Surgical Anatomy of the Female Pelvis
John O.L. DeLancey
DEFINITIONS
Endopelvic fascia—The endopelvic fascias are those tissues outside of the muscularis of the pelvic organs that attach these organs to the pelvic sidewall. There is also some extension of loose areolar tissue over the surfaces of the organ. The surgical fascia used by gynecologists during pelvic reconstructive surgery, however, is primarily composed of the muscularis of the vaginal wall.
Pelvic diaphragm—The term pelvic diaphragm refers to the levator ani muscle and its covering fasciae, both the superior fascia and the inferior fascia. The term pelvic floor refers to all of the supportive structures that are involved with pelvic organ support. Sometimes the term pelvic floor and pelvic diaphragm can be used interchangeably, especially in the British literature.
Pelvic spaces—The space between the bladder and the anterior portion of the pelvic walls is the perivesical space or space of Retzius. The space between the lower urinary tract and the genital tract is the vesicovaginal or vesicocervical space. This is bounded laterally by the “bladder pillars,” which is the region in which the tissues that go to the vagina separate from those that go to the bladder base. The rectovaginal space lies between the posterior vaginal wall and the anterior surface of the rectum, and lies primarily above the top of the perineal body.
Urethra and vesicle neck—The urethra is that portion of the lower urinary tract outside of the bladder that the urethral lumen traverses. That portion of the urethra lumen that is surrounded by the bladder vasculature is referred to as the vesicle neck.
Urinary trigone—The urinary trigone is a triangular visible area in the bladder, the apices of which are the ureteral orifices and the internal urinary meatus. This is a layer of smooth muscle connecting the ureters and the urethra, the edges of which are visible cystoscopically and when the bladder is open.
VULVA AND ERECTILE STRUCTURES
The bony pelvic outlet is bordered by the ischiopubic rami anteriorly and the coccyx and sacrotuberous ligaments posteriorly. It can be divided into anterior and posterior triangles, which share a common base along a line between the ischial tuberosities. The tissues filling the anterior triangle have a layered structure similar to that of the abdominal wall (Table 7.1). There is a skin and adipose layer (vulva) overlying a fascial layer (perineal membrane) that lies superficial to a muscular layer (levator ani muscles).
Subcutaneous Tissues of the Vulva
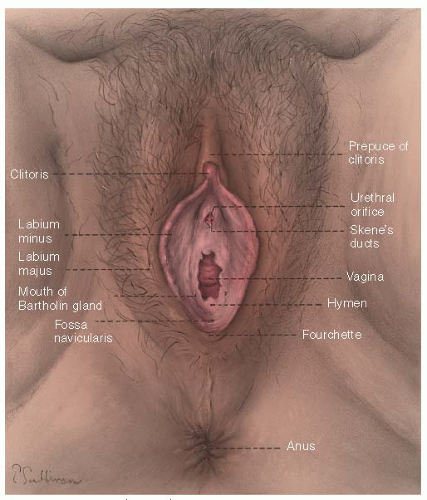
The structures of the vulva lie on the pubic bones and extend caudally under the pubic arch (Fig. 7.1). They consist of the mons, labia, clitoris, vestibule, and associated erectile structures and their muscles. The mons consists of hair-bearing skin over a cushion of adipose tissue that lies on the pubic bones. Extending posteriorly from the mons, the labia majora are composed of similar hair-bearing skin and adipose tissue, which contain the termination of the round ligaments of the uterus and the obliterated processus vaginalis (canal of Nuck). The round ligament can give rise to leiomyomas in this region, and the obliterated processus vaginalis can be a dilated embryonic remnant in the adult.
The labia minora, vestibule, and glans clitoris can be seen between the two labia majora. The labia minora are hairless skin folds, each of which splits anteriorly to run over, and under, the glans of the clitoris. The more anterior folds unite to form the hood-shaped prepuce of the clitoris, whereas the posterior folds insert into the underside of the glans as the frenulum.
Unlike the skin of the labia majora, the cutaneous structures of the labia minora and vestibule do not lie on an adipose layer but on a connective tissue stratum that is loosely organized and permits mobility of the skin during intercourse. This loose attachment of the skin to underlying tissues allows the skin to be easily dissected off the underlying fascia during skinning vulvectomy in the area of the labia minora and vestibule.
In the posterior lateral aspect of the vestibule, the duct of the major vestibular gland can be seen 3 to 4 mm outside
the hymenal ring. The minor vestibular gland openings are found along a line extending anteriorly from this point, parallel to the hymenal ring and extending toward the urethral orifice. The urethra bulges slightly around the surrounding vestibular skin anterior to the vagina and posterior to the clitoris. Its orifice is flanked on either side by two small labia. Skene ducts open into the inner aspect of these labia and can be seen as small, punctate openings when the urethral labia are separated.
the hymenal ring. The minor vestibular gland openings are found along a line extending anteriorly from this point, parallel to the hymenal ring and extending toward the urethral orifice. The urethra bulges slightly around the surrounding vestibular skin anterior to the vagina and posterior to the clitoris. Its orifice is flanked on either side by two small labia. Skene ducts open into the inner aspect of these labia and can be seen as small, punctate openings when the urethral labia are separated.
TABLE 7.1 Layers of the Anterior Triangle of the Perineum | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||
Within the skin of the vulva are specialized glands that can become enlarged and thereby require surgical removal. The holocrine sebaceous glands in the labia majora are associated with hair shafts, and in the labia minora, they are freestanding. They lie close to the surface, which explains their easy recognition with minimal enlargement. In addition, lateral to the introitus and anus, there are numerous apocrine sweat glands, along with the normal eccrine sweat glands. The former structures undergo change with the menstrual cycle, having increased secretory activity in the premenstrual period. They can become chronically infected, as in hidradenitis suppurativa, or neoplastically enlarged, as in hidradenomas, both of which may require surgical therapy. The eccrine sweat glands in the vulvar skin rarely present abnormalities, but on occasion form palpable masses as syringomas.
The subcutaneous tissue of the labia majora is similar in composition to that of the abdominal wall. It consists of lobules of fat interlaced with connective tissue septa. Although there are no well-defined layers in the subcutaneous tissue, regional variations in the relative quantity of fat and fibrous tissue exist. The superficial region of this tissue, where fat predominates, has been called Camper fascia, as it is on the abdomen. In this region, there is a continuation of fat from the anterior abdominal wall, called the digital process of fat.
In the deeper layers of the vulva, there is less fat, and the interlacing fibrous connective tissue septa are much more evident than those in Camper fascia. This more fibrous layer is called Colles fascia and is similar to Scarpa fascia on the abdomen. Its interlacing fibrous septa of the subcutaneous tissue attach laterally to the ischiopubic rami and fuse posteriorly with the posterior edge of the perineal membrane (i.e., urogenital diaphragm). Anteriorly, however, there is no connection to the pubic rami, and this permits communication between the area deep to this layer and the abdominal wall. These fibrous attachments to the ischiopubic rami and the posterior aspect of the perineal membrane limit the spread of hematomas or infection in this compartment posterolaterally but allow spread into the abdomen. This clinical observation has led to the consideration of Colles fascia as a separate entity from the superficial Camper fascia, which lacks these connections.
Superficial Compartment
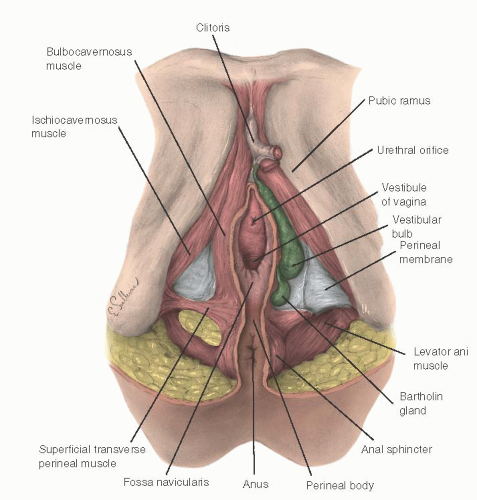
The space between the subcutaneous tissues and perineal membrane, which contains the clitoris, crura, vestibular bulbs, and ischiocavernous and bulbocavernosus muscles, is called the superficial compartment of the perineum (Fig. 7.2). The deep compartment is the region just above the perineal membrane; it is discussed later.
The erectile bodies and their associated muscles within the superficial compartment lie on the caudal surface of the perineal membrane. The clitoris is composed of a midline shaft (body) capped with the glans. This shaft lies on, and is suspended from, the pubic bones by a subcutaneous suspensory ligament. The paired crura of the clitoris bend downward from the shaft and are firmly attached to the pubic bones, continuing dorsally to lie on the inferior aspects of the pubic rami. The ischiocavernous muscles originate at the ischial tuberosities and the free surfaces of the crura to insert on the upper crura and body of the clitoris. A few muscle fibers, called the superficial transverse perineal muscles, originate in common with the ischiocavernous muscle from the ischial tuberosity and lie medial to the perineal body.
The paired vestibular bulbs lie immediately under the vestibular skin and are composed of erectile tissue. They are covered by the bulbocavernosus muscles, which originate in the perineal body and lie over their lateral surfaces. These muscles, along with the ischiocavernous muscles, insert into the body of the clitoris and act to pull it downward.
The Bartholin greater vestibular gland is found at the tail end of the bulb of the vestibule and is connected to the vestibular mucosa by a duct lined with squamous epithelium. The gland lies on the perineal membrane and beneath the bulbocavernosus muscle. The intimate relation between the enormously vascular erectile tissue of the vestibular bulb and the Bartholin gland is responsible for the hemorrhage associated with removal of this latter structure.
The perineal membrane and perineal body are important to the support of the pelvic organs. They are discussed in the section on the pelvic floor.
Pudendal Nerve and Vessels
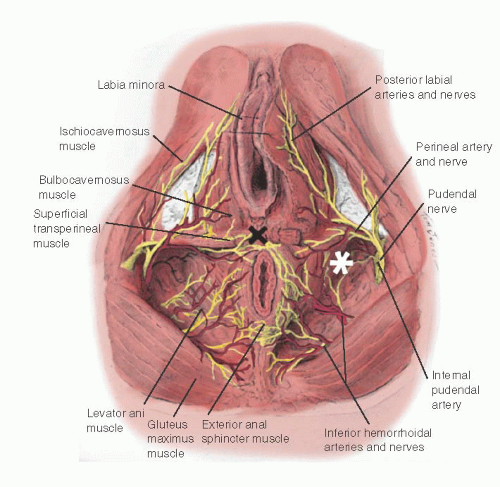
The pudendal nerve is the sensory and motor nerve of the perineum. Its course and distribution in the perineum parallel the pudendal artery and veins that connect with the internal iliac vessels (Fig. 7.3). The course and division of the nerve are described with the understanding that the vascular channels parallel them.
The pudendal nerve arises from the sacral plexus (S2-S4), and the vessels originate from the anterior division of the internal iliac artery. They leave the pelvis through the greater sciatic foramen by hooking around the ischial spine and sacrospinous ligament to enter the pudendal (Alcock) canal through the lesser sciatic foramen.
The nerve and vessels have three branches: the clitoral, perineal, and inferior hemorrhoidal. The clitoral branch lies on the perineal membrane along its path to supply the clitoris. The perineal branch (the largest of the three branches) enters the subcutaneous tissues of the vulva behind the perineal membrane. Here, it supplies the bulbocavernosus, ischiocavernous, and transverse perineal muscles. It also supplies the skin of the inner portions of the labia majora, labia minora, and vestibule. The inferior hemorrhoidal branch goes to the external anal sphincter and perianal skin.
Lymphatic Drainage
The pattern of the vulvar lymphatic vessels and drainage into the superficial inguinal group of lymph nodes has been established by both injection studies and clinical observation. It is important to the treatment of vulvar malignancies; an overview of this system is provided here. This area is described and illustrated in more detail in Chapter 33.
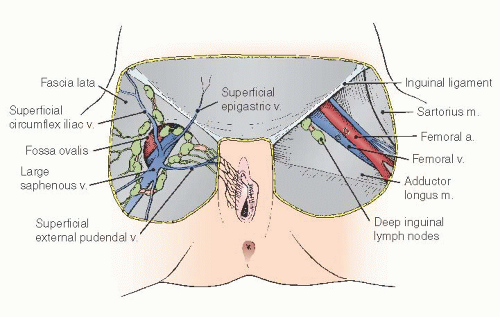
Tissues external to the hymenal ring are supplied by an anastomotic series of vessels in the superficial tissues that coalesce to a few trunks lateral to the clitoris and proceed laterally to the superficial inguinal nodes (Fig. 7.4). The vessels draining the labia majora also run in an anterior direction, lateral to those of the labia minora and vestibule. These lymphatic channels lie medial to the labiocrural fold, establishing it as the lateral border of surgical resection.
Injection studies of the urethral lymphatics have shown that lymphatic drainage of this region terminates in either the right or left inguinal nodes. The clitoris has been said to have some direct drainage to deep pelvic lymph nodes, bypassing the usual superficial nodes, but the clinical significance of this appears to be minimal.
The inguinal lymph nodes are divided into two groups— the superficial and the deep nodes. There are 12 to 20 superficial nodes, and they lie in a T-shaped distribution parallel to and 1 cm below the inguinal ligament, with the stem extending down along the saphenous vein. The nodes are often divided into four quadrants, with the center of the division at the saphenous opening. The vulvar drainage goes primarily to the medial nodes of the upper quadrant. These nodes lie deep in the adipose layer of the subcutaneous tissues, in the membranous layer, just superficial to the fascia lata.
The large saphenous vein joins the femoral vein through the saphenous opening. Within 2 cm of the inguinal ligament, several superficial blood vessels branch from the saphenous vein and femoral artery. They include the superficial epigastric vessels that supply the subcutaneous tissues of the lower abdomen; the superficial circumflex iliac vessels that course laterally to the region of the iliac crest; and the superficial external pudendal vessels that supply the mons, labia majora, and clitoral hood.
Lymphatics from the superficial nodes enter the fossa ovalis and drain into one to three deep inguinal nodes, which lie in the femoral canal of the femoral triangle. They pass through the fossa ovalis (saphenous opening) in the fascia lata, which lies approximately 3 cm below the inguinal ligament, lateral to the pubic tubercle, along with the saphenous vein on its way to the femoral vein. The membranous layer of the subcutaneous tissues spans this opening as a trabeculate layer called a fascia cribrosa, pierced by lymphatics. The deep nodes are found under this fascia in the femoral triangle.
The femoral triangle is the subfascial space of the upper one third of the thigh. It is bounded by the inguinal ligament, sartorius muscle, and adductor longus muscle. Its floor is formed by the pectineal, adductor longus, and iliopsoas muscles. The femoral artery bisects it vertically between the anterosuperior iliac spine and pubic tubercle. The femoral vein lies medial to the artery; the femoral nerve is lateral to it.
As these vessels pass under the inguinal ligament, they carry with them an extension of the transversalis fascia, which is the extraperitoneal connective tissue deep to the rectus abdominis muscle called the femoral sheath. These sheaths extend about 2 to 3 cm below the inguinal ligament before fusing with the vascular adventitia. Besides the two parts of the femoral sheath that accompany these vessels, a third portion—the femoral canal—can be found in the space medial to the vein. The abdominal opening of this is the femoral ring. The femoral canal contains the deep inguinal lymph nodes. Lymph channels from these nodes pierce the membrane, filling the femoral ring to communicate with the external iliac nodes. Also within this region, the femoral vessels give rise to the deep external pudendal vessels. The external pudendal vessels run deep to the femoral vein over the pectineal muscle to pierce the fascia lata. Here, they become subcutaneous and form anastomoses
with branches of the internal pudendal vessels as well as the deep femoral and lateral circumflex femoral arteries.
with branches of the internal pudendal vessels as well as the deep femoral and lateral circumflex femoral arteries.
THE PELVIC FLOOR
When humans assumed the upright posture, the opening in the bony pelvis came to lie at the bottom of the abdominopelvic cavity. This required the evolution of a supportive system to prevent the pelvic organs from being pushed downward through this opening. In the woman, this system must withstand these downward forces but allow for the passage of the large and cranially dominant human fetus. The supportive system that has evolved to meet these needs consists of a fibromuscular floor that forms a shelf spanning the pelvic outlet and that contains a cleft for the birth canal and excretory drainage. A series of visceral ligaments and fasciae tethers the organs and maintains their position over the closed portions of the floor. The floor consists of the levator ani muscles and perineal membrane. The openings in these structures for parturition and elimination have required the development of ancillary fibrous elements that are concentrated over open areas in the muscular floor to support the viscera in these weak areas. This section discusses the structures of the pelvic floor; the fibrous supportive system is described in the section on the pelvic viscera and cleavage planes and fascia.
Perineal Membrane (Urogenital Diaphragm)
The perineal membrane forms the inferior portion of the anterior pelvic floor. It is a triangular sheet of dense, fibromuscular tissue that spans the anterior half of the pelvic outlet (Fig. 7.2). It was previously called the urogenital diaphragm, and this change in name reflects the appreciation that it is not a two-layered structure with muscle in between, as was previously thought. It lies just caudal to the skeletal muscle of the striated urogenital sphincter (formerly the deep transverse perineal muscle). Because of the presence of the vagina, the perineal membrane cannot form a continuous sheet to close off the anterior pelvis in the woman, as it does in the man. It does provide support for the posterior vaginal wall by attaching the perineal body and vagina and perineal body to the ischiopubic rami, thereby limiting their downward descent. This layer of the floor arises from the inner aspect of the inferior ischiopubic rami above the ischiocavernous muscles and the crura of the clitoris. The medial attachments of the perineal membrane are to the urethra, walls of the vagina, and perineal body.
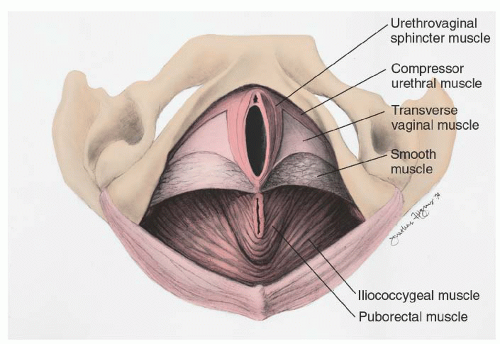 FIGURE 7.5 Structures visible after removal of the perineal membrane and superficial perineal muscles. (Copyright 1995 John O. L. DeLancey, with permission.) |
Just cephalad to the perineal membrane lie two archshaped muscles that begin posteriorly to arch over the urethra (Fig. 7.5). These are the compressor urethral and the urethrovaginal sphincters. They are a part of the striated urogenital sphincter muscle in the woman and are continuous with the sphincter urethrae muscle. They act to compress the distal urethra. Posteriorly, intermingled within the membrane are skeletal muscle fibers of the transverse vaginal muscle and some smooth muscle fibers. The dorsal and deep nerve and vessels of the clitoris are also found within this membrane and are described later.
The primary function of the perineal membrane is related to its attachment to the vagina and perineal body. By attaching these structures to the bony pelvic outlet, the perineal membrane supports the pelvic floor against the effects of increases in intra-abdominal pressure and against the effects of gravity. The pubococcygeal and puborectal portions of the levator ani muscles lie just at the upper margin of the perineal membrane contacting its cranial surface. Contraction of these muscles elevates the medial margin of the perineal membrane along with the vagina and relaxation allows for its caudal movement. The amount of downward descent that is permitted by the connections of the perineal membrane to the midline structures can be assessed during an examination under anesthesia by placing a finger in the rectum, hooking it forward, and gently pulling the perineal body downward. If the perineal membrane has been torn during parturition, then an abnormal amount of descent is detectable, and the pelvic floor sags and the introitus gapes.
Perineal Body
Within the area bounded by the lower vagina, perineal skin, and anus is a mass of connective tissue called the perineal body (Fig. 7.3). The term central tendon of the perineum has also been applied to this structure and is descriptive, suggesting its role as a central point into which many muscles insert.
The perineal body is attached to the inferior pubic rami and ischial tuberosities through the perineal membrane and
superficial transverse perineal muscles. Anterolaterally, it receives the insertion of the bulbocavernosus muscles. On its lateral margins, the upper portions of the perineal body are connected with some fibers of the pelvic diaphragm. Posteriorly, the perineal body is indirectly attached to the coccyx by the external anal sphincter that is embedded in the perineal body, and it is attached at its other end to the coccyx. These connections anchor the perineal body and its surrounding structures to the bony pelvis and help to keep it in place.
superficial transverse perineal muscles. Anterolaterally, it receives the insertion of the bulbocavernosus muscles. On its lateral margins, the upper portions of the perineal body are connected with some fibers of the pelvic diaphragm. Posteriorly, the perineal body is indirectly attached to the coccyx by the external anal sphincter that is embedded in the perineal body, and it is attached at its other end to the coccyx. These connections anchor the perineal body and its surrounding structures to the bony pelvis and help to keep it in place.
Posterior Triangle: Ischiorectal Fossa
In the posterior triangle of the pelvis, the ischiorectal fossa lies between the pelvic walls and the levator ani muscles (Fig. 7.3). It has an anterior recess that lies above the perineal membrane. It is bounded medially by the levator ani muscles and anterolaterally by the obturator internus muscle. The main portion of the fossa is lateral to the levator ani and external anal sphincter, and it has a posterior portion that extends above the gluteus maximus. Traversing this region is the pudendal neurovascular trunk.
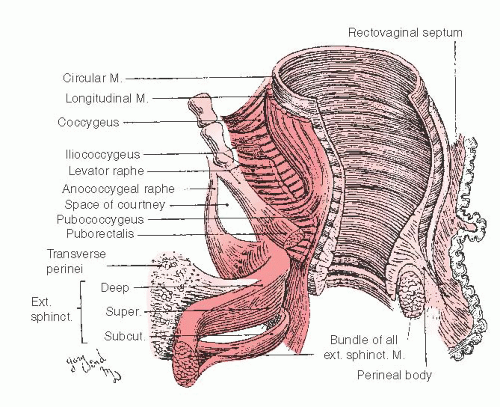
Anal Sphincters
The external sphincter lies in the posterior triangle of the perineum (Fig. 7.6). It is a single mass of muscle that has traditionally been divided into superficial and deep portions. The subcutaneous portion lies attached to the perianal skin and forms an encircling ring around the anal canal. It is responsible for the characteristic radially oriented folds in the perianal skin. The superficial part attaches to the coccyx posteriorly and sends a few fibers into the perineal body anteriorly and forms the bulk of the anal sphincter seen separated in third-degree midline obstetric tears. The fibers of the deep part generally encircle the rectum and blend indistinguishably with the puborectalis, which forms a loop under the dorsal surface of the anorectum and which is attached anteriorly to the pubic bone (Fig. 7.6).
The internal anal sphincter is a thickening in the circular smooth muscle of the anal wall. It lies just inside the external anal sphincter and is separated from it by a visible intersphincteric groove. It extends downward inside the external anal sphincter to within a few millimeters of the external sphincter’s caudal extent. The internal sphincter can be identified just beneath the anal submucosa in repair of a chronic fourthdegree laceration of the perineum as a rubbery white layer that is often erroneously been referred to as fascia during obstetrical repair of fourth-degree laceration. The longitudinal smooth muscle layer of the bowel, along with some fibers of the levator ani, separates the external and internal sphincters as they descend in the intersphincteric groove.
Levator Ani and Pelvic Wall
The typical depiction of the levator ani muscles in anatomy textbooks is unfortunately distorted by the extreme abdominal pressures generated during embalming that forces them downward. Many of these illustrations therefore fail to give a true picture of the horizontal nature of this strong supportive shelf of muscle. Examination of the normal standing patient is the best way to appreciate the nature of this closure mechanism, because the lithotomy position causes some relaxation of the musculature. During routine pelvic examination of the nullipara, the effectiveness of this closure can be appreciated, because it is often difficult to insert a speculum if the muscles are contracted and not relaxed.
The pelvic canal is spanned by the muscles of the pelvic diaphragm. This diaphragm consists of two components: (a) a thin horizontal shelf-like layer formed by the iliococcygeal muscle and (b) a thicker “U”-shaped sling of muscles that surround the levator hiatus that include the medial pubococcygeal and lateral puborectal muscles (Fig. 7.7). The open area within the U through which the urethra, vagina, and rectum pass is called the levator hiatus, and the portion of the hiatus anterior to the perineal body is called the urogenital hiatus.
The pubococcygeal muscle arises from a thin aponeurotic attachment to the inner surface of the pubic bone and inserts to the distal lateral vagina, perineal body, and anus. Some fibers also attach to the superior surface of the coccyx; hence the name pubococcygeus. Because the majority of the attachments, however, are to the vagina and anus, the term pubovisceral muscle is replacing this older term. The puborectal muscle is distinct from the pubococcygeal muscle and lies lateral to it. Its fibers originate from the lower pubis and some from the top of the perineal membrane. The muscle fibers pass beside the rectum forming a sling behind the anorectal junction.
The iliococcygeal muscle arises from a fibrous band overlying the obturator internus called the arcus tendineus levatoris ani. From these broad origins, the fibers of the iliococcygeal muscle pass behind the rectum and insert into the midline anococcygeal raphe and the coccyx. The coccygeal muscle arises from the ischial spine and sacrospinous ligament to insert into the borders of the coccyx and the lowest segment of the sacrum.
These muscles are covered on their superior and inferior surfaces by superior and inferior fasciae. When the levator ani muscles and their fasciae are considered together, they are called the pelvic diaphragm, not to be confused with the urogenital diaphragm (perineal membrane).
The normal tone of the muscles of the pelvic diaphragm keep the base of the U pressed against the backs of the pubic bones, keeping the vagina and rectum closed. The region of the levator ani between the anus and coccyx formed by the anococcygeal raphe (see previous discussion) is clinically called the levator plate. It forms a supportive shelf on which the rectum, upper vagina, and uterus can rest. The relatively horizontal position of this shelf is determined by the anterior traction on the fibrous levator plane by the pubococcygeal and puborectal muscles and is important to vaginal and uterine support.
The levator ani muscles receive their innervation from an anterior branch of the ventral ramus of the third and fourth sacral nerves called, appropriately, the nerve to the levator ani. Some aspects of the puborectal muscle may also receive a small contribution to the inferior hemorrhoidal branch of the pudendal nerve.
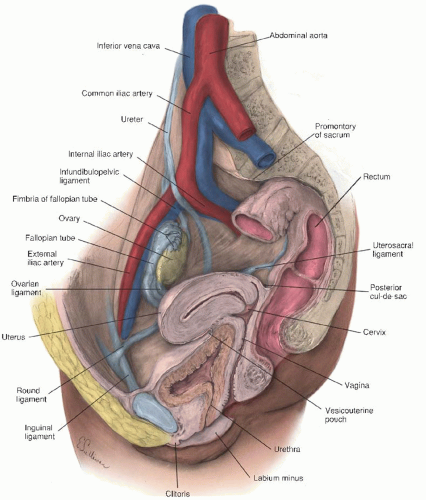
This section on the pelvic viscera discusses the structure of the individual pelvic organs and considers specific aspects of their interrelations (Fig. 7.8). Those aspects of blood supply, innervation, and lymphatic drainage that are idiosyncratic to the specific pelvic viscera are covered here. However, the section on the retroperitoneum, where the overall description of these systems is given, provides the general consideration of these latter three topics.
Genital Structures
Vagina
The vagina is a pliable hollow viscus with a shape that is determined by the structures surrounding it and by its attachments to the pelvic wall. These attachments are to the lateral margins of the vagina, so that its lumen is a transverse slit, with the anterior and posterior walls in contact with one another. The lower portion of the vagina is constricted as it passes through the urogenital hiatus in the levator ani. The upper part is much more capacious. The vagina is bent at an angle of 120 degrees by the anterior traction of the levator ani muscles at the junction of the lower one third and upper two thirds of the vagina (Fig. 7.9). The cervix typically lies within the anterior vaginal wall, making it shorter than the posterior wall by about 3 cm. The former is about 7 to 9 cm in length, although there is great variability in this dimension.
When the lumen of the vagina is inspected through the introitus, many landmarks can be seen. The anterior and posterior walls have a midline ridge, called the anterior and posterior columns, respectively. These are caused by the impression of the urethra and bladder and the rectum on the vaginal lumen. The caudal portion of the anterior column is distinct and is called the urethral carina. The recesses in front of and behind the cervix are commonly called the anterior and posterior fornices of the vagina, and the creases along the side of the vagina, where the anterior and posterior walls meet, are called the lateral vaginal sulci.
The vagina’s relations to other parts of the body can be understood by dividing it into thirds. In the lower third, the
vagina is fused anteriorly with the urethra, posteriorly with the perineal body, and laterally to each levator ani by the “fibers of Luschka.” In the middle third are the vesical neck and trigone anteriorly, the rectum posteriorly, and the levators laterally. In the upper third, the anterior vagina is adjacent to the bladder and ureters (which allow these latter structures to be palpated on pelvic examination), posterior to the cul-de-sac, and lateral to the cardinal ligaments of the vagina.
vagina is fused anteriorly with the urethra, posteriorly with the perineal body, and laterally to each levator ani by the “fibers of Luschka.” In the middle third are the vesical neck and trigone anteriorly, the rectum posteriorly, and the levators laterally. In the upper third, the anterior vagina is adjacent to the bladder and ureters (which allow these latter structures to be palpated on pelvic examination), posterior to the cul-de-sac, and lateral to the cardinal ligaments of the vagina.
The vaginal wall contains the same layers as all hollow viscera (i.e., mucosa, submucosa, muscularis, and adventitia). Except for the area covered by the cul-de-sac, it has no serosal covering. The mucosa is of the nonkeratinized stratified squamous type and lies on a dense, dermislike submucosa. The similarity of these layers to dermis and epidermis has resulted in their being called the “vaginal skin.”
The vaginal muscularis is fused with the submucosa, and the pattern of the muscularis is a bihelical arrangement. Outside the muscularis, there is an adventitia that has varying degrees of development in different areas of the vagina. This layer is a portion of the connective tissue in the pelvis called the endopelvic fascia and has been given a separate name because of its unusual development. When it is dissected in the operating room, the muscularis is usually adherent to it, and this combination of specialized adventitia and muscularis is the surgeon’s “fascia,” which might better be called the fibromuscular layer of the vagina, as Nichols and Randall suggested in Vaginal Surgery.
Uterus
The uterus is a fibromuscular organ with shape, weight, and dimensions that vary considerably, depending on both estrogenic stimulation and previous parturition. It has two portions: an upper muscular corpus and a lower fibrous cervix. In a woman of reproductive age, the corpus is considerably larger than the cervix, but before menarche, and after the menopause, their sizes are similar. Within the corpus, there is a triangularly shaped endometrial cavity surrounded by a thick muscular wall. That portion of the corpus that extends above the top of the endometrial cavity (i.e., above the insertions of the fallopian tubes) is called the fundus.
The muscle fibers that make up most of the uterine corpus are not arranged in a simple layered manner, as is true
in the gastrointestinal tract, but are arranged in a more complex pattern. This pattern reflects the origin of the uterus from paired paramesonephric primordia, with the fibers from each half crisscrossing diagonally with those of the opposite side.
in the gastrointestinal tract, but are arranged in a more complex pattern. This pattern reflects the origin of the uterus from paired paramesonephric primordia, with the fibers from each half crisscrossing diagonally with those of the opposite side.
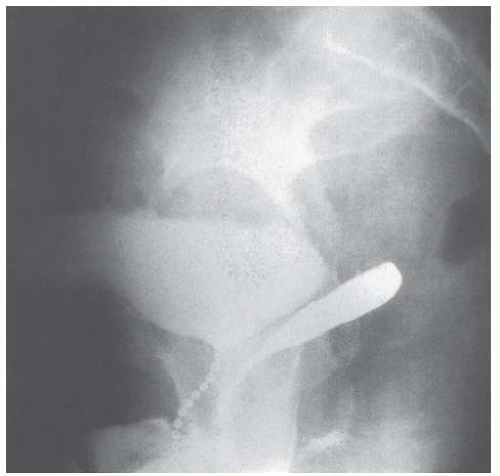 FIGURE 7.9 Bead chain cystourethrogram with barium in the vagina showing normal vaginal axis in a patient in the standing position. |
The uterus is lined by a unique mucosa, the endometrium. It has both a columnar epithelium that forms glands and a specialized stroma. The superficial portion of this layer undergoes cyclic change with the menstrual cycle. Spasm of hormonally sensitive spiral arterioles that lie within the endometrium causes shedding of this layer after each cycle, but a deeper basal layer of the endometrium remains to regenerate a new lining. Separate arteries supply the basal endometrium, explaining its preservation at the time of menses.
The cervix is divided into two portions: the portio vaginalis, which is that part protruding into the vagina; and the portio supravaginalis, which lies above the vagina and below the corpus.
The substance of the cervical wall is made up of dense fibrous connective tissue with only a small (about 10%) amount of smooth muscle. What smooth muscle is there lies on the periphery of the cervix, connecting the myometrium with the muscle of the vaginal wall. This smooth muscle and accompanying fibrous tissue are easily dissected off the fibrous cervix and form the layer reflected during intrafascial hysterectomy. It is circularly arranged around the fibrous cervix and is the tissue into which the cardinal and uterosacral ligaments and pubocervical fascia insert.
The portio vaginalis is covered by nonkeratinizing squamous epithelium. Its canal is lined by a columnar mucus-secreting epithelium that is thrown into a series of V-shaped folds that appear like the leaves of a palm and are therefore called plicae palmatae. These form compound clefts in the endocervical canal, not tubular racemose glands, as formerly thought.
The upper border of the cervical canal is marked by the internal os, where the narrow cervical canal widens out into the endometrial cavity. The lower border of the canal, the external os, contains the transition from squamous epithelium of the portio vaginalis to the columnar epithelium of the endocervical canal. This occurs at a variable level relative to the os and changes with hormonal variations that occur during a woman’s life. It is in this active area of cellular transition that the cervix is most susceptible to malignant transformation.
There is little adventitia in the uterus, with the peritoneal serosa being directly attached to most of the corpus. The anterior portion of the uterine cervix is covered by the bladder; therefore, it has no serosa. Similarly, as discussed in the following, the broad ligament envelops the lateral aspects of the cervix and corpus; therefore, it has no serosal covering there. The posterior cervix does have a serosal covering.
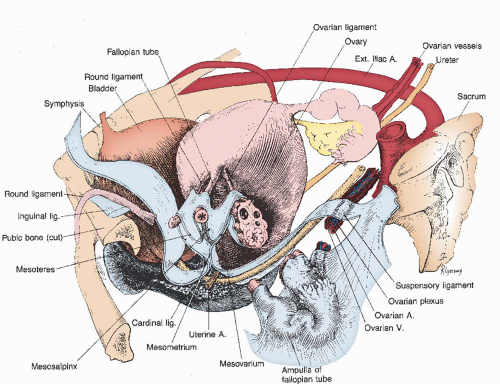
Adnexal Structures and Broad Ligament
The fallopian tubes are paired tubular structures 7 to 12 cm in length (Fig. 7.10). Each has four recognizable portions. At the uterus, the tube passes through the cornu as an interstitial
portion. On emerging from the corpus, a narrow isthmic portion begins with a narrow lumen and thick muscular wall. Proceeding toward the abdominal end, next is the ampulla, which has an expanding lumen and more convoluted mucosa. The fimbriated end of the tube has many frondlike projections to provide a wide surface for ovum pickup. The distal end of the fallopian tube is attached to the ovary by the fimbria ovarica, which is a smooth muscle band responsible for bringing the fimbria and ovary close to one another at the time of ovulation. The outer layer of the tube’s muscularis is composed of longitudinal fibers; the inner layer has a circular orientation.
portion. On emerging from the corpus, a narrow isthmic portion begins with a narrow lumen and thick muscular wall. Proceeding toward the abdominal end, next is the ampulla, which has an expanding lumen and more convoluted mucosa. The fimbriated end of the tube has many frondlike projections to provide a wide surface for ovum pickup. The distal end of the fallopian tube is attached to the ovary by the fimbria ovarica, which is a smooth muscle band responsible for bringing the fimbria and ovary close to one another at the time of ovulation. The outer layer of the tube’s muscularis is composed of longitudinal fibers; the inner layer has a circular orientation.
The lateral pole of the ovary is attached to the pelvic wall by the infundibulopelvic ligament and the ovarian artery and vein contained therein. Medially, it is connected to the uterus through the utero-ovarian ligament. During reproductive life, it measures about 2.5 to 5 cm long, 1.5 to 3 cm thick, and 0.7 to 1.5 cm wide, varying with its state of activity or suppression, as with oral contraceptive medications. Its surface is mostly free but has an attachment to the broad ligament through the mesovarium, as discussed in the following.
The ovary has a cuboidal to columnar covering and consists of a cortex and medulla. The medullary portion is primarily fibromuscular, with many blood vessels and much connective tissue. The cortex is composed of a more specialized stroma, punctuated with follicles, corpora lutea, and corpora albicantia.
The round ligaments are extensions of the uterine musculature and represent the homolog of the gubernaculum testis. They begin as broad bands that arise on each lateral aspect of the anterior corpus. They assume a more rounded shape before they enter the retroperitoneal tissue, where they pass lateral to the deep inferior epigastric vessels and enter each internal inguinal ring. After traversing the inguinal canal, they exit the external ring and enter the subcutaneous tissue of the labia majora. They have little to do with uterine support.
The ovaries and tubes constitute the uterine adnexa. They are covered by a specialized series of peritoneal folds called the broad ligament. During embryonic development, the paired müllerian ducts and ovaries arise from the lateral abdominopelvic walls. As they migrate toward the midline, a mesentery of peritoneum is pulled out from the pelvic wall from the cervix on up. This leaves the midline uterus connected on either side to the pelvic wall by a double layer of peritoneum.
Within the upper layers of these two folds, called the broad ligament, lie the fallopian tubes, round ligaments, and ovaries (Fig. 7.11). The cardinal and uterosacral ligaments are at the lower margin of the broad ligament. These structures are visceral ligaments; therefore, they are composed of varying amounts of smooth muscle, vessels, connective tissue, and other structures. They are not the pure ligaments associated with joints in the skeleton.
The ovary, tube, and round ligament each have their own separate mesentery, called the mesovarium, mesosalpinx,
and mesoteres, respectively. These are arranged in a constant pattern, with the round ligament placed ventrally, where it exits the pelvis through the inguinal ligament, and the ovary placed dorsally. The tube is in the middle and is the most cephalic of the three structures. At the lateral end of the fallopian tube and ovary, the broad ligament ends where the infundibulopelvic ligament blends with the pelvic wall. The cardinal ligaments lie at the base of the broad ligament and are described under the section on supportive tissues and cleavage planes.
and mesoteres, respectively. These are arranged in a constant pattern, with the round ligament placed ventrally, where it exits the pelvis through the inguinal ligament, and the ovary placed dorsally. The tube is in the middle and is the most cephalic of the three structures. At the lateral end of the fallopian tube and ovary, the broad ligament ends where the infundibulopelvic ligament blends with the pelvic wall. The cardinal ligaments lie at the base of the broad ligament and are described under the section on supportive tissues and cleavage planes.
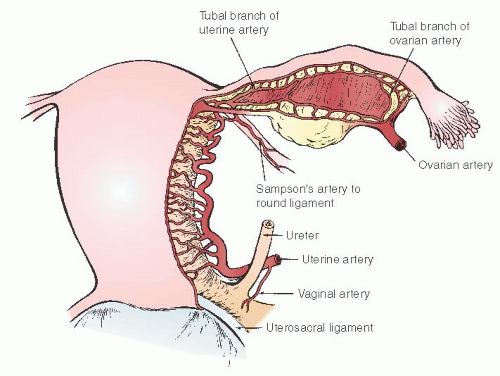
Blood Supply and Lymphatics of the Genital Tract
The blood supply to the genital organs comes from the ovarian arteries and uterine and vaginal branches of the internal iliac arteries. A continuous arterial arcade connects these vessels on the lateral border of the adnexa, uterus, and vagina (Fig. 7.10).
The blood supply of the upper adnexal structures comes from the ovarian arteries that arise from the anterior surface of the aorta just below the level of the renal arteries. The accompanying plexus of veins drains into the vena cava on the right and the renal vein on the left. The arteries and veins follow a long, retroperitoneal course before reaching the cephalic end of the ovary. They pass along the mesenteric surface of the ovary to connect with the upper end of the marginal artery of the uterus. Because the ovarian artery runs along the hilum of the ovary, it not only supplies the gonad but also sends many small vessels through the mesosalpinx to supply the fallopian tube, including a prominent fimbrial branch at the lateral end of the tube.
The uterine artery originates from the internal iliac artery. It usually arises independently from this source but can have a common origin with either the internal pudendal or vaginal artery. It joins the uterus near the junction of the corpus and cervix, but this position varies considerably, both with the individual and the amount of upward or downward traction placed on the uterus. Accompanying each uterine artery are several large uterine veins that drain the corpus and cervix.
On arriving at the lateral border of the uterus (after passing over the ureter and giving off a small branch to this structure), the uterine artery flows into the side of the marginal artery that runs along the side of the uterus. Through this connection, it sends blood both upward toward the corpus and downward to the cervix. Because the marginal artery continues along the lateral aspect of the cervix, it eventually crosses over the cervicovaginal junction and lies on the side of the vagina.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree