● INTRODUCTION
The sonographic assessment in axial planes of the vessels in the upper fetal thorax was first described in the mid-1980s (1) and early 1990s (2). The value of these axial planes in the comprehensive evaluation of the fetal cardiovascular system became well known and disseminated in the late 1990s (3). Various names, which corresponded to various anatomic levels, were given to these axial and tangential planes in the upper thorax. These axial and tangential planes assess the ascending aorta and aortic arch, the main pulmonary artery and ductal arch, the superior vena cava (SVC), and other neighboring vessels and structures. From inferior to superior, starting cephalad from the five-chamber view, several planes have been described to include the three-vessel view, the ductal arch view, the three-vessel-trachea (3VT) view, the transverse aortic arch view, and the brachiocephalic vein view (3–9). The three-vessel view describes an axial plane that shows the ascending aorta, the main pulmonary artery, and the SVC, at the site where the SVC enters the right atrium (see Fig. 8.4 and Chapter 8). The 3VT view describes, in a slightly oblique axial plane in the upper mediastinum, the transverse main pulmonary artery and ductal arch, the transverse aortic arch and its isthmic region, and the cross sections of the SVC and trachea (Fig. 9.1). This plane is part of the fetal echocardiography examination and is suggested in cardiac screening guidelines (10–12). The authors believe that the 3VT view is a very important plane for the assessment of great vessels and upper venous system, in addition to the neighboring anatomic structures in the upper mediastinum. It is for this reason that we decided to dedicate a full chapter of this book on this topic. In order to better understand the clinical value of this plane, we hereby describe its normal anatomy and include several cardiac abnormalities associated with abnormal 3VT views.
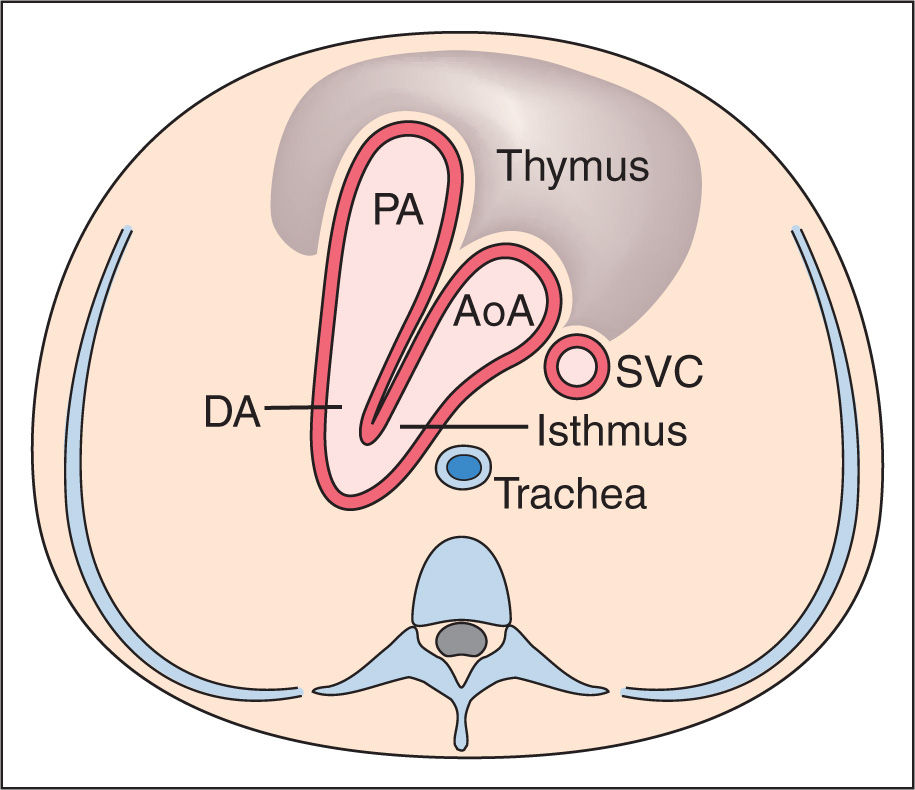
Figure 9.1: Schematic drawing of a cross section of the upper mediastinum at the level of the three-vessel-trachea view. Note that the transverse aortic arch (AoA) and isthmus merge with the pulmonary artery (PA) and ductus arteriosus (DA) into the descending aorta in a “V-shape” configuration. Both vessels point to the left of the trachea, which is found central and anterior to the spine. The superior vena cava (SVC) is anterior to the trachea and on the right of the AoA. The space between the great vessels and the anterior sternal wall is occupied by the thymus.
● SCANNING TECHNIQUE FOR THE THREE-VESSEL-TRACHEA VIEW AND UPPER MEDIASTINUM
The 3VT view is an axial/oblique plane of the upper thorax. Scanning technique for obtaining the 3VT view is as follows:
1. Determine the fetal situs (see Chapter 6).
2. Obtain a four-chamber view of the fetal heart (see Chapter 7).
3. Obtain a three-vessel view by sliding the transducer cranially while maintaining the transverse orientation in the chest (see Chapter 8).
4. From the three-vessel view, the 3VT view can be obtained by slightly angling the transducer caudally, toward the fetal left side (Fig. 8.1), until the fusion of aortic and ductal arches are visualized (Figs. 9.1 to 9.4). In this plane, several great vessel abnormalities can be demonstrated as shown in this chapter.
5. Anterior to the 3VT and behind the anterior chest wall, the thymus is identified as a hypoechoic structure, with often clear lateral borders as compared to the slightly more echogenic neighboring lungs. A higher frequency transducer and/or high-resolution settings allows for a better delineation of the thymus, where measurements can be performed and abnormalities identified.
6. Moving the transducer further cranially and slightly oblique to the left, from the 3VT view, the SVC is noted as it connects with the brachiocephalic vein. The brachiocephalic vein runs from the posterior left upper to the anterior right thorax as it connects with the SVC. In this upper thoracic plane, the great vessels are not seen, as they are inferior in anatomic location.
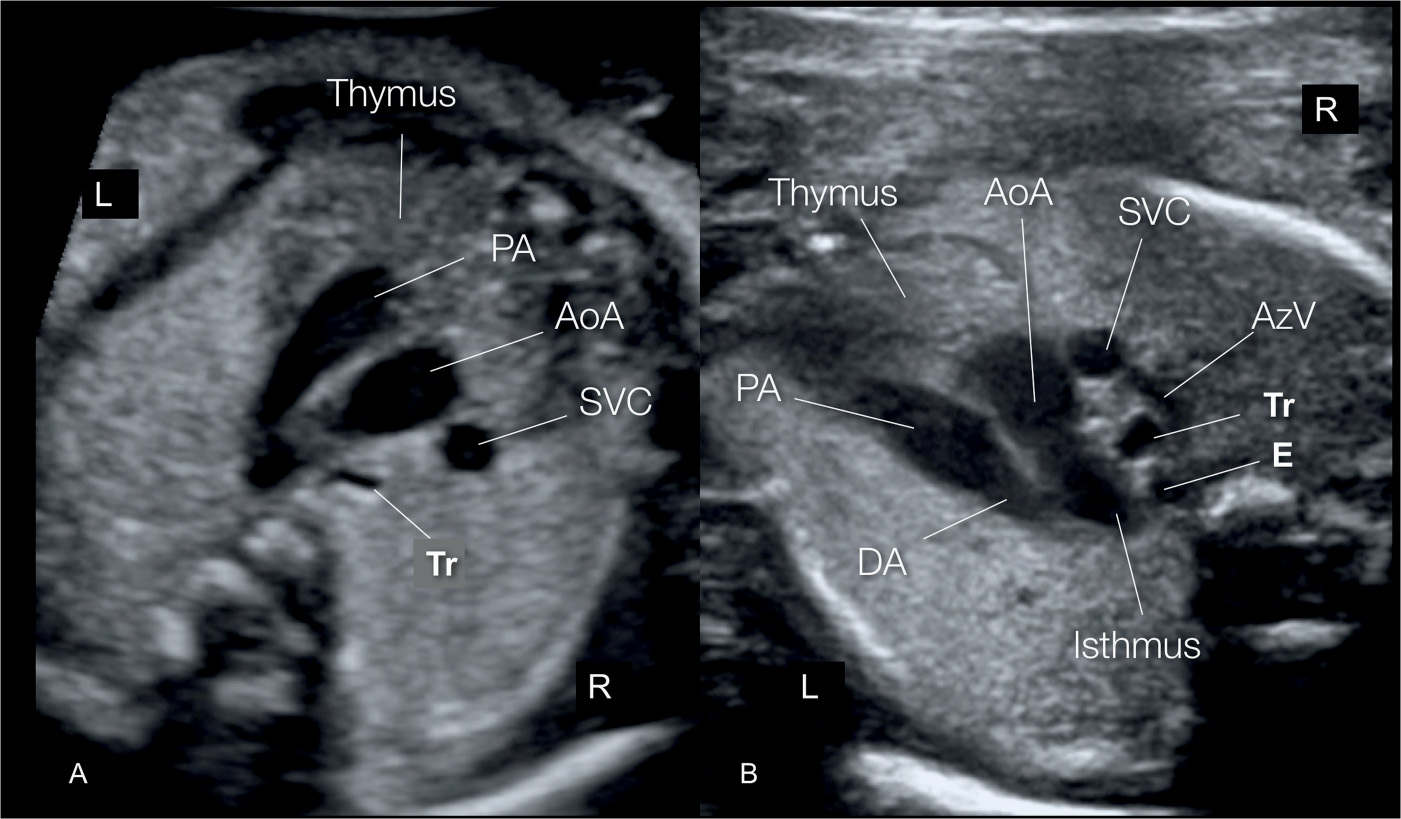
Figure 9.2: Three-vessel-trachea view shown on grayscale ultrasound using a normal transducer (A) and a high-resolution linear transducer (B). Note in A and B the aortic arch (AoA) and ductal arch (DA) merging together with a course to the left of the spine and trachea (Tr). The superior vena cava (SVC) is located to the right of the aortic arch (compare with Fig. 9.1). Note in B the azygos vein draining into the SVC and the esophagus (E) posterior to the Tr. The thymus gland is seen anteriorly. PA, pulmonary artery; L, left; R, right. Compare with Figure 9.5A.
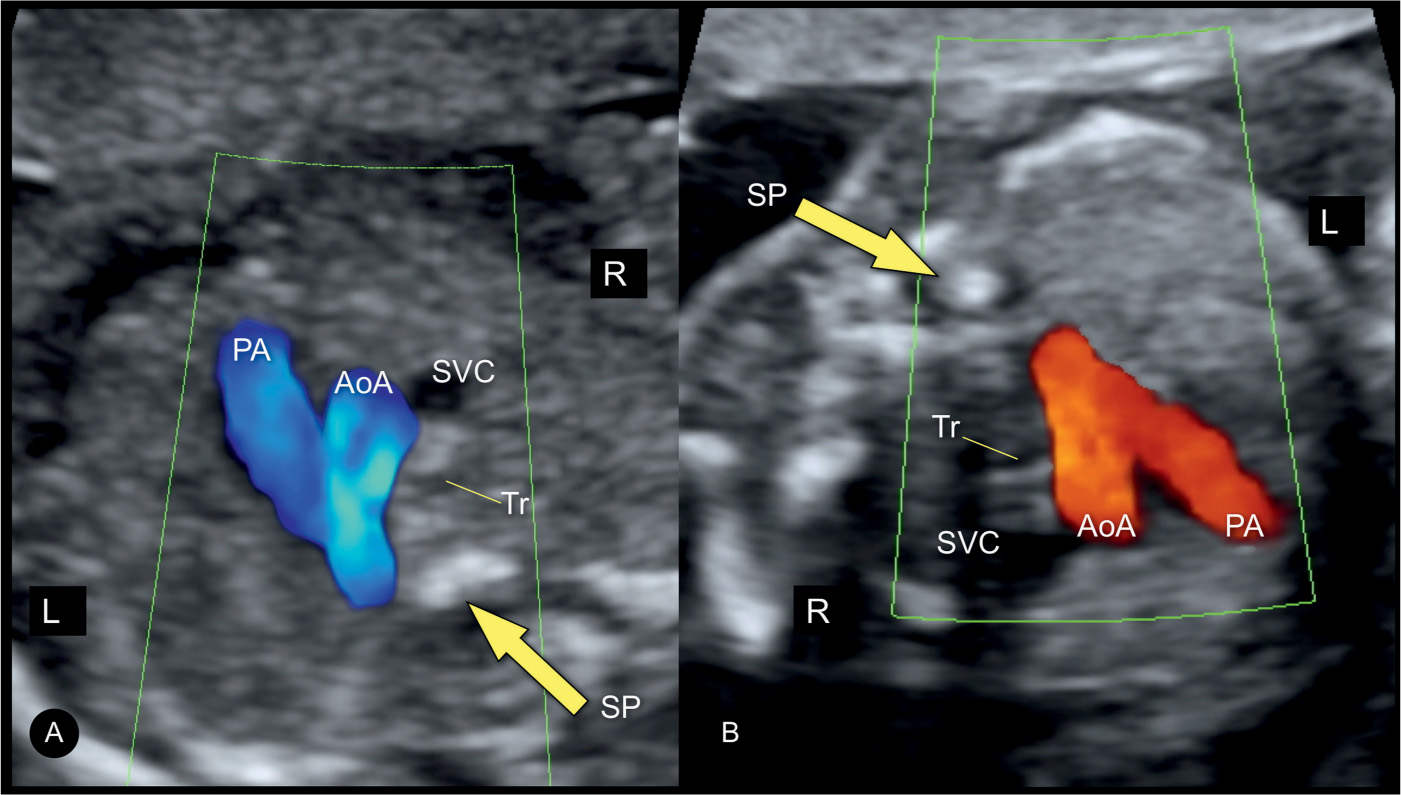
Figure 9.3: Three-vessel-trachea view shown on color Doppler from a ventral (A) or dorsal (B) insonation. Note in A the flow in the great vessels is in blue color and in B in red color, both toward the descending aorta (spine). AoA, aortic arch; PA, pulmonary artery; SP, spine; SVC, superior vena cava; Tr, trachea; L, left; R, right.
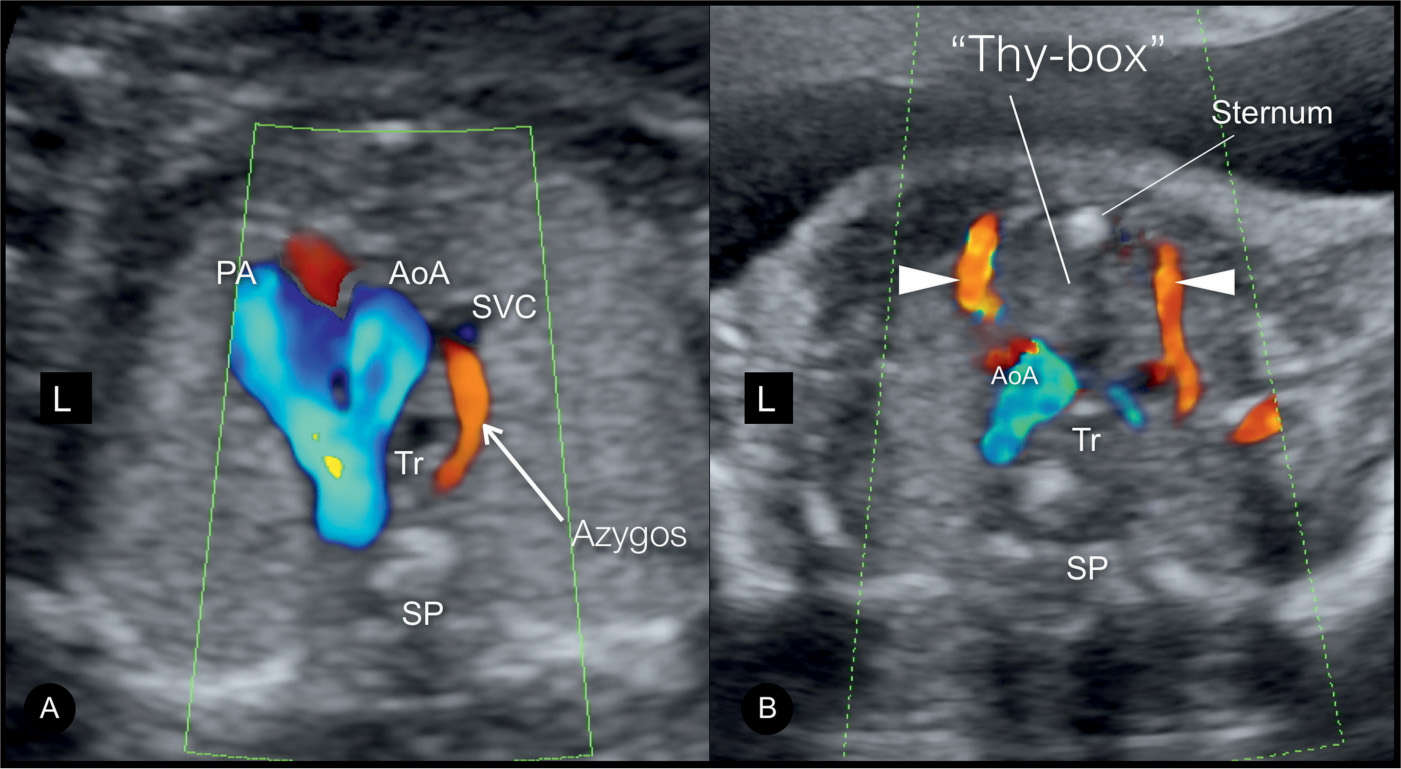
Figure 9.4: Three-vessel-trachea view shown in A with color Doppler in low-velocity preset, demonstrating the azygos vein (AzV) arch draining into the superior vena cava (SVC) (compare with Figs. 9.2 and 10.15). B represents low-velocity color Doppler in a slightly higher plane, demonstrating both mammarian arteries (arrows) bordering the thymus, a view called “thy-box.” AoA, aortic arch; PA, pulmonary artery; SP, spine; Tr, trachea; L, left.
● ASSESSMENT OF THE THREE-VESSEL-TRACHEA VIEW ON GRAY SCALE AND COLOR DOPPLER
Normal Findings in the Three-Vessel-Trachea View
In the 3VT view, the aortic and ductal arches are seen as they merge together into the descending aorta with an acute angle between them (Figs. 9.1 to 9.3). Both arches are located to the left of the spine and trachea, an important anatomic landmark, as no vessel should be seen to the right of the trachea in normal cardiovascular anatomy. Directly anterior to the spine, the trachea is recognized as a circular structure with an echogenic wall and a black lumen (Fig. 9.2).
The SVC is seen in a cross section and is located to the right of the aortic arch (Fig. 9.2). The three vessels have an oblique line orientation with the ductal arch, the largest of the three, assuming a more anterior position; the aortic arch, slightly smaller than the ductal arch, in the middle; and the SVC, the smallest of the three, in a more inferior position (Fig. 9.2). Figure 5.17 in Chapter 5 shows the relationship of the aortic and ductal arches in an anatomic specimen, where the SVC has been removed.
Color Doppler reveals anteroposterior flow in both ductal and aortic arches (7) (Fig. 9.3). By reducing the color Doppler velocity scale, blood flow in the SVC and the azygos arch entering the SVC is recognized (Fig. 9.4A). By further lowering the color Doppler velocity scale and orienting the transducer in a slightly more cranial plane, the mammarian arteries can be visualized running on the lateral borders of the thymus (Fig. 9.4B) in a view called the “thy-box” (13). A more cranial plane will show blood flow in the left brachiocephalic vein (LBCV), in a left-to-right direction (14), which is always opposite to the direction of the aortic blood flow seen in a more caudal plane (see Chapter 10).
Typical Abnormal Findings in the Three-Vessel-Trachea View
As shown in various chapters within this book, cardiac anomalies involving the great vessels are commonly associated with abnormal appearances of the 3VT views. In few conditions, however, the abnormal 3VT is pathognomonic or highly suggestive for a specific cardiovascular abnormality (9). An abnormal 3VT view can thus provide clues for certain group of abnormalities, which requires confirmation following a comprehensive examination of the fetal heart (9). In this section, we present common 3VT view abnormalities, and discuss various associations with certain cardiovascular abnormalities. For a more comprehensive list of associations between an abnormal 3VT view and congenital heart disease, the readers are referred to this book’s chapters on abnormal hearts and various review articles (5–9, 15).
Narrow or Absent Aortic Arch
A narrow aortic arch on a 3VT view in gray scale is suggestive for left ventricular outflow tract obstruction as in aortic coarctation or tubular hypoplasia of the aortic arch (Fig. 9.5). Color Doppler is very helpful in these conditions, as the presence of reverse flow in a narrow aortic arch (Fig. 9.6B) is typical for aortic atresia or severe aortic stenosis as part of hypoplastic left heart syndrome or severe critical aortic stenosis. The presence of antegrade flow on color Doppler in a narrow aortic arch is typically found in aortic coarctation (Fig. 9.6A). An absence of the continuity of the aortic arch on 2D is suggestive for an interrupted aortic arch (Fig. 9.5B), and in color Doppler, the presence of antegrade flow in the proximal aortic arch and absent flow in the distal aortic arch confirm this condition.
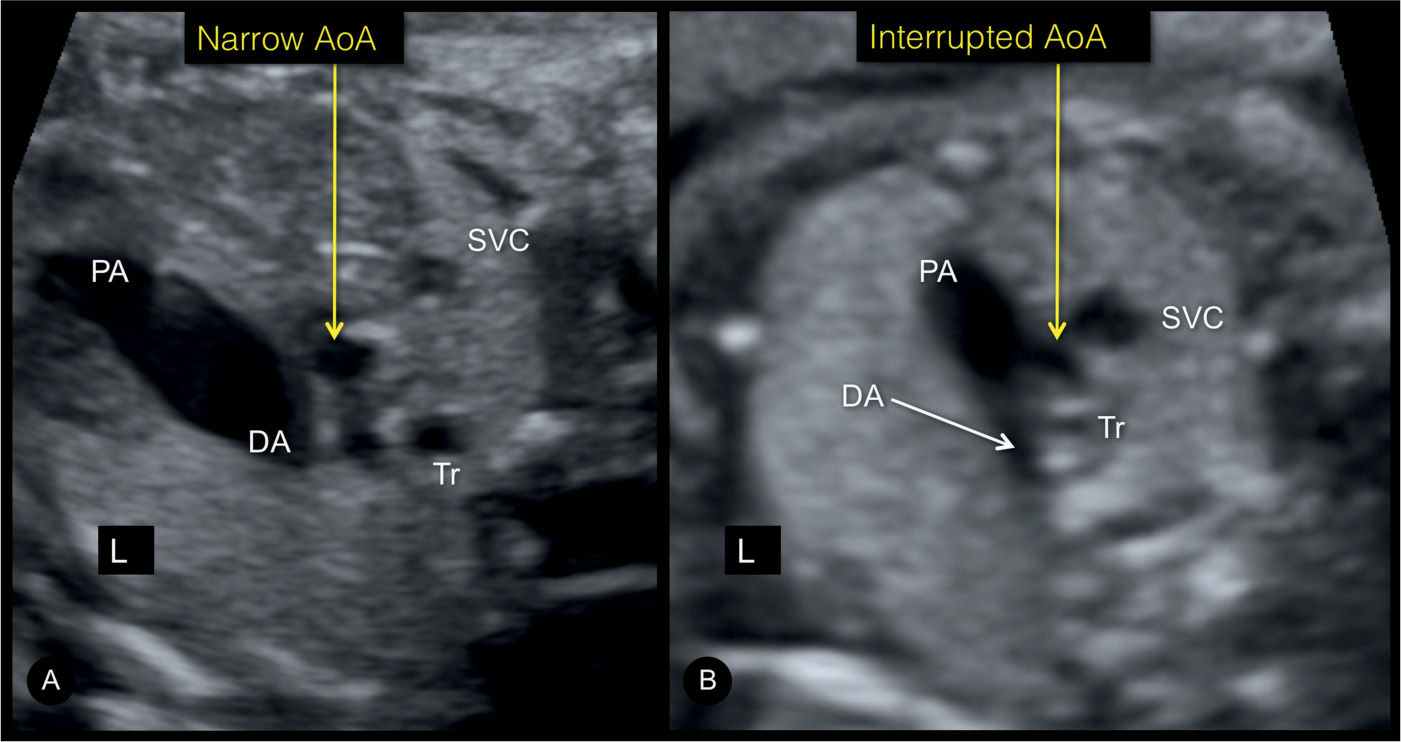
Figure 9.5: Three-vessel-trachea view in a fetus with a narrow aortic arch (AoA) in aortic coarctation (A) and in a fetus with an interrupted aortic arch (B). Note the absence of AoA continuity in B. DA, ductus arteriosus; PA, pulmonary artery; SVC, superior vena cava; Tr, trachea; L, left.
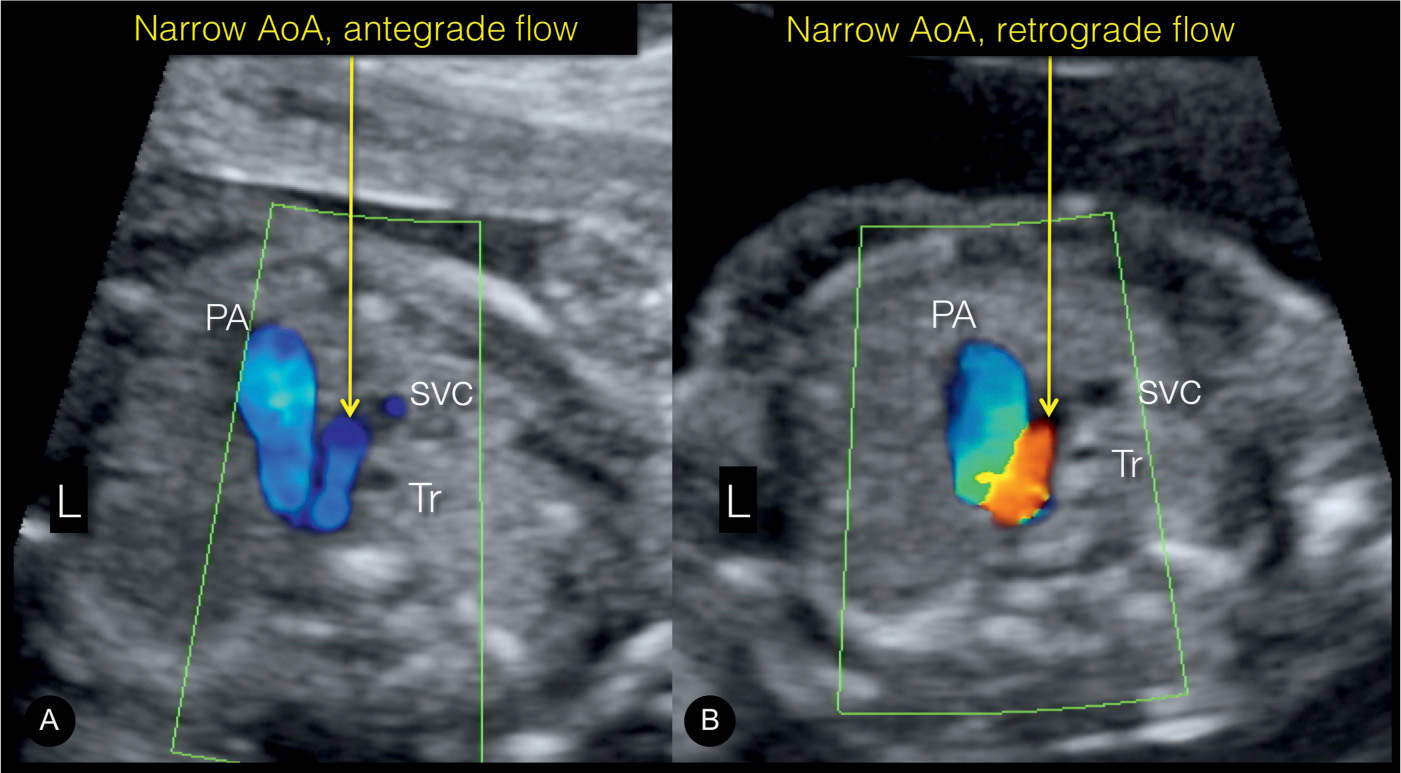
Figure 9.6: Three-vessel-trachea view in color Doppler in two fetuses with a narrow aortic arch (AoA). Note the presence of antegrade AoA flow in fetus A, suggestive of an aortic coarctation. In fetus B, retrograde flow in the AoA is seen, which is typical for hypoplastic left heart syndrome with aortic atresia. PA, pulmonary artery; SVC, superior vena cava; Tr, trachea; L, left.
Narrow or Absent Pulmonary Artery
A narrow or absent pulmonary artery in the 3VT view can be typically found in cardiac anomalies associated with right ventricular outflow tract obstruction as in pulmonary stenosis or atresia, showing reduced antegrade or reverse perfusion in the pulmonary artery on color Doppler. Cardiac anomalies commonly associated with this 3VT view abnormality include tetralogy of Fallot, Ebstein anomaly, pulmonary atresia, some cases of double outlet right ventricle, and many cases of tricuspid atresia with ventricular septal defect (VSD). In the cases of pulmonary stenosis, color Doppler shows antegrade flow in the narrow pulmonary artery when compared to the aorta (Fig. 9.7A). In the cases of pulmonary atresia (with and without VSD), grayscale ultrasound demonstrates a narrow or even nonvisible pulmonary artery, and color Doppler confirms the diagnosis by the presence of retrograde flow in the ductus arteriosus and pulmonary artery (Fig. 9.7B). In pulmonary atresia with intact septum, the ductus arteriosus is rather straight (see Chapter 24), whereas in pulmonary atresia with VSD it is often tortuous (see Chapter 25) or even completely absent.
Dilated Transverse Aortic Arch
A dilated transverse aortic arch in the 3VT view can be found in isolated aortic valve stenosis with poststenotic dilation of the aorta. Color Doppler confirms the diagnosis with typical turbulent antegrade flow of high velocity.
Dilated Pulmonary Artery
A dilated pulmonary artery in the 3VT view can be found in isolated pulmonary valve stenosis with poststenotic dilation of the main pulmonary artery. Color Doppler typically shows turbulent antegrade flow in the pulmonary artery (Fig. 9.8B). A hugely dilated pulmonary artery in the 3VT view is typically found in tetralogy of Fallot with absent pulmonary valve syndrome (Fig. 9.8A), with color Doppler showing to and fro blood flow across the pulmonary valve with patterns of severe stenosis and insufficiency. Absent pulmonary valve syndrome is often present in association with the absence of the arterial duct.
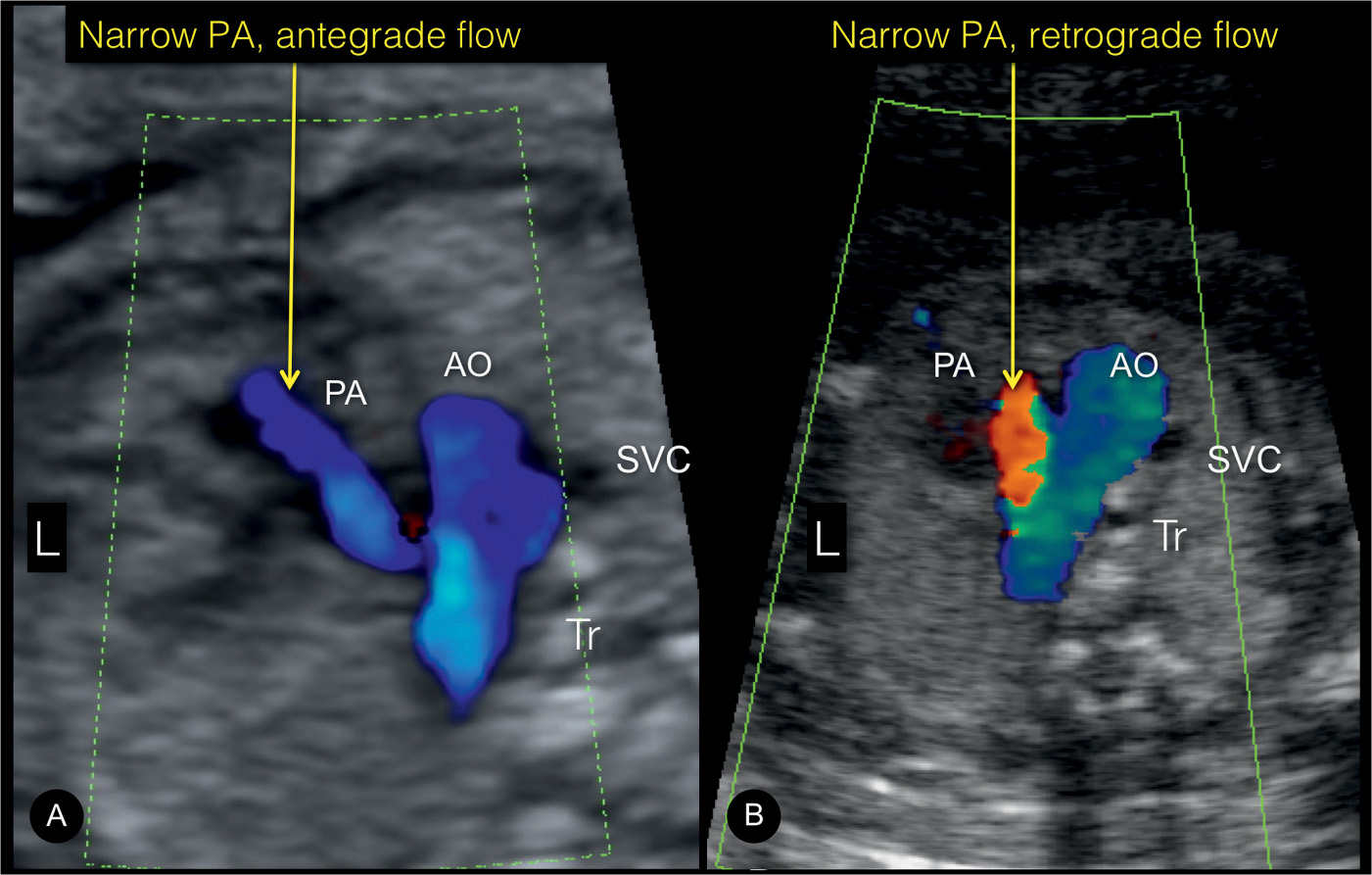
Figure 9.7: Three-vessel-trachea view in color Doppler in two fetuses with a narrow pulmonary artery (PA). Note the presence of antegrade PA flow in fetus A, suggestive of reduced flow pattern as in pulmonary stenosis in tetralogy of Fallot. In fetus B, retrograde flow in the PA is seen, which is typical for pulmonary atresia. AO, aorta; SVC, superior vena cava; Tr, trachea; L, left.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


