Orthopedic Principles for Trauma
Paul D. Sponseller
Orthopaedic Surgery, Johns Hopkins University, Johns Hopkins Hospital, Baltimore, Maryland 21287.
Sprains, fractures, and dislocations are among the most common injuries in children (1). In 30% to 50% of patients with multiple traumatic injuries, an extremity injury is present. Residual morbidity after the accident is often due to orthopedic and neurologic injuries (2,3). This chapter provides an update on current principles of skeletal trauma.
SKELETAL DEVELOPMENT AND NOMENCLATURE
The long bones have several distinct anatomic regions. The diaphysis is the shaft area. The metaphysis is the region that widens or expands toward the bone end. The physis, or growth plate, is present in the immature skeleton. The epiphysis is the end of the long bone. Initially, the epiphysis is made of cartilage; however, as maturation proceeds, a secondary ossification center develops within it. As maturity progresses, the epiphysis changes from cartilage to bone.
The periosteum is the outer connective tissue envelope of the bone. This layer is better developed in children than adults. It provides for growth in width. Periosteal bone deposition also plays an important role in fracture healing.
PATHOPHYSIOLOGY AND BIOMECHANICS OF FRACTURES
The immature skeleton is biologically and mechanically different from the adult skeleton. As bone matures, it undergoes changes in porosity, collagen fiber composition, and mineral content. The elasticity of bone in children allows incomplete fractures and plastic deformation to occur, such as buckle and greenstick fractures. Immature bone can also absorb more energy before breaking (4).
The angulation of a child’s bone after fracture will often remodel with growth. Because of this prolific biologic activity, most childhood fractures can be treated without surgical intervention. Fractures that occur in the metaphyseal region of the bone in young children remodel most. Although angular deviation can improve, rotational malalignment after a fracture does not effectively correct itself.
PATIENT EVALUATION
Clinical Examination
The orthopedic areas of concern in the polytrauma patient are the spine, the pelvis, and the extremities. Much can be learned from palpation of the skeletal system. Assessment is made of the ability of the patient to voluntarily move the arms and legs. The neurovascular examination of an injured extremity should be carefully documented. Rectal tone should be documented in any patient with a suspected spinal column injury.
Radiography
The polytrauma patient should usually have spine, chest, and pelvis radiographs (5). The upper cervical spine, especially at the C1 and C2 junction, is the most important area to evaluate on lateral radiograph (6).
Radiography of the extremities should be undertaken in the presence of obvious deformity, pain on palpation, swelling, or concern about retained foreign debris. If a long bone is found to have a fracture, the radiographs should include the entire long bone, not just the area of injury. Multilevel injury to a single long bone does occur. If tenderness or signs of trauma along the spinal column are seen, spine radiographs should be included in the evaluation. In seat-belt injuries, radiographs of the thoracolumbar spine should be taken because of the association with flexion-distraction injuries of the spine (see the “Thoracic and Lumbar Spine” section).
GENERAL FRACTURE CARE
The basic tenet of fracture care is to provide immobilization of the bone so soft tissue and bony healing can occur. This can be accomplished by a number of means. Splints are an effective way to immobilize an extremity if there is concern about applying a rigid circular dressing (i.e., a cast) in the face of significant soft tissue swelling. Casting has been the time-honored method of treatment, but it requires skill.
More invasive means of fracture care have evolved for fractures that cannot be adequately aligned in a satisfactory position within a cast. Traction can be effective, but is seldom used as definitive treatment due to prolonged recumbency time. Percutaneous pin fixation in conjunction with a cast has proved useful in pediatric fractures, especially elbow injuries. External fixation is more suitable for children than adults. In the past, external fixation was used mainly in open fractures. It is now being used for some closed pediatric fractures as well. Internal fixation using screws, plates, and intramedullary rods has given the orthopedist more options.
GROWTH PLATE INJURY
About 15% of children’s fractures involve the physis (3). Inherent to the physis can be problematic because the physis constitutes a weak area. It is through this zone that a fracture can occur and propagate. An injury to the epiphysis and physis is an injury to the area of endochondral bone formation and can produce long-term sequelae. Premature complete closure of the growth plate leads to a discrepancy in the length of an arm or a leg. A partial growth arrest can lead to a discrepancy in length and can also create an angular deformity.
A classification system that is commonly used in North America for growth plate fractures is the Salter-Harris system (7):
Type I: The epiphysis separates from the metaphysis, with low likelihood of later growth disturbance.
Type II: The epiphysis separates with a metaphyseal fracture fragment—the most common type of physeal fracture.
Type III: Intraarticular type of fracture through the epiphysis and the physis.
Type IV: Intraarticular fracture that involves epiphysis, physis, and metaphysis. These typically require anatomic reduction of the fracture to guard against growth disturbance.
Type V: Crush injury to the physis. These can be difficult to diagnose at the time of injury.
Treatment consists of accurately reducing these fragments by manipulation with or without percutaneous fixation. If this is unsuccessful, open reduction with internal fixation is indicated.
OPEN FRACTURES
Open fractures typically result from a greater magnitude of energy than closed fractures and have more associated soft tissue damage. The initial treatment consists of irrigation and debridement of the wound. This decreases the bacterial count in the wound. Necrotic tissue and particulate debris are removed. Bone stabilization promotes soft tissue recovery. For fracture healing to occur, a healthy soft tissue envelope must first be present. A classification system is widely used for open fractures. The Gustilo and Anderson classification is as follows:
Type I (grade I): Open fracture in a clean wound less than 1 cm in length.
Type II (grade II): Open fracture with a laceration more than 1 cm long.
Type III (grade III): Open fracture with extensive soft tissue injury. Typically, the wounds are greater than 10 cm in length and often require flap coverage. Open, severely comminuted fractures, as well as farm injuries are considered grade III injuries, regardless of wound size. Traumatic amputations are also grade III injuries (8).
Follow-up irrigation and debridement should be done every 24 to 48 hours until the wound is clean and free of necrotic debris. Wound closure can be accomplished using immediate or delayed primary closure, skin grafting, or soft tissue flaps.
Antibiotic coverage consists of a first-generation cephalosporin for type I and II injuries. In a type III injury, an aminoglycoside is usually added. Farm injuries are grade III injuries because of the contamination with barnyard and soil organisms, especially clostridia. In these cases, penicillin is added to the cephalosporin and aminoglycoside antibiotic regime.
In most clinical scenarios, antibiotic coverage continues for 48 hours after each debridement and after the final wound closure. Because patients with type III injuries often return for two or three debridements, antibiotic treatment often lasts for 1 week to 10 days.
COMPARTMENT SYNDROME
A compartment syndrome occurs when the tissue pressure in a closed fascial space reaches a critical level, creating tissue ischemia. If normal tissue pressure is not restored, permanent loss of function ensues. Compartment syndromes are most frequently seen in the leg, but can occur in the arm, hand, foot, thigh, shoulder, and buttocks. Compartment syndromes are seen with fractures (including open
fractures), crush injuries, bums, hemorrhage into a closed space, and after revascularization of ischemic limbs.
fractures), crush injuries, bums, hemorrhage into a closed space, and after revascularization of ischemic limbs.
Signs and symptoms of a compartment syndrome include pain out of proportion to the clinical setting (the earliest symptom), pain on passive stretch of the involved compartment’s muscles, a tense muscle compartment on palpation, and hypesthesia (a late finding). A patient can have normal intact distal pulses in the face of a compartment syndrome because the major arteries traversing the compartment have a pressure gradient sufficient to allow flow through the compartment, thereby preserving the peripheral pulse (Fig. 27-1) (9). Therefore, the peripheral pulse and digital circulation are poor indicators of a compartment syndrome.
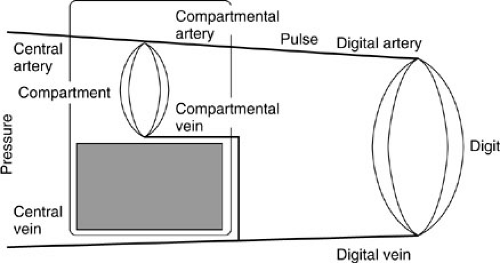 FIGURE 27-1. Pathophysiology of a compartment syndrome. (Adapted from Matsen FA. Pathophysiology of compartment syndromes. Instr Course Lect 1989;38:463–472.) |
Tissue pressure monitoring allows early diagnosis of compartment syndrome. Tissue pressure can be obtained by using a needle or catheter connected by a fluid column to a pressure transducer or manometer. Normal resting muscle compartment pressures are 0 to 5 mm Hg. There is disagreement about what absolute pressure constitutes a compartment syndrome; however, the threshold for considering decompression in an acute compartment syndrome is approximately 40 mm Hg. The patient’s hemodynamic status should also be considered. If the compartment pressure is within 10 to 30 mm Hg of the diastolic blood pressure, perfusion may be inadequate (9,10).
Diagnosis is made by clinical examination and compartment pressures. In the awake patient, both excessive pain at rest and pain on passive stretch of the involved muscles are the predominant features. This is the time the diagnosis should be made, not when hypesthesia develops. Compartment pressures are a helpful adjunct. In a patient with an altered mental status, the tissue pressures are often the only reliable guideline for diagnosis.
Treatment of acute compartment syndrome is fasciotomy. Irreversible tissue injury occurs within 6 hours. The involved extremity should be placed at heart level and not elevated. This allows the delivery of the best possible perfusion pressure to the tissues. In acute compartment syndrome, subcutaneous fasciotomy through limited skin incisions should be avoided because the skin acts as a noncompliant envelope (11). In lower compartment syndromes, the two-incision technique of fasciotomy is preferred (12).
FRACTURE CARE IN THE POLYTRAUMA PATIENT
Traditionally, closed fracture treatment in children has been common. It is becoming clear, however, that early operative stabilization of fractures is also of benefit in children (2,13). Problems resulting from immobilization in bed are refocusing the discussion about operative fracture intervention for some of these children (14).
HEAD INJURY
Head injuries in children pose special problems in fracture care. Increased muscle tone and agitation can make controlling long bone fracture alignment difficult. Cast treatment is not without risk because of the potential for skin ulceration under the cast. Because many of these children regain the ability to walk, long bone malunions can be a source of morbidity and should be avoided. These issues have led to the use of internal or external fixation in patients with injuries resulting in muscle spasticity (15).
Care should be taken in the acute phase of head injury management to prevent joint and muscle contractures (16). Both range-of-motion therapy and splinting are necessary to avoid deformity. The muscular spasticity can be strong enough to break splints and to cause skin ulcerations.
VASCULAR INJURY
Vascular injury associated with a closed fracture is uncommon in children; however, it can occur with essentially any fracture (11). At the moment of fracture, the bone ends become widely displaced, stretching the accompanying soft tissues, including the neurovascular bundle. This can create
intimal injury or direct laceration and can lead to entrapment of the vessels between the fracture fragments.
intimal injury or direct laceration and can lead to entrapment of the vessels between the fracture fragments.
Several fractures often cause vascular insult. These include the supracondylar humerus fracture with brachial artery injury, fractures around the knee with distal superficial femoral or popliteal vessel injury, and open fractures in general. Sternoclavicular separations can injure the innominate and subclavian vessels.
CERVICAL SPINE
Neck injuries in children are usually the result of significant trauma. They differ from adult neck injuries in the following ways:
Most children’s cervical spine injuries occur in the upper three vertebrae, due to the relatively large head. In the child older than age 11, the injuries are more common in the lower cervical spine.
Most cervical spine injuries in young children are due to birth trauma, motor vehicle accidents (as passengers), or shaken baby syndrome. Children struck as pedestrians infrequently sustain cervical fractures. In older children, sports, falls from heights, and gunshot wounds are significant causes.
Growth and Development
Some stages of growth simulate traumatic abnormalities. The first cervical vertebra or atlas develops from three ossification centers: one anteriorly in the midline, which may not appear until late in the first year, and one on each side posterolaterally to complete the ring. The ring may not fuse posteriorly for several years.
The axis or second cervical vertebra contains four centers. Its unique feature is the peglike odontoid process (also called the dens). It serves to stabilize C1 and C2 during rotation, flexion, and extension. There is a physis at the bottom of the odontoid at the junction with the body of C2 (19). This usually fuses by 6 years of age. This physis can be mistaken for a fracture. There is also a small ossicle at the tip of the odontoid, the ossiculum terminale, which fuses by 12 years of age.
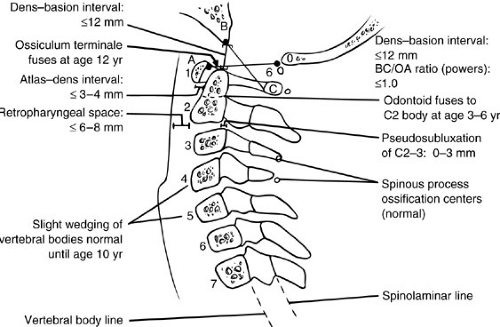
The odontoid is stabilized against the ring of C1 by the transverse ligament. The normal space between C1 and the dens in children is up to 4 mm in flexion (Fig. 27-2). The space inside the ring of C-1 can be conceptualized in thirds: one-third of the diameter is occupied by the spinal cord, one-third is occupied by the odontoid, and one-third is free space.
The vertebral bodies in childhood are more wedge shaped than in adults. This may give the appearance of a compression injury, but is simply due to the lack of complete ossification of cartilage.
Physical Examination and Immediate Care
In the trauma setting, a spine injury should always be presumed to be present until proven otherwise. The neck should be palpated for tenderness or swelling. Motor function can be assessed by looking for movement at each major joint, and sensation should be tested in each limb segment. Head injuries or facial lacerations should increase the level of suspicion of cervical spine injuries (20). Neck guarding, stiffness, or holding the head still with the hands
can all be signs of an injury to the spine in an awake patient. Pulmonary arrest may also be a sign of spine trauma. Patients should be kept immobilized until radiographs show no signs of injury. This should include a backboard for the entire spine, and sandbags and tape for the head. Hard cervical collars are often available, but they permit some degree of motion and are best supplemented with sandbags and tape. Foam cervical collars have no value and provide a false sense of immobilization.
can all be signs of an injury to the spine in an awake patient. Pulmonary arrest may also be a sign of spine trauma. Patients should be kept immobilized until radiographs show no signs of injury. This should include a backboard for the entire spine, and sandbags and tape for the head. Hard cervical collars are often available, but they permit some degree of motion and are best supplemented with sandbags and tape. Foam cervical collars have no value and provide a false sense of immobilization.
The head in a young child is relatively large, so placing it flat on a backboard forces the neck into relative flexion (21). It is therefore recommended that adult backboards be modified by either a cutout for the head or an extra mattress beneath the trunk. This applies in children 8 years of age and younger. If a child is injured with an athletic helmet on, it should be left on during transport. This avoids the additional movement of removing it. The face mask should be removed to allow for airway control.
If intubation is needed, avoid flexing and extending the neck. Theoretically, nasotracheal intubation can be performed with less movement than orotracheal, but the orotracheal route is easier to carry out.
Radiography
By Advanced Trauma Life Support (ATLS) guidelines, all polytrauma patients should have AP and lateral cervical spine films. Particular concern regarding neck radiographs exist in the presence of neck pain, trauma to the head or face, or an unconscious patient. The lateral film is by far more important. Anteroposterior and open mouth views may provide additional information. Oblique views rarely add additional information owing to the rarity of subaxial subluxations in young children and the availability of better imaging modalities.
The film should be scrutinized for all seven cervical vertebrae (Fig. 27-2). The alignment of the posterior vertebral bodies and the spinal laminae should form a smooth curve, with no stepoffs. The retropharyngeal space (in front of the cervical spine) should be less than 7 mm at C2, and the retrotracheal space less than 14 mm at C6. These figures may be increased somewhat by inspiration, but if greatly increased, may signal bleeding from an injury. The occipitoatlantal interval should also be scrutinized. A gap of more than 10 mm between the basion and the dens or a forward shift of the skull may signal injury at this level. Even when one spinal injury is seen, the rest of the spine should be carefully examined because multiple fractures occur in more than 15% of all spinal injuries.
Children also may have spinal cord injury without radiographic abnormality (SCIWORA) (22). SCIWORA may be related to the elasticity of the spinal column when subjected to distraction forces. The spine tolerates four times as much stretch as does the spinal cord before failure occurs. Other theories about the cause of SCIWORA include cord ischemia, cord compression by a hematoma, and compression by an epiphyseal cartilage end-plate fracture that is not seen on plain radiographs. These injuries account for 5% of all spinal cord injuries in children. An end-plate disruption can leave the spinal column unstable, so patients with SCIWORA should be immobilized until further workup is completed. A clinical examination of the cervical spine identifying whether pain exists with flexion and extension or with rotational movement should be performed after the cervical spine has been cleared radiographically. If pain exists with movement, immobilization should be maintained and other imaging studies obtained (flexion/extension films or neck cervical spine films. Likewise, the unconscious patient should be kept with the neck immobilized even if the screening cervical spine film is negative.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree