter 30), especially in the presence of a common inlet ventricle (11). The sequential approach to the ultrasound examination of the heart may permit detection of corresponding abnormalities. Chromosome anomalies and other extracardiac anomalies than isomerism are possible but rather unusual.
Differential Diagnosis
Table 19.1 lists several cardiac malformations in the differential diagnosis of DIV. DIV may be missed on prenatal ultrasound in a lateral view of the heart in diastole because the papillary muscles may mimic a ventricular septum in a single ventricle.
Prognosis and Outcome
DIV with patent atrioventricular valves is well tolerated in the fetus. Follow-up ultrasound is important prenatally as outflow tract obstruction may develop or worsen due to reduced flow and lack of vessel growth. The neonatal course of DIV is dependent on the presence of associated malformations, such as obstruction of the great vessels or atrioventricular valve abnormalities. Surgical treatment corresponds to a single ventricular repair. The type of surgical repair (pulmonary artery banding, Fontan procedure, or other) mainly depends on detailed evaluation of the great vessel arrangement and perfusion.
An overall mortality rate of 29% with follow-up up to 25 years of age was noted in an outcome study on 105 patients with DILV and transposed arteries (12). Multivariate analysis showed the presence of arrhythmia and pacemaker requirement as independent risk factors for mortality, whereas pulmonary atresia or stenosis and pulmonary artery banding were associated with decreased mortality (12). Gender, era of birth, aortic arch anomaly, and systemic outflow obstruction were not risk factors for long-term outcome (12). Similar findings were reported on eight fetuses with DILV with L-transposition of the great vessels (13). Of these, four fetuses (50%) had pulmonary atresia, one fetus (12.5%) also had TA and coarctation of the aorta (died), and one fetus had complete heart block and long QT syndrome (died) (13). Overall good outcome was noted in six (75%) infants (13). The outcome of fetuses with DIV is generally good in the absence of associated rhythm abnormalities.
KEY POINTS  Double Inlet Ventricle
Double Inlet Ventricle
 DIV is the most common form of univentricular atrioventricular connection.
DIV is the most common form of univentricular atrioventricular connection.
 DIV is characterized by two normally developed right and left atria that connect via separate right and left atrioventricular valves to a common ventricle.
DIV is characterized by two normally developed right and left atria that connect via separate right and left atrioventricular valves to a common ventricle.
 The most common form of DIV is a double inlet to a morphologic left ventricle, representing about 80% of cases.
The most common form of DIV is a double inlet to a morphologic left ventricle, representing about 80% of cases.
 The four-chamber view is abnormal in DIV.
The four-chamber view is abnormal in DIV.
 In DIV, outflow tract obstruction is often present and affects the vessel arising from the rudimentary ventricle.
In DIV, outflow tract obstruction is often present and affects the vessel arising from the rudimentary ventricle.
 Associated malformations with DIV are atresia, hypoplasia or straddling of the atrioventricular valves, pulmonary (or subpulmonic) outflow obstruction, (sub)aortic outflow obstruction, and conduction abnormalities.
Associated malformations with DIV are atresia, hypoplasia or straddling of the atrioventricular valves, pulmonary (or subpulmonic) outflow obstruction, (sub)aortic outflow obstruction, and conduction abnormalities.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


