Background
Since 1995 uterine artery embolization has been described as an alternative for hysterectomy in patients with symptomatic fibroids. Many studies including several randomized controlled trials established uterine artery embolization as a valuable treatment. These randomized controlled trials reported outcomes in terms of health-related quality of life, clinical outcomes, efficacy, and cost-effectiveness after 1, 2, and 5 years of follow-up.
Objective
The purpose of this study was to compare clinical outcome and health-related quality of life 10 years after uterine artery embolization or hysterectomy in the treatment of heavy menstrual bleeding caused by uterine fibroids in a randomized controlled trial.
Study Design
In all, 28 Dutch hospitals recruited patients with symptomatic uterine fibroids who were eligible for hysterectomy. Patients were 1:1 randomly assigned to uterine artery embolization or hysterectomy. The outcomes assessed at 10 years postintervention were reintervention rates, health-related quality of life, and patient satisfaction, which were obtained through validated questionnaires. Study outcomes were analyzed according to original treatment assignment (intention to treat).
Results
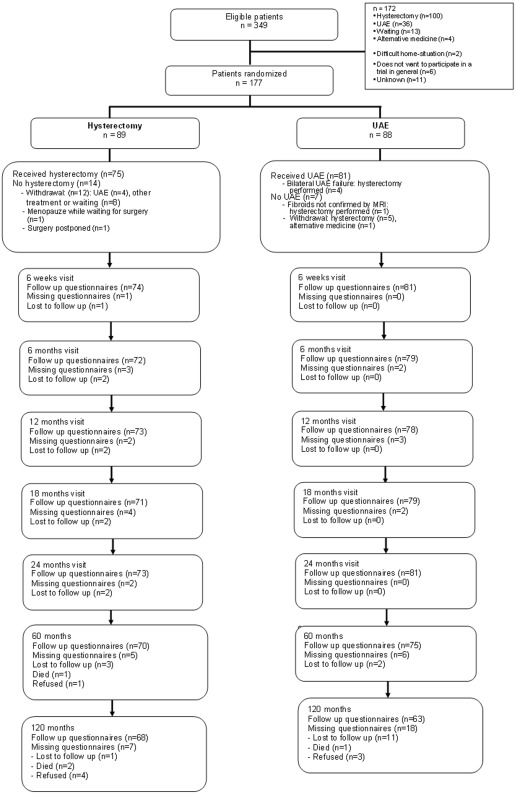
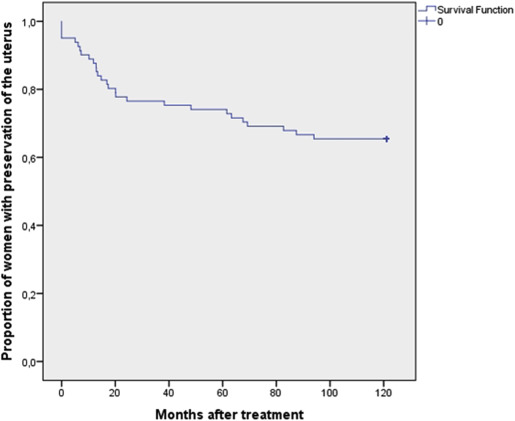
A total of 177 patients were randomized from 2002 through 2004. Eventually 81 uterine artery embolization and 75 hysterectomy patients underwent the allocated treatment shortly after randomization. The remaining patients withdrew from the trial. The 10-year questionnaire was mailed when the last included patient had been treated 10 years earlier. The mean duration of follow-up was 133 months (SD 8.58) accompanied by a mean age of 57 years (SD 4.53). Questionnaires were received from 131 of 156 patients (84%). Ten years after treatment, 5 patients underwent secondary hysterectomy resulting in a total of 28 of 81 (35%) (24/77 [31%] after successful uterine artery embolization). Secondary hysterectomies were performed for persisting symptoms in all cases but 1 (for prolapse). After the initial treatment health-related quality of life improved significantly. After 10 years, generic health-related quality of life remained stable, without differences between both groups. The urogenital distress inventory and the defecation distress inventory showed a decrease in both groups, probably related to increasing age, without significant differences between study arms. Satisfaction in both groups remained comparable. The majority of patients declared being (very) satisfied about the received treatment: 78% of the uterine artery embolization group vs 87% in the hysterectomy group.
