Vascular Access
Jed G. Nuchtern
Department of Surgery, Baylor College of Medicine, Texas Children’s Hospital, Houston, Texas 77030.
Vascular access can be an extremely challenging aspect of pediatric surgical practice. Technical improvements both in access devices and in aids to catheter insertion have improved the safety and efficiency of device placement in a broad spectrum of patients. As the ease of placement has increased, so have the indications for vascular access. Thus, central venous catheterization has become a standard approach over peripheral venous cutdown for urgent vascular access in hospitalized patients with poor superficial veins. Central venous catheters in various forms have become standard means for hemodialysis, apheresis, and long-term intravenous (IV) antibiotics, in addition to the standard indications of total parenteral nutrition (TPN), central venous pressure monitoring, and chemotherapy. This chapter examines the current indications for various forms of vascular access, technical aspects of insertion of these devices, and advantages and potential problems associated with their use.
PERIPHERAL VENOUS ACCESS
Peripheral vein cannulation is the safest and easiest method of venous access. The goal of all indwelling catheters is reliable access that allows for patient movement with the lowest possible risk of dislodgement, infiltration, phlebitis, and infection. Catheter flexibility is inversely related to the risk of thrombosis and infiltration, and the surface characteristics strongly influence the rate of infection and thrombosis. PEU-Vialon catheters appear to be superior to other materials in preventing phlebitis and infiltration (1,2) and comparable in terms of rate of infection. The vast majority of peripheral catheters are placed by the over-the-needle approach, with the remainder inserted directly into the vein after a cutdown is performed.
Indications
Peripheral vein cannulation is the preferred method of vascular access in all patients, assuming that no specific indication for central venous catheterization is present. Peripheral IVs normally last from 2 to 4 days in a typical toddler, can handle twice maintenance fluid volumes for prolonged periods, and are compatible with multiple medications and dilute parenteral nutrition. A patient with multiple, adequate-appearing peripheral veins can receive 10 to 14 days of IV therapy via peripheral IV without significant difficulty.
Technical Aspects
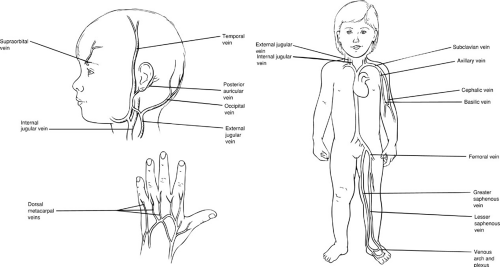
The dorsal veins of the hands and feet are the first choice for peripheral cannulation. The basilic, cephalic, and median cubital veins in the antecubital fossa are highly accessible, but it may be preferable to preserve these sites for phlebotomy or as access for peripherally inserted central catheters. The greater saphenous vein at the ankle or knee is a reasonable size even in a small child and has constant enough anatomy to be cannulated, even if it is not palpable. A scalp vein is useful in small to moderate-size infants. Although the external jugular vein is normally relatively easy to cannulate, it can be very difficult to immobilize these catheters, and they are often displaced shortly after insertion (Fig. 104-1).
Palpation or visualization of peripheral veins may be facilitated by application of tourniquets, dependent positioning, local heat application, and transillumination. The cannula should be carefully matched to the size of the vessel.
Peripheral venous cutdown is a useful technique for emergent or urgent venous access when insertion of a central line is impractical or impossible. The obvious disadvantage is the permanent scarring following the procedure and the short-lived nature of most IVs placed by this technique. For a greater saphenous vein cutdown, a transverse incision is made just proximal to the medial malleolus of
the tibia. The vein is dissected out, and proximal and distal ligatures are placed but not tied down. Applying traction to the proximal ligature, a small venotomy is made on the anterior surface of the vein. The cannula is then passed directly into the vessel, a maneuver that can be facilitated with the use of a small plastic vein pick. The ligatures are tied down, and the hub of the catheter is securely sutured to the skin.
the tibia. The vein is dissected out, and proximal and distal ligatures are placed but not tied down. Applying traction to the proximal ligature, a small venotomy is made on the anterior surface of the vein. The cannula is then passed directly into the vessel, a maneuver that can be facilitated with the use of a small plastic vein pick. The ligatures are tied down, and the hub of the catheter is securely sutured to the skin.
Advantages and Disadvantages
The main advantages of peripheral venous access include technical ease of insertion, safety, and low incidence of sepsis. The disadvantages relate to the risks of phlebitis and thrombosis, as well as simple dislodgement from the vein. The final common pathway of thrombosis and displacement from the vein is extravasation of the infusate, with the potential for skin and tissue necrosis either through hyperosmolar shock, through direct toxic injury, or by induction of vasoconstriction with ischemic injury. Reducing the osmolarity and volume of the infusate decreases the incidence of these problems, but it will also limit the ability to provide adequate parenteral nutrition through this route. Elevation of the extremity is the first line of therapy for an IV infiltrate. Application of heat is no longer recommended because it can accelerate the process of tissue injury from entrapped medications (3). Hyaluronidase (Wydase, Wyeth-Ayerst, Philadelphia, PA) is useful in the treatment of almost all infiltrates and can be particularly helpful in infants. By breaking down the interstitial substrate, it facilitates more rapid reabsorption of chemical irritants and decreases fluid pressure within the tissues. The standard treatment is 15 U, given subcutaneously in five sites around the infiltration, although giving a portion through the catheter has also been reported to be particularly helpful (4).
Phlebitis is treated by removal of the catheter and application of heat. Antibiotics are administered to all patients with symptoms of sepsis and to those with positive blood cultures, regardless of symptoms. We normally withhold antibiotic therapy in nonbacteremic, immunocompetent infants and children older than 1 month of age unless there is severe associated cellulitis. Persistent sepsis in spite of appropriate antimicrobial therapy should raise the suspicion of suppurative thrombophlebitis, prompting exploration and excision of the vein if pus is found.
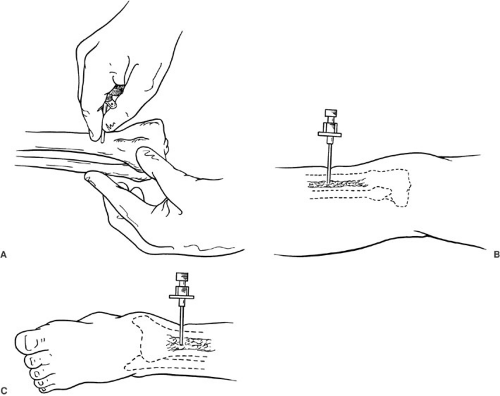 FIGURE 104-2. Intraosseous infusion needle. (A) Technique for proper hand position and placement. (B) Proximal tibial insertion. (C) Distal tibial insertion. |
Rather than having a strict policy regarding the frequency of site changes for peripheral IVs, nursing units should have precise standards of care for surveillance of catheter sites and dressing changes. A site change should occur at the earliest sign of occlusion or infiltration.
INTRAOSSEOUS ACCESS
Indications
The technique of intraosseous infusion was used extensively in the 1930s and 1940s, but decreased in popularity substantially after the development of biocompatible IV catheters. Currently, this technique is limited to life-threatening situations when other rapid techniques have failed. Indications include cardiopulmonary arrest, burns, life- or function-threatening status epilepticus, and shock due to trauma, sepsis, or dehydration. In the tibias and femurs of infants and children, fluid infused into the intramedullary space ultimately drains into the systemic venous circulation. Clinical studies in adults and cadaver experiments suggest that red marrow does not need to be
present within the space for successful intraosseous infusion. The rigid bone matrix acts as a noncollapsible vein that remains easily accessible even during severe hypovolemia and circulatory arrest (5). The tibia and femur have the additional advantage of being physically remote from the anatomic regions of interest during advanced life support procedures. Intraosseous catheters have been used successfully for administration of fluids, blood products, and a variety of medications. Marrow aspirates obtained prior to fluid infusion can be used to determine venous blood gases, chemistry, hemoglobin, as well as type and cross and blood culture samples. The few absolute contraindications include osteoporosis, osteogenesis imperfecta, and an ipsilateral fractured extremity.
present within the space for successful intraosseous infusion. The rigid bone matrix acts as a noncollapsible vein that remains easily accessible even during severe hypovolemia and circulatory arrest (5). The tibia and femur have the additional advantage of being physically remote from the anatomic regions of interest during advanced life support procedures. Intraosseous catheters have been used successfully for administration of fluids, blood products, and a variety of medications. Marrow aspirates obtained prior to fluid infusion can be used to determine venous blood gases, chemistry, hemoglobin, as well as type and cross and blood culture samples. The few absolute contraindications include osteoporosis, osteogenesis imperfecta, and an ipsilateral fractured extremity.
Technical Aspects
The proximal tibia is the best site for insertion of an intraosseous needle, followed by the distal tibia and the femur (Fig. 104-2). A 16- to 18-gauge, disposable, bone marrow aspiration needle is the ideal equipment, although a similar gauge IV cannula can be used under emergency or field conditions. The needle is inserted through the skin, at a perpendicular angle, 1 to 2 cm distal and just medial to the tibial tuberosity and advanced through the bone using a boring or screwing motion (6). There is normally a distinct loss of resistance as the needle enters the marrow space. Intramedullary placement is confirmed by aspiration of marrow contents and easy infusion of fluid. Secure fixation with tape is mandatory to avoid complications.
Advantages and Disadvantages
Intraosseous catheters are the fastest, most reliable means for obtaining emergency vascular access in infants and children.
The risk of serious complications of intraosseous catheters is very low. The more common complications include infiltration of fluid into the subperiosteal and subcutaneous tissues, and leakage at the infusion site. Localized cellulitis, with occasional formation of subcutaneous abscesses, and the more worrisome problem of osteomyelitis are both seen in less than 1% of collected series (5,7). Given that the risk of these complications increases with
duration of intraosseous access, it is important to obtain peripheral or central access as soon as the patient has been stabilized and volume resuscitated.
duration of intraosseous access, it is important to obtain peripheral or central access as soon as the patient has been stabilized and volume resuscitated.
PERIPHERALLY INSERTED CENTRAL VENOUS CATHETERS
Indications
Since the mid-1990s, there has been a huge expansion in the use of peripherally inserted central venous catheters (PICCs) for intermediate-term vascular access. These are small Silastic catheters, ranging in size from 2 to 7 French, which are inserted in a peripheral vein and passed into a central location. Ideally, they combine the ease and safety of insertion of peripheral IVs with the relative permanence and versatility of central lines. These catheters have had the highest impact on the neonatal population, particularly the premature or small-for-gestational-age infant who weighs less than 1,500 g. The limitations of peripheral access (e.g., phlebitis, subcutaneous fluid extravasation, skin slough, restricted use of high-osmolarity solutions, short-term patency) and the complications of surgically placed central lines (e.g., sepsis, pneumothorax, pericardial effusion, superior vena cava thrombosis) have been especially difficult in this age group. In 1982, Dolcourt and Bose (8) reported successful use of Silastic PICCs in 15 neonates, with a mean catheter longevity of 24.8 ± 15.9 days and no catheter sepsis, thrombophlebitis, or caval obstruction. This compares favorably with a study (9) documenting that peripheral IV catheters remained functional for a mean of 33 hours in neonates of similar weight and gestational age. Larger series have demonstrated comparable rates of catheter-related sepsis between PICCs and central venous catheters (10). Success in the neonatal population spurred expanded use of these catheters in children and adolescents. In children with perforated appendicitis, osteomyelitis, meningitis, and immunocompromised patients with opportunistic infections, PICC lines can be an ideal means for administration of antibiotic or antiviral therapy, either in the hospital or at home.
