● INTRODUCTION
Congenital heart disease (CHD) is one of the most common congenital malformations in utero, with an incidence of about 8/1,000 live births (1). Prenatal diagnosis of CHD is traditionally made by ultrasound examination of the fetus in the second and third trimesters of pregnancy. Recently, the ability to diagnose CHD in the first trimester of pregnancy has been shown to be possible with high-resolution equipment (2, 3) (see Chapter 16).
Despite substantial advancement in ultrasound technology over the past years and increased availability of ultrasound to pregnant women, CHD remains an abnormality that is most frequently missed by prenatal ultrasonography (4) with wide detection rates (5). Indeed, prenatal detection of some form of CHD such as transposition of the great arteries remains in the range of 25% in some regions (6).
Prenatal detection of CHD has been shown to improve the outcome of fetuses with specific types of cardiac malformations (7, 8). Efforts targeted at training of health care workers in cardiac screening and referral for a fetal echocardiography for pregnancies at risk of cardiac malformations are major steps toward improving the effectiveness of screening and detection of CHD. The presence of clear guidelines on what defines cardiac screening and fetal echocardiography helps to standardize the approach to the sonographic evaluation of the fetal heart.
In this chapter, we present existing national and international guidelines for both (1) fetal cardiac screening and (2) fetal echocardiography. Indications for fetal echocardiography were discussed in Chapter 1. The reader should be aware that national and international guidelines are reviewed and updated on a regular basis. It is therefore important to refer to the most recent version of the existing guidelines for the most up-to-date information.
● DEFINITION OF TERMS AND RATIONALE FOR GUIDELINE DEVELOPMENT IN FETAL CARDIAC SCREENING AND FETAL ECHOCARDIOGRAPHY
It is important to understand the various terms that are used in standardization of practice, including ultrasound examinations. Guidelines, protocols, standards, and policies refer to the ultrasound examination itself (the cardiac screening or the fetal echocardiography examination). Certifications, credentialing, and qualifications refer to the personnel performing the ultrasound examinations, including physicians, sonographers, and allied health personnel. Accreditation, on the other hand, refers to the ultrasound laboratory/unit where the examination is performed, and thus requires evaluation of the qualifications of the personnel performing the ultrasound examination, the equipment that is being used for the ultrasound examination, compliance with existing examination guidelines, and quality assurance.
It is the opinion of the authors that the development of cardiac screening and fetal echocardiography guidelines helps in the standardization of the ultrasound examination, provides consensus on study indications, and defines the components of the fetal screening/echocardiography examination. In general, guidelines are consensus-based and reflect the scientific evidence at the time of guideline development. They reduce inappropriate variations in practice and provide a more rational basis for study referral. Guidelines also, when appropriately developed, can help to provide a focus for quality control and to assess the need for continuing education for the personnel performing the fetal cardiac examination. Guidelines may also identify shortcomings of scientific studies and suggest appropriate research topics on the subject.
● PRACTICE GUIDELINES FOR THE PERFORMANCE OF THE SONOGRAPHIC SCREENING EXAMINATION OF THE FETAL HEART
Typically, screening programs are intended to be applied to the low-risk population, and thus should be part of the routine care. Screening programs for CHD are, in general, incorporated into routine prenatal care and made available to all pregnant women. Pregnancies at high risk for CHD or suspected heart anomalies will require more comprehensive evaluation using fetal echocardiography.
Sonographic Cardiac Screening—Guidelines from the International Society of Ultrasound in Obstetrics and Gynecology (ISUOG)
The International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) published in 2013 the updated practice guidelines for the sonographic screening of the fetal heart (9). These guidelines are comprehensive and provide an unambiguous approach to fetal cardiac screening.
Fetal cardiac screening guidelines are most optimally performed between 18 and 22 weeks’ gestation. Ultrasound examinations performed at an earlier gestation, such as in the late first and early second trimesters of pregnancy, have been shown to identify cardiac malformations, but typically require high-resolution equipment and special operator expertise.
The fetal cardiac screening examination, as defined by the ISUOG practice guidelines, includes the upper abdomen, the four-chamber view, and outflow tracts (9) (Fig. 2.1). Table 2.1 and Figure 2.1 show the detailed components of the assessment of laterality and of the normal four-chamber view. For more information on the approach to the four-chamber view, schematic drawings, and ultrasound figures, the readers are referred to Chapter 7 in this book.
The left (LVOT) and right (RVOT) outflow tracts are now part of the fetal cardiac screening examination (Fig. 2.1). Evaluation of the LVOT and RVOT requires documentation of vessel size, origin from respective ventricle, integrity of semilunar valves, and anatomic orientation.
Normal anatomy of the LVOT and RVOT can be ascertained by obtaining transverse views from the four-chamber view and into the upper mediastinum. In this sweep, the five-chamber view (LVOT) can be first seen, followed by the RVOT, the three-vessel view (3V), and then the three-vessel trachea (3VT) view (Fig. 2.1). The ISUOG cardiac screening guidelines state that visualization of the 3V view and the 3VT view is desirable and should be attempted as part of the routine cardiac screening examination, although it may not be technically feasible to obtain in all patients. The approach to the sonographic evaluation of the outflow tracts, including schematic drawings and ultrasound figures, is described in great detail in Chapters 8 and 9.
Although the use of color flow Doppler is not considered mandatory for cardiac screening, the ISUOG guidelines recommend that the examiner become familiar with its use. Furthermore, the guidelines state that adding color flow Doppler to the routine screening examination of the fetal heart is encouraged if the examiner is competent with its use. Color flow Doppler may facilitate imaging of various cardiac structures as well as highlighting abnormal blood flow patterns. Color flow Doppler may also be valuable in some difficult scanning conditions, such as obese patients. Chapter 12 presents a detailed review on color flow Doppler in fetal cardiac imaging.
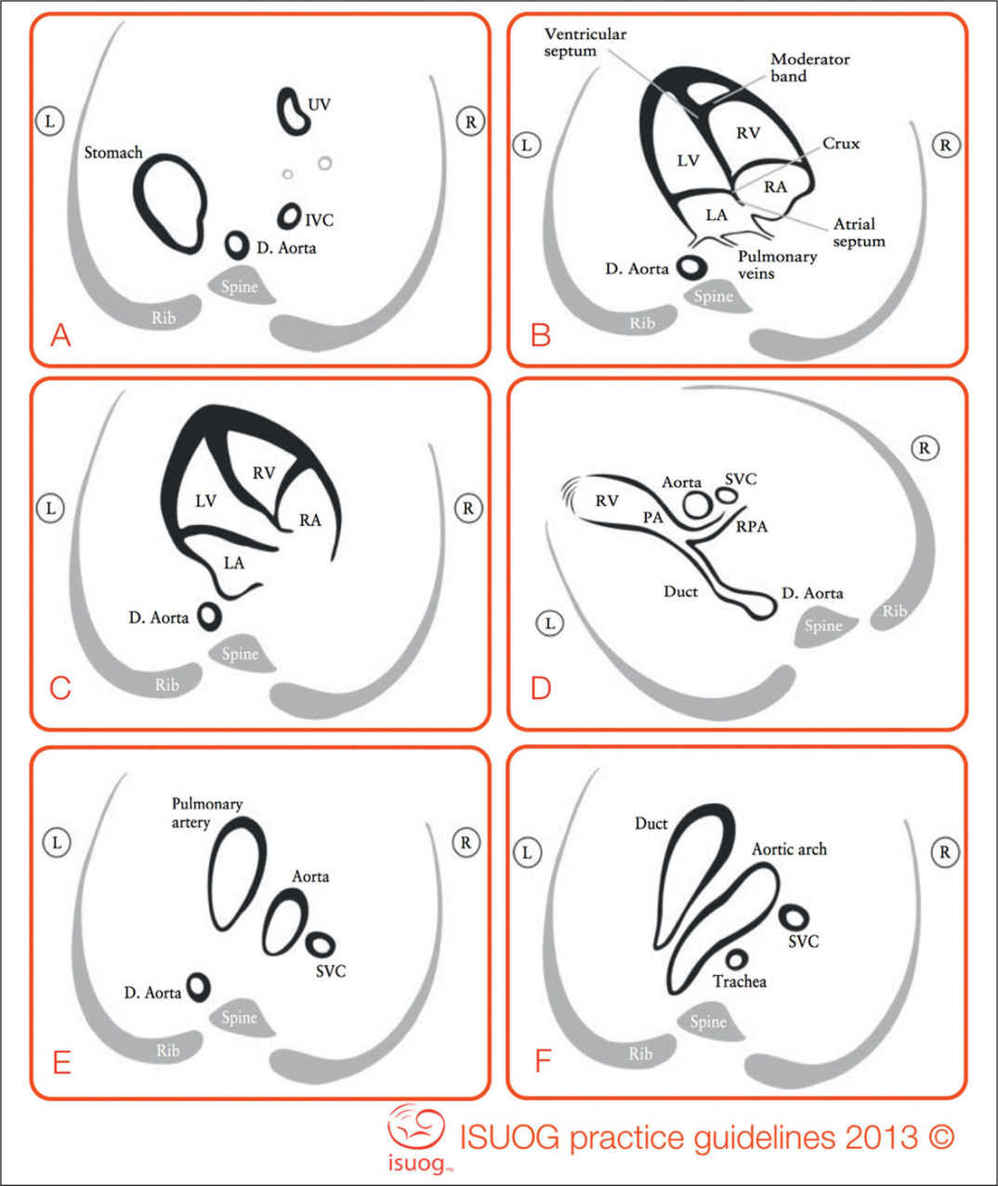
Figure 2.1: Selected views of fetal cardiac screening as recommended by the International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) (9). (A) abdominal situs, (B) four-chamber view, (C) left ventricular outflow tract view, (D) right ventricular outflow tract view, (E) three-vessel view, and (F) three-vessel-trachea view. D. Aorta, descending aorta; Duct, ductus arteriosus; IVC, inferior vena cava; L, left; LA, left atrium; LV, left ventricle; PA, pulmonary artery; RA, right atrium; RPA, right pulmonary artery; RV, right ventricle; R, right; SVC, superior vena cava; UV, umbilical vein. (Modified from International Society of Ultrasound in Obstetrics and Gynecology, Carvalho JS, Allan LD, et al. ISUOG Practice Guidelines (updated): sonographic screening examination of the fetal heart.Ultrasound Obstet Gynecol. 2013;41:348–359, with permission.)
Assessment of Fetal Situs/Laterality and the Four-Chamber View |
Situs and general aspects | • Fetal laterality (identify right and left sides of fetus) • Stomach and heart on left • Heart occupies a third of thoracic area • Majority of heart in left chest • Cardiac axis (apex) points to left by 45° 1 20° • Four chambers present • Regular cardiac rhythm • No pericardial effusion |
Atrial chambers | • Two atria, approximately equal in size • Foramen ovale flap in left atrium • Atrial septum primum present (near to crux) • Pulmonary veins entering left atrium |
Ventricular chambers | • Two ventricles, approximately equal in size • No ventricular wall hypertrophy • Moderator band at right ventricular apex • Ventricular septum intact (apex to crux) |
Atrioventricular junction and valves | • Intact cardiac crux • Two atrioventricular valves open and move freely • Differential offsetting: tricuspid valve leaflet inserts on ventricular septum closer to cardiac apex than does mitral valve |
Modified from International Society of Ultrasound in Obstetrics and Gynecology, Carvalho JS, Allan LD, et al. ISUOG Practice Guidelines (updated): sonographic screening examination of the fetal heart. Ultrasound Obstet Gynecol. 2013;41:348–359, with permission.
Sonographic Cardiac Screening—Guidelines from the American Institute of Ultrasound in Medicine (AIUM)
The American Institute of Ultrasound in Medicine (AIUM) released the practice guidelines for the performance of the obstetric ultrasound examinations in 2013 (10). These guidelines primarily address the components of the obstetric ultrasound examinations, and thus specify the elements of cardiac screening. In the evaluation of the fetal heart, the AIUM guidelines now list the four-chamber view, the LVOT, and RVOT as required components of the screening ultrasound examination. The AIUM guidelines do not provide details on the specific anatomic approach to the evaluation of the outflow tracts (10).
● PRACTICE GUIDELINES FOR THE PERFORMANCE OF THE FETAL ECHOCARDIOGRAPHY EXAMINATION
The fetal echocardiography examination is performed to provide a comprehensive assessment of the fetal cardiovascular anatomy and function. The fetal echocardiography examination includes a detailed assessment of fetal situs, cardiac axis, cardiac chambers, great vessels, atrioventricular and semilunar valves, systemic and pulmonary venous connections to the heart, and cardiac function and rhythm. Given the complexity of the fetal echocardiography examination, it requires advanced operator expertise and high-resolution equipment with color and pulse Doppler capabilities. Defining the components of the fetal echocardiography examination, its indications, and the qualifications of the personnel performing the examination is thus of significant importance.
Typical components of fetal echocardiography guidelines include an introduction, which lists the collaborating organizations, notes the timing of guidelines development, and provides a definition of the fetal echocardiography examination. A section on personnel qualifications typically follows and lists the required qualifications of physicians and sonographers performing the fetal echocardiography examination and the need for continuing medical education over a specified period. The guidelines also define the indications for the fetal echocardiography examination, which allows for standardization in clinical practice. Components of the fetal echocardiography examination are then defined, to include the required ultrasound gray scale, color, and pulsed Doppler views. Sections on storage of images and clips, documentation of the examination and quality control and safety typically follow and complete the guidelines.
Guidelines from the American Institute of Ultrasound in Medicine (AIUM)
The AIUM published the practice guidelines for the performance of the fetal echocardiography examination in 2013 (11). These guidelines were developed in conjunction with the American College of Obstetricians and Gynecologists, the Society of Maternal Fetal Medicine, and the American Society of Echocardiography (ASE) (11). These practice guidelines were also endorsed by the American College of Radiology (11). In these guidelines, the qualifications and responsibilities of personnel performing the fetal echocardiography examination are listed, and these state that appropriately trained obstetricians, maternal-fetal medicine specialists, pediatric cardiologists, and radiologists with special expertise in fetal imaging and who have acquired appropriate knowledge base and skills (outlined by AIUM and ASE) may perform fetal echocardiography.
The AIUM guidelines further state that a request, originated by a physician or other appropriately licensed health care provider in the field, must be available before the fetal echocardiography examination is performed. The AIUM guidelines require that clinical information is provided at the time of the examination request to allow for an understanding of the study indication and should be consistent with relevant legal and local health care facility requirements.
The fetal echocardiography examination is traditionally performed between 18 and 22 weeks of gestational age. The AIUM guidelines acknowledge that some forms of congenital heart disease may be recognized during the early stages of pregnancy, and the readers should refer to Chapter 16 and various sections within this book to learn more about fetal cardiac imaging in the first and early second trimesters of pregnancy. Furthermore, steps for the optimization of the fetal echocardiography examination are reviewed in detail in Chapter 11. The guidelines state that a fetal echocardiogram typically involves a sequential segmental analysis of three basic areas that include the atria, ventricles, and great arteries and their connections. A segmental analysis includes an initial assessment of fetal right/left orientation, followed by an assessment of the segments and their relationship as listed in Table 2.2 and shown in Figures 2.2 to 2.4. Tables 2.3 and 2.4 list the required gray scale and color Doppler views respectively. Documentation of the fetal heart rhythm should be performed by pulse Doppler or M-mode sonography. Any signs of cardiomegaly, atrioventricular valve regurgitation, and hydrops fetalis should be noted, and any abnormal function, if suspected, would require quantitative assessment, including fractional shortening, ventricular strain, and a myocardial performance index. The reader is referred to Chapter 14 in this book for a more comprehensive presentation of cardiac function. Documentation of the fetal echocardiography examination should be performed by real time imaging with acquisition of recording or digital video clips and still images when appropriate.
Guidelines from the Association for European Paediatric Cardiology (AEPC)
The Association for European Paediatric Cardiology (AEPC) provided recommendations for the practice of fetal cardiology in Europe in 2004 (12). These recommendations were provided specifically for the pediatric cardiologist. They are comprehensive and include sections on aims of service and basic requirements such as space, staff, and counseling for prenatal diagnosis of cardiac disease (12). Volume requirements to maintain an adequate level of service are also listed and include 250 to 500 normal studies each year with approximately 50 abnormal cases (12). Maternal, familial, and fetal indications for the fetal echocardiography examination are listed. Details of the components of the complete fetal echocardiography study are also provided. The reader is encouraged to refer to Reference (12) for more details. This document also includes a section on training in fetal cardiology with the required basic knowledge and teaching schedule (12).
Visceral/abdominal situs | • Stomach position • Cardiac apex position |
Atria | • Situs • Systemic and pulmonary venous connections • Venous anatomy • Atrial anatomy (including septum) |
Ventricles | • Position • Atrial connections • Ventricular anatomy (including septum) • Relative and absolute size • Function • Pericardium |
Great arteries (aorta, main and branch pulmonary arteries, and ductus arteriosus) | • Position relative to the trachea • Ventricular connections • Vessel size, patency, and flow (both velocity and direction) |
In addition to a segmental analysis, the following connections should be evaluated | • Atrioventricular junction: anatomy, size, and function of atrioventricular (e.g., mitral and tricuspid) valves • Ventriculoarterial junction: anatomy, size, and function of semilunar (e.g., aortic and pulmonary) valves, including assessment of both the subpulmonary and subaortic regions |
Modified from American Institute of Ultrasound in Medicine. AIUM practice guideline for the performance of fetal echocardiography. J Ultrasound Med. 2013;32:1067–1082, with permission.
Consensus Statement on Fetal Echocardiography from the International Society of Ultrasound in Obstetrics and Gynecology (ISUOG)
The International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) assembled in 2006 a task force to develop a standard description of what constitutes a fetal echocardiogram (13). This consensus document included topics on timing and indications for fetal echocardiography, definition of what constitutes a fetal echocardiogram, description of imaging modalities for fetal echocardiography, the importance of multidisciplinary collaboration and documentation of diagnostic findings and conclusions (13). The reader is encouraged to review Reference (13) for more details.
● CONCLUSIONS
In this chapter, consensus guidelines on fetal cardiac screening and fetal echocardiography are presented. In general, there is good agreement between various guidelines both in cardiac screening and in the components of fetal echocardiography. It is important to note that screening for cardiac malformations in the low-risk population currently includes, as a minimum, views of the four-chamber and outflow tracts. Although not specified in the AIUM screening guidelines, the authors believe that the three-vessel trachea view is a relatively easy plane to obtain and provides significant information on the anatomic relationship of the outflow tracts, more so than the individual LVOT and RVOT planes provide.
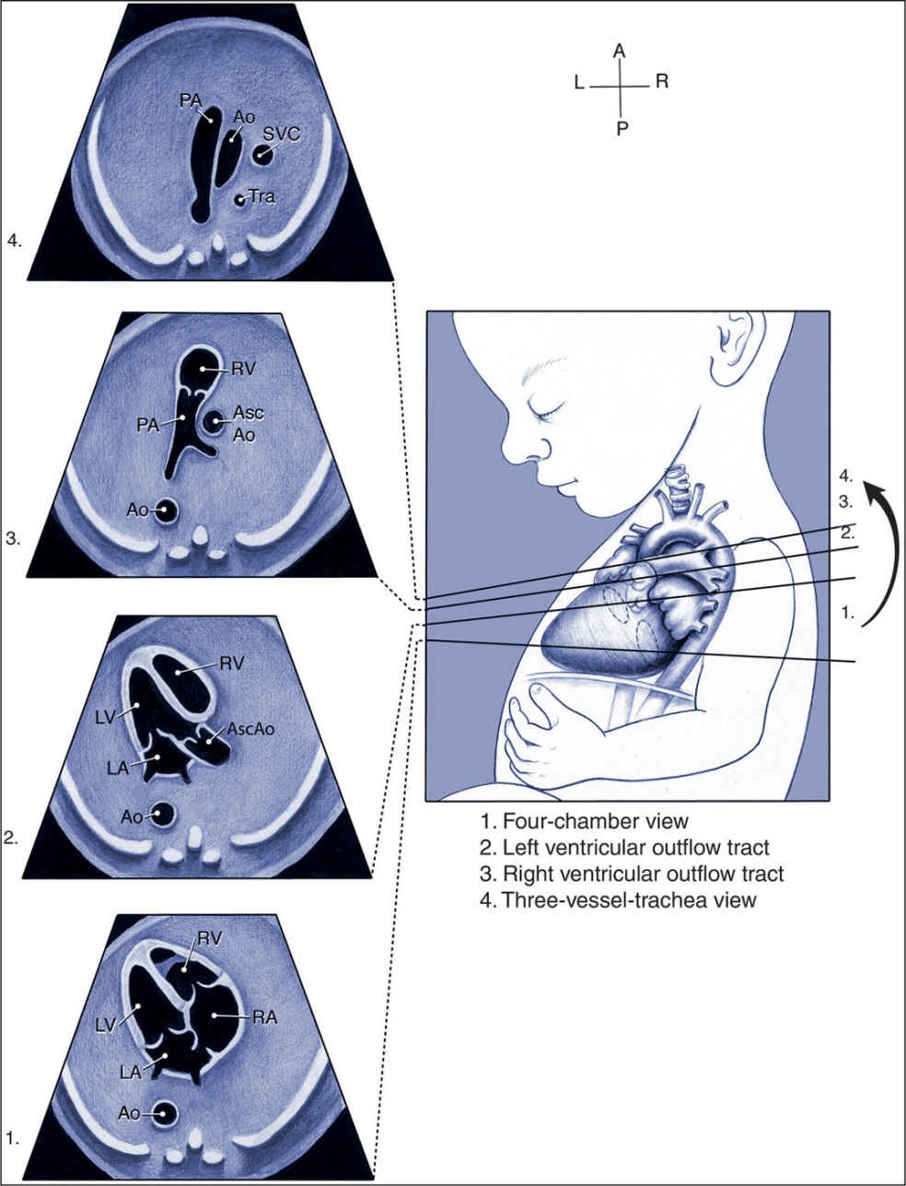
Figure 2.2: Standardized transverse scanning planes for fetal echocardiography as recommended in the Guidelines of the American Institute of Ultrasound in Medicine (AIUM) (11), and include an evaluation of the four-chamber view (1), arterial outflow tracts (2 and 3), and the three-vessel-trachea view (4). Ao, descending aorta; Asc Ao, ascending aorta; LA, left atrium; LV, left ventricle; PA, pulmonary artery; RA, right atrium; RV, right ventricle; and Tra, trachea. (From American Institute of Ultrasound in Medicine. AIUM practice guideline for the performance of fetal echocardiography. J Ultrasound Med. 2013;32:1067–1082, with permission.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