Conclusion
In about two thirds of uterine artery embolization–treated patients with symptomatic uterine fibroids a hysterectomy can be avoided. Health-related quality of life 10 years after uterine artery embolization or hysterectomy remained comparably stable. Uterine artery embolization is a well-documented and less invasive alternative to hysterectomy for symptomatic uterine fibroids on which eligible patients should be counseled.
Introduction
Uterine artery embolization (UAE) was first described for the treatment of symptomatic uterine fibroids in 1995. Since then UAE was established as being a valuable treatment alternative for hysterectomy in many studies including several randomized controlled trials. These randomized controlled trials compared hysterectomy or myomectomy with UAE and found similar results in terms of health-related quality of life (HRQOL) after 1, 2, and 5 years of follow-up.
Earlier we reported on the results from the randomized EMMY (Embolization vs Hysterectomy) trial. These results contained data through 5 years after index procedure. We compared clinical results, HRQOL outcomes, and menopausal symptoms between embolization and hysterectomy.
In the present study, we analyzed these results again, now 10 years after treatment.
Materials and Methods
Study design
The full methods of this trial have been described earlier. Here we describe the condensed methods. The EMMY study is a multicenter, randomized controlled trial, conducted in The Netherlands from 2002 through 2004. Five university hospitals and 29 general hospitals recruited patients. Patients with symptomatic uterine fibroids who visited the gynecological outpatient clinic were asked to participate in the trial. The following inclusion criteria had to be met: (1) premenopausal status, (2) diagnosis of uterine fibroids by ultrasonography, (3) heavy menstrual bleeding as the predominant symptom, (4) no other treatment option than hysterectomy, and (5) no wish to conceive in the future. The study was approved by the Central Committee Involving Human Subjects followed by approval from local ethics committees of the participating hospitals. After informed consent had been obtained, patients were randomly (1:1) allocated to UAE or hysterectomy.
Procedures
As described earlier UAE and hysterectomy were performed according to protocol and professional standards. See Table 1 for type of hysterectomy and UAE.
| UAE N = 88 | Hysterectomy N = 89 | |
|---|---|---|
| Age, y | ||
| Mean (SD) | 44.6 (4.8) | 45.4 (4.2) |
| Body mass index, weight [kg]/length [m 2 ] | ||
| Mean (SD) | 26.7 (5.6) | 25.4 (4.0) |
| Parity | ||
| 0 | 30 (34.1) | 20 (22.5) |
| ≥1 | 58 (65.9) | 69 (77.5) |
| Ethnicity | ||
| Black | 24 (27.3) | 20 (22.5) |
| Caucasian | 54 (61.4) | 57 (64.0) |
| Other | 10 (11.4) | 12 (13.5) |
| Marital status | ||
| Single | 16 (18.2) | 13 (14.8) |
| Married | 55 (62.5) | 54 (61.4) |
| Together but living apart | 5 (5.7) | 4 (4.5) |
| Divorced | 12 (13.6) | 15 (17.0) |
| Widow | 0 (0) | 2 (2.3) |
| Employment status | ||
| Employed | 68 (77.3) | 69 (78.4) |
| Unemployed | 20 (22.7) | 19 (21.6) |
| Smoking status | ||
| Current smoker | 21 (23.9) | 23 (25.8) |
| Former smoker | 11 (12.5) | 14 (15.7) |
| Nonsmoker | 56 (63.6) | 52 (58.4) |
| Highest educational level | ||
| Elementary school | 3 (3.4) | 6 (6.9) |
| Lower vocational, lower secondary school | 29 (33.0) | 32 (36.8) |
| Intermediate and higher vocational, higher secondary school | 26 (29.5) | 27 (31.0) |
| College/university | 28 (31.8) | 22 (25.3) |
| Other | 2 (2.3) | 0 (0) |
| Previous treatment | ||
| None | 11 (12.5) | 15 (16.9) |
| Hormonal | 59 (67.0) | 59 (66.3) |
| Nonsteroidal antiinflammatory drugs/tranexamic acid | 45 (51.1) | 41 (46.1) |
| Iron supplement/blood transfusion | 50 (56.8) | 52 (58.4) |
| Surgical procedures | 17 (19.3) | 11 (12.4) |
| Symptoms | ||
| Menorrhagia | 88 (100) | 89 (100) |
| Dysmenorrhea | 47 (53.4) | 50 (56.2) |
| Pain (not during menstruation) | 15 (17.0) | 14 (15.7) |
| Anemia | 43 (48.9) | 42 (47.2) |
| Pressure symptoms | 23 (26.1) | 25 (28.1) |
| Other symptoms | 6 (6.8) | 11 (12.4) |
| Duration of symptoms, mo | ||
| Median (range) | 24 (3–250) | 24 (4–240) |
| No. of fibroids | ||
| Median (range) | 2 (1–20) | 2 (1–9) |
| Uterine volume, cm 3 | ||
| Median (range) | 321 (31–3005) | 313 (58–3617) |
| Fibroid volume–dominant fibroid, cm 3 | ||
| Median (range) | 59 (1–673) | 87 (4–1641) |
| Type of UAE | ||
| Target embolization | ||
| Left uterine artery | 65 | – |
| Right uterine artery | 59 | – |
| Selective embolization | ||
| Left uterine artery | 8 | – |
| Right uterine artery | 12 | – |
| Type of hysterectomy | (N = 4) | |
| Abdominal hysterectomy | 2 | 63 |
| Vaginal hysterectomy | 1 | 8 |
| Vaginal hysterectomy with morcellation | 1 | 1 |
| LH with morcellation | – | 2 |
| LAVH | – | 1 |
Sample size and endpoints of the study
The primary endpoint of the 2-year EMMY trial was elimination of heavy/abnormal menstrual bleeding in at least 75% of patients who were therefore spared a hysterectomy. To reject the null hypothesis that UAE and hysterectomy are not clinically equivalent, at least 2 × 60 (= 120) analyzable patients had to be included. Endpoints after 10 years were reinterventions, quality of life, urinary and defecation function, menopausal symptoms, menstrual characteristics, and satisfaction with the received treatment.
Study measures
During the first 2-year follow-up patients received a total of 6 questionnaires. After 5 and 10 years, an additional questionnaire was sent to all participants of the trial. The 10-year questionnaire was mailed when the last included patient had reached 10 years of follow-up. As a result, the questionnaire was returned after a median of 11 years of follow-up (133 months; SD 8.58). Nonresponders were contacted by telephone. All questionnaires were similar except for the 5- and 10-year follow-up questionnaires, which were condensed versions of the original 6 questionnaires to optimize the response rate. The 10-year questionnaire evaluated the following subjects: additional interventions between 5-10 years of follow-up, HRQOL, urinary and defecation function, menopausal symptoms, menstrual characteristics (bleeding symptoms since UAE or no symptoms due to successful UAE or menopause), and satisfaction.
Generic HRQOL
Health status and HRQOL was evaluated using the Medical Outcome Study Short Form (SF)-36. The SF-36 generates 2 summary scores: The physical component summary (PCS) and the mental component summary (MCS). The scores range from 0-100 and were validated for the Dutch population. Higher scores represent better physical or mental functioning.
Urinary function and defecation
Urinary and defecation functioning was evaluated using the validated urogenital distress inventory (UDI) and the defecation distress inventory (DDI).
The UDI was used to investigate urinary symptoms. The UDI score ranges from 1-100. Higher scores represent worse functioning. The same applies to the DDI, which was used to score defecation symptoms. Patients were asked to rate the overall quality of urinary and stool function: very good, good, not good, nor bad, fairly bad, bad, or very bad. Furthermore, an inquiry was made if patients used pads for urinary incontinence or laxatives.
Menopause
Menopausal symptoms were evaluated by the Kupperman score as modified by Wiklund et al. Scores range from 0-51, where higher scores represent more serious menopausal symptoms.
Satisfaction
We inquired whether the patients would recommend the primary treatment to a friend and whether or not they would indeed have chosen the assigned treatment again if they would have the opportunity to do so. Finally, patients were asked to indicate how satisfied they were with the received treatment on a 7-point Likert scale: very satisfied, satisfied, fairly satisfied, not satisfied/not unsatisfied, fairly unsatisfied, unsatisfied, or very unsatisfied.
Statistical analysis
Statistical software (SPSS, Version 20.0; IBM Corp, Armonk, NY) was used for analyses. Study outcomes were analyzed according to original treatment assignment (intention to treat). Comparison of differences in categorical data was assessed with the χ 2 test (or Fisher exact test, if appropriate). Differences in numeric data were assessed by the unpaired Student t test. Predictors for secondary hysterectomy were analyzed by binary logistic regression. Whenever univariate analyses within baseline characteristics ( Appendix ) yielded a P value < .1 these were included for binary logistic regression.
Differences in HRQOL between the groups were assessed with the unpaired Student t tests. Repeated measurement analysis was used to evaluate longitudinal differences (MCS, PCS, UDI, DDI, and Wiklund scores) between the treatment strategies with time as a repeated factor (covariance structure: unstructured).
Multiple linear regression analyses were performed for baseline characteristics ( Appendix ) that yielded P values < .1 in univariate analyses to evaluate the impact of these characteristics on the MCS, PCS, UDI, and DDI change scores at 10 years compared to baseline.
P < .05 (2-sided) was considered statistically significant in all analyses.
Materials and Methods
Study design
The full methods of this trial have been described earlier. Here we describe the condensed methods. The EMMY study is a multicenter, randomized controlled trial, conducted in The Netherlands from 2002 through 2004. Five university hospitals and 29 general hospitals recruited patients. Patients with symptomatic uterine fibroids who visited the gynecological outpatient clinic were asked to participate in the trial. The following inclusion criteria had to be met: (1) premenopausal status, (2) diagnosis of uterine fibroids by ultrasonography, (3) heavy menstrual bleeding as the predominant symptom, (4) no other treatment option than hysterectomy, and (5) no wish to conceive in the future. The study was approved by the Central Committee Involving Human Subjects followed by approval from local ethics committees of the participating hospitals. After informed consent had been obtained, patients were randomly (1:1) allocated to UAE or hysterectomy.
Procedures
As described earlier UAE and hysterectomy were performed according to protocol and professional standards. See Table 1 for type of hysterectomy and UAE.
| UAE N = 88 | Hysterectomy N = 89 | |
|---|---|---|
| Age, y | ||
| Mean (SD) | 44.6 (4.8) | 45.4 (4.2) |
| Body mass index, weight [kg]/length [m 2 ] | ||
| Mean (SD) | 26.7 (5.6) | 25.4 (4.0) |
| Parity | ||
| 0 | 30 (34.1) | 20 (22.5) |
| ≥1 | 58 (65.9) | 69 (77.5) |
| Ethnicity | ||
| Black | 24 (27.3) | 20 (22.5) |
| Caucasian | 54 (61.4) | 57 (64.0) |
| Other | 10 (11.4) | 12 (13.5) |
| Marital status | ||
| Single | 16 (18.2) | 13 (14.8) |
| Married | 55 (62.5) | 54 (61.4) |
| Together but living apart | 5 (5.7) | 4 (4.5) |
| Divorced | 12 (13.6) | 15 (17.0) |
| Widow | 0 (0) | 2 (2.3) |
| Employment status | ||
| Employed | 68 (77.3) | 69 (78.4) |
| Unemployed | 20 (22.7) | 19 (21.6) |
| Smoking status | ||
| Current smoker | 21 (23.9) | 23 (25.8) |
| Former smoker | 11 (12.5) | 14 (15.7) |
| Nonsmoker | 56 (63.6) | 52 (58.4) |
| Highest educational level | ||
| Elementary school | 3 (3.4) | 6 (6.9) |
| Lower vocational, lower secondary school | 29 (33.0) | 32 (36.8) |
| Intermediate and higher vocational, higher secondary school | 26 (29.5) | 27 (31.0) |
| College/university | 28 (31.8) | 22 (25.3) |
| Other | 2 (2.3) | 0 (0) |
| Previous treatment | ||
| None | 11 (12.5) | 15 (16.9) |
| Hormonal | 59 (67.0) | 59 (66.3) |
| Nonsteroidal antiinflammatory drugs/tranexamic acid | 45 (51.1) | 41 (46.1) |
| Iron supplement/blood transfusion | 50 (56.8) | 52 (58.4) |
| Surgical procedures | 17 (19.3) | 11 (12.4) |
| Symptoms | ||
| Menorrhagia | 88 (100) | 89 (100) |
| Dysmenorrhea | 47 (53.4) | 50 (56.2) |
| Pain (not during menstruation) | 15 (17.0) | 14 (15.7) |
| Anemia | 43 (48.9) | 42 (47.2) |
| Pressure symptoms | 23 (26.1) | 25 (28.1) |
| Other symptoms | 6 (6.8) | 11 (12.4) |
| Duration of symptoms, mo | ||
| Median (range) | 24 (3–250) | 24 (4–240) |
| No. of fibroids | ||
| Median (range) | 2 (1–20) | 2 (1–9) |
| Uterine volume, cm 3 | ||
| Median (range) | 321 (31–3005) | 313 (58–3617) |
| Fibroid volume–dominant fibroid, cm 3 | ||
| Median (range) | 59 (1–673) | 87 (4–1641) |
| Type of UAE | ||
| Target embolization | ||
| Left uterine artery | 65 | – |
| Right uterine artery | 59 | – |
| Selective embolization | ||
| Left uterine artery | 8 | – |
| Right uterine artery | 12 | – |
| Type of hysterectomy | (N = 4) | |
| Abdominal hysterectomy | 2 | 63 |
| Vaginal hysterectomy | 1 | 8 |
| Vaginal hysterectomy with morcellation | 1 | 1 |
| LH with morcellation | – | 2 |
| LAVH | – | 1 |
Sample size and endpoints of the study
The primary endpoint of the 2-year EMMY trial was elimination of heavy/abnormal menstrual bleeding in at least 75% of patients who were therefore spared a hysterectomy. To reject the null hypothesis that UAE and hysterectomy are not clinically equivalent, at least 2 × 60 (= 120) analyzable patients had to be included. Endpoints after 10 years were reinterventions, quality of life, urinary and defecation function, menopausal symptoms, menstrual characteristics, and satisfaction with the received treatment.
Study measures
During the first 2-year follow-up patients received a total of 6 questionnaires. After 5 and 10 years, an additional questionnaire was sent to all participants of the trial. The 10-year questionnaire was mailed when the last included patient had reached 10 years of follow-up. As a result, the questionnaire was returned after a median of 11 years of follow-up (133 months; SD 8.58). Nonresponders were contacted by telephone. All questionnaires were similar except for the 5- and 10-year follow-up questionnaires, which were condensed versions of the original 6 questionnaires to optimize the response rate. The 10-year questionnaire evaluated the following subjects: additional interventions between 5-10 years of follow-up, HRQOL, urinary and defecation function, menopausal symptoms, menstrual characteristics (bleeding symptoms since UAE or no symptoms due to successful UAE or menopause), and satisfaction.
Generic HRQOL
Health status and HRQOL was evaluated using the Medical Outcome Study Short Form (SF)-36. The SF-36 generates 2 summary scores: The physical component summary (PCS) and the mental component summary (MCS). The scores range from 0-100 and were validated for the Dutch population. Higher scores represent better physical or mental functioning.
Urinary function and defecation
Urinary and defecation functioning was evaluated using the validated urogenital distress inventory (UDI) and the defecation distress inventory (DDI).
The UDI was used to investigate urinary symptoms. The UDI score ranges from 1-100. Higher scores represent worse functioning. The same applies to the DDI, which was used to score defecation symptoms. Patients were asked to rate the overall quality of urinary and stool function: very good, good, not good, nor bad, fairly bad, bad, or very bad. Furthermore, an inquiry was made if patients used pads for urinary incontinence or laxatives.
Menopause
Menopausal symptoms were evaluated by the Kupperman score as modified by Wiklund et al. Scores range from 0-51, where higher scores represent more serious menopausal symptoms.
Satisfaction
We inquired whether the patients would recommend the primary treatment to a friend and whether or not they would indeed have chosen the assigned treatment again if they would have the opportunity to do so. Finally, patients were asked to indicate how satisfied they were with the received treatment on a 7-point Likert scale: very satisfied, satisfied, fairly satisfied, not satisfied/not unsatisfied, fairly unsatisfied, unsatisfied, or very unsatisfied.
Statistical analysis
Statistical software (SPSS, Version 20.0; IBM Corp, Armonk, NY) was used for analyses. Study outcomes were analyzed according to original treatment assignment (intention to treat). Comparison of differences in categorical data was assessed with the χ 2 test (or Fisher exact test, if appropriate). Differences in numeric data were assessed by the unpaired Student t test. Predictors for secondary hysterectomy were analyzed by binary logistic regression. Whenever univariate analyses within baseline characteristics ( Appendix ) yielded a P value < .1 these were included for binary logistic regression.
Differences in HRQOL between the groups were assessed with the unpaired Student t tests. Repeated measurement analysis was used to evaluate longitudinal differences (MCS, PCS, UDI, DDI, and Wiklund scores) between the treatment strategies with time as a repeated factor (covariance structure: unstructured).
Multiple linear regression analyses were performed for baseline characteristics ( Appendix ) that yielded P values < .1 in univariate analyses to evaluate the impact of these characteristics on the MCS, PCS, UDI, and DDI change scores at 10 years compared to baseline.
P < .05 (2-sided) was considered statistically significant in all analyses.
Results
Patients
Enrollment took place from March 2002 through February 2004 in 28 of 34 hospitals in The Netherlands. A total of 75 women vs 81 women received hysterectomy or UAE, respectively. Baseline and procedural characteristics are listed in Table 1 . The patient flow is described in Figure 1 ; 84% of the mailed 10-year questionnaires were returned, with a mean follow-up of 133 months (SD 8.58 for analytical purposes, the median time of 11 years is depicted as a fixed point in time and mentioned hereafter as “10 years”). The remaining 16% consisted of nonresponders due to emigration (n = 3), unknown address (n = 10), refusal to participate (n = 9), or death (n = 3). Of the nonresponders 10 patients underwent UAE without secondary hysterectomy. The median age of all patients responding to the 10-year questionnaire was 56 years (range 45-68).
Clinical outcome already reported
In the first 2 years of follow-up, 19 secondary hysterectomies were performed (23.5%): 4 because of bilateral UAE failure and another 15 because of clinical failure during follow-up. At 2-5 years an additional 4 secondary hysterectomies were performed, because of insufficient improvement of menstrual bleeding symptoms, thus increasing the total secondary hysterectomy rate after 5 years to 28.4%.
Clinical outcome at 10 years
In addition to these 23 secondary hysterectomies, another 5 hysterectomies were required between 5-10 years ( Figure 2 ). This totals 28 (35%) secondary hysterectomies after 10 years. Secondary hysterectomies were performed because of persistent menstrual problems or pain in all cases but 1, which was carried out for prolapse. Per protocol analysis showed that 24 of 77 (31%) patients underwent a secondary hysterectomy after a technically successful UAE, while another 4 patients in the UAE group had a bilateral embolization failure and subsequently had a hysterectomy. Three of the patients who underwent unilateral embolization (30%) had a secondary hysterectomy, all within the first 2 years of follow-up. A total of 10 of 81 (12%) patients underwent unilateral embolization. Of these 10 patients, 3 of 28 (10.7% received a secondary hysterectomy) and 8 of 53 (13.2%) did not.
UAE failure within 10 years of follow-up was associated with a body mass index >25 (odds ratio, 3.29; 95% confidence interval [CI], 1.14–9.55; P = .028) and smoking (odds ratio, 3.24; 95% CI, 1.08–9.68; P = .036) in the multivariate analysis.
An overview of all additional interventions performed within 10 years in the UAE group and hysterectomy group are listed in Table 2 .
| Primary intervention UAE | Secondary intervention | Reason for intervention | Time since primary intervention, mo |
|---|---|---|---|
| Until 2 y | |||
| 1 | Abdominal hysterectomy | Bilateral failure UAE | <1 |
| 2 | Abdominal hysterectomy | Bilateral failure UAE | <1 |
| 3 | Abdominal hysterectomy | Bilateral failure UAE | <1 |
| 4 | Vaginal hysterectomy with morcellation | Bilateral failure UAE | <1 |
| 5–1 | Failed attempt to hysteroscopically remove myoma under general anesthesia | Persistent abdominal pain/myoma nascens | 1 |
| 5–2 | Attempt at hysteroscopic myoma resection: converted to vaginal hysterectomy | Return menorrhagia | 20 |
| 6 | Manual resection myoma under general anesthesia | Discharge, fever, and abdominal pain/myoma nascens | 2 |
| 7 | Abdominal hysterectomy | Menorrhagia and persistent abdominal pain | 5 |
| 8 | Abdominal hysterectomy | Menorrhagia | 6 |
| 9 | Abdominal hysterectomy | Menorrhagia, persistent pain, bulk symptoms | 7 |
| 10 | Abdominal hysterectomy | Menorrhagia | 7 |
| 11 | Abdominal hysterectomy | Persistent abdominal pain and irregular menstruation | 10 |
| 12 | Vaginal hysterectomy | Menorrhagia, persistent pain, and dyspareunia | 12 |
| 13–1 | Diagnostic hysteroscopy with curettage | Post menstrual blood loss | 12 |
| 13–2 | Abdominal hysterectomy | Irregular cycle, pain, and bulk symptoms | 13 |
| 14 | Abdominal hysterectomy | Menorrhagia and bulk symptoms | 13 |
| 15 | Abdominal hysterectomy | Return menorrhagia | 13 |
| 16 | Laparoscopic-assisted vaginal hysterectomy | Menorrhagia | 15 |
| 17 | Abdominal hysterectomy | Menorrhagia | 17 |
| 18 | Vaginal hysterectomy | Menorrhagia | 17 |
| 19 | Abdominal hysterectomy | Menorrhagia | 20 |
| 20 | Abdominal hysterectomy | Menorrhagia | 24 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