Technical Aspects
The most common sites for placement of PICC lines are the antecubital and superficial saphenous veins. Successful placement via a scalp vein has been reported in infants (11). Ultrasound and fluoroscopy can be helpful for localizing a vein and threading the catheter into the vena cava, respectively (12). Using a modified Seldinger technique, a venipuncture is performed and the guide wire is passed centrally. After a confirmatory chest radiograph or fluoroscopy, the dilator/introducer is passed over the wire and the wire is withdrawn. The wire is then used as a guide to cut the catheter itself to the appropriate length. With a stiffening stylet in place, the catheter is passed through the introducer and the sheath is carefully split and withdrawn. An occlusive dressing is placed, and chest radiography confirms the proper position of the catheter at the junction of the superior vena cava and the right atrium. Even though the catheter is radioopaque, the tip can be difficult to visualize because of its small caliber; thus, it may be necessary to fill the catheter with radioopaque contrast material. As with other systems, attention to a standard protocol for insertion and care is critical for long-term success. Directions supplied with commercial kits are helpful and should be reviewed before attempting catheter placement.
Advantages and Disadvantages
When they are inserted using proper technique, PICCs have the potential to be a safe, cost-effective alternative to standard central venous catheters. Because they can be inserted at the bedside with local anesthetic in the neonatal or pediatric intensive care unit, the cost and risk of a trip to the operating theater are avoided. There are no randomized controlled trials of PICC lines versus central venous catheters in children. In the only such adult trial, PICCs actually had a higher rate of complications (thrombophlebitis and difficulty of insertion) and were more costly than subclavian central lines in hospitalized patients requiring TPN.
Nonrandomized series reporting PICC use in infants and children have demonstrated excellent results overall (13,14,15), with a greater than 90% rate of successful insertion. The main drawback of this device appears to be a high incidence of mechanical problems, especially with difficulty passing the catheter and occlusion [as high as 28% in one series (16)], related to small caliber, relatively long length, and delicate consistency of the Silastic catheter. Although the rate of infection is comparable to subclavian central lines, removal for occlusion, dislodgement, and thrombophlebitis is definitely more common with PICCs (17).
Based on the available data, PICCs are a reasonable choice for central access in infants and children who require 2 to 3 weeks of therapy. Patients who are likely to require more than 4 weeks of therapy may be better served by a tunneled “permanent” central venous catheter because many of the complications of PICCs are related to duration of use.
CENTRAL VENOUS ACCESS
Indications
Central venous catheterization is indicated for (1) secure delivery of drugs to the central circulation, (2) administration of parenteral alimentation in high concentration, (3) central venous pressure monitoring, (4) rapid infusion
of large volumes of fluids or blood products in very small patients whose peripheral veins may not withstand high flow rates, (5) alternative route for parenteral fluid or drugs in patients for whom peripheral venous access is no longer possible, (6) long-term continuous or intermittent access for blood sampling or therapy, (7) hemodialysis, and (8) apheresis for cellular therapy and plasmapheresis.
of large volumes of fluids or blood products in very small patients whose peripheral veins may not withstand high flow rates, (5) alternative route for parenteral fluid or drugs in patients for whom peripheral venous access is no longer possible, (6) long-term continuous or intermittent access for blood sampling or therapy, (7) hemodialysis, and (8) apheresis for cellular therapy and plasmapheresis.
Technical Considerations
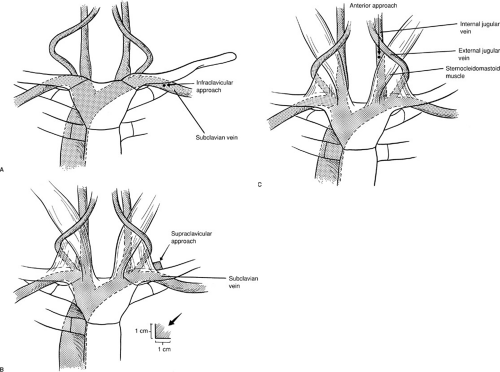
Landmarks for subclavian and internal jugular vein catheter insertion are indicated in Fig. 104-3. In children younger than 5 years of age, the subclavian vein is located closer to the superior border of the clavicle, and the needle insertion angle should be adjusted accordingly. Once the needle has been inserted and the angle established, the course should not be changed unless the needle is completely withdrawn for danger of lacerating the vein, artery, or other mediastinal structures, such as the phrenic nerve.
Advantages and Disadvantages
With the advent of subclavian central venous access (18), central venous catheters were available for use in place
of peripheral catheters in older children and adults. They also enabled the administration of hyperosmolar solutions, making TPN possible and practical. Once the technical aspects of insertion are mastered, central venous catheters are relatively easy to insert rapidly, with an acceptably low complication rate. Central venous catheter longevity is also much greater than that of peripheral lines, and they are better tolerated by patients, who are left unencumbered by immobilization boards and dressings, thereby retaining use of their hands and feet. Central venous catheters also have the advantage of enabling periodic blood sampling without the necessity of separate peripheral venipunctures. In 1986, Newman and colleagues (19) demonstrated the efficacy and safety of percutaneous central venous catheters in a prospective study comparing the subclavian or jugular approach with peripheral venous cutdown in the pediatric population. They concluded that percutaneous central intravenous catheterization is the method of choice for venous access other than routine short-term situations. In current practice, PICC lines have replaced percutaneous central venous catheters in many intermediate-term applications, although they are not appropriate in emergencies.
of peripheral catheters in older children and adults. They also enabled the administration of hyperosmolar solutions, making TPN possible and practical. Once the technical aspects of insertion are mastered, central venous catheters are relatively easy to insert rapidly, with an acceptably low complication rate. Central venous catheter longevity is also much greater than that of peripheral lines, and they are better tolerated by patients, who are left unencumbered by immobilization boards and dressings, thereby retaining use of their hands and feet. Central venous catheters also have the advantage of enabling periodic blood sampling without the necessity of separate peripheral venipunctures. In 1986, Newman and colleagues (19) demonstrated the efficacy and safety of percutaneous central venous catheters in a prospective study comparing the subclavian or jugular approach with peripheral venous cutdown in the pediatric population. They concluded that percutaneous central intravenous catheterization is the method of choice for venous access other than routine short-term situations. In current practice, PICC lines have replaced percutaneous central venous catheters in many intermediate-term applications, although they are not appropriate in emergencies.
The main disadvantage of central venous catheter placement is that complications are generally more serious than those associated with peripheral venous access. Only physicians well experienced in the techniques of subclavian and internal jugular venipuncture should insert central venous catheters. Except in an emergency, central venous catheters should be inserted only under planned circumstances with sufficient help available and with careful attention to aseptic technique, including full barrier precautions. Possible complications at the time of catheter insertion are discussed in the concluding section.
BROVIAC-TYPE SILASTIC CATHETERS: PERMANENT CENTRAL VENOUS CATHETERS
Indications
The first generation of indwelling central venous catheters was made of polyvinyl chloride and was relatively stiff and thrombogenic. These catheters were associated with a number of mechanical and septic complications. In 1973, Broviac and colleagues (20) introduced the Silastic catheter, an indwelling silicone rubber catheter that can remain in place for extended periods. The Silastic catheter is much more flexible and inert and is associated with fewer complications than polyvinyl catheters with respect to mechanical occlusion, venous perforation, and infection. Commercial versions of these catheters have evolved to the widely used permanent central venous catheter (PCVC) (21). These catheters are manufactured from radioopaque soft silicone rubber, in varying calibers and lengths, and have a small Dacron felt cuff 30 cm from the external end. The cuff allows fibrous ingrowth, which serves to anchor the catheter and to act as a barrier to infection. Indications for PCVC use in children include any condition requiring long-term venous access for the administration of fluids, antibiotics, antineoplastic drugs, TPN, and blood products, or the need for frequent blood sampling. Modified versions of these catheters, generally with larger, duel lumens and a 2- to 3-centimeter offset between the ends of the
lumens, are uses for therapies requiring high throughput without recirculation, such as hemodialysis and apheresis. Appropriate candidates for PCVC placement include in-hospital patients, such as infants recovering from gastroschisis or necrotizing enterocolitis, or outpatients, such as children with neoplastic disease requiring chemotherapy or patients with short bowel syndrome on home parenteral nutrition.
lumens, are uses for therapies requiring high throughput without recirculation, such as hemodialysis and apheresis. Appropriate candidates for PCVC placement include in-hospital patients, such as infants recovering from gastroschisis or necrotizing enterocolitis, or outpatients, such as children with neoplastic disease requiring chemotherapy or patients with short bowel syndrome on home parenteral nutrition.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree