Structural Abnormalities of the Genitourinary Tract
George W. Kaplan
Irene M. McAleer
Anomalies of the genitourinary tract found in the neonatal period make up many of the pediatric urology problems. Some age-specific problems do not present in early infancy, but many conditions can present primarily or specifically in the neonatal period. The use of antenatal ultrasonography has had a profound effect on the detection, management, and understanding of many lesions of the urinary tract. Genitourinary anomalies account for approximately 50% of all antenatally sonographically detected lesions; hydronephrosis represents about two-thirds of these genitourinary abnormalities (1). Information from antenatal ultrasonography can be further complemented in utero with magnetic resonance imaging (MRI), fetal bladder urine specimen measurements of electrolytes, osmolality, and &bgr;2-microglobulin. In utero surgical therapy is also possible although the benefits derived from fetal surgery of the urinary tract thus far have not been proven and generally have a high complication rate for both the fetus and mother (2,3,4,5).
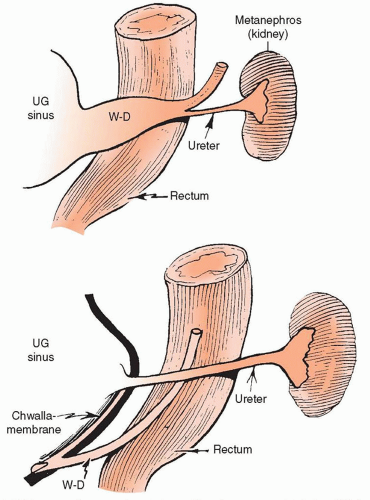
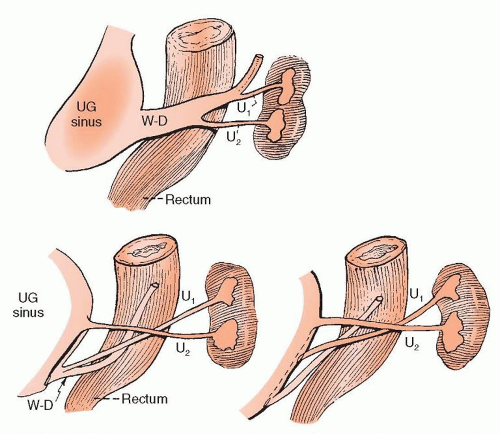
Understanding the significant events of embryogenesis of the genitourinary tract is essential to understand and interpret the findings seen in most congenital urologic problems. The ureteral bud arises from the mesonephric duct at 4 to 5 weeks of gestation, the kidney begins to form at 6 weeks, and the bladder develops during the 6th to 7th week. The wolffian duct is then incorporated into the bladder (Fig. 40.1). It is not until week 10 of gestation that urine production begins, but the urinary tract is generally not well imaged by antenatal ultrasonography until weeks 15 to 16 when the urinary tract is evident on antenatal ultrasonography (6). Disordered embryogenesis of the ureter or kidney is responsible for a number of anomalies. Most genitourinary anomalies seem to occur sporadically, although some abnormalities are familial and others are associated with chromosomal abnormalities. The concept of CAKUT (congenital abnormalities of the kidney and urinary tract) would suggest that many seemingly sporadic problems are actually familial (7).
▪ IMAGING
Fetal anomalies of the urinary tract are detected in about 1% of pregnancies. Urologic diagnostic imaging in the fetus, newborn, and infant has been transformed by the use of ultrasonography through all stages of development and after birth where previously neonatal renal function had to be sufficient to allow imaging of the genitourinary system for diagnostic purposes. Neonatal renal function may be sufficient to maintain homeostasis, but it may not suffice to produce an accurate diagnosis as it does in older children and adults with normal renal function. Many infants with congenital genitourinary conditions have extensive prenatal imaging, so a presumed diagnosis of many of these conditions, including those incompatible with life, may be determined well before delivery so that families and health professionals can be prepared for postnatal management of these varied conditions.
Ultrasonography and voiding cystourethrography are not dependent on renal function and are the mainstay of diagnostic imaging for genitourinary conditions. Improved ultrasonographic equipment, resolution, and techniques are identifying fetal anomalies with great accuracy earlier in gestation to assist in postnatal planning for the fetus with genitourinary problems. Renal scintigraphy depends on renal function to produce images and consequently may not yield reliable information in the first few weeks of life. MRI, computed tomography (CT) imaging, and some scintigraphic agents have made evaluation of the neonatal kidneys and bladder more reliable and diagnostic.
▪ ANOMALIES OF THE KIDNEY
Understanding normal embryogenesis, genitourinary anomalies, and associated problems can be anticipated, because most have an embryologic basis. Some conditions are incompatible with life, which may lead to an early demise although early dialysis and renal transplant have been considered in some cases. Some of the abnormalities seen are of no clinical significance. However, many are potential sources of morbidity that can be reduced, especially if the problems are diagnosed and treated at an early age.
Renal anomalies include the cystic diseases as well as abnormalities of number, position, and rotation. Normal renal development depends on progression of all the stages of renal development starting with the pronephros through to normal development of the metanephros. If any stage of development is not met, there may be an aberrant genitourinary tract. We now know that many molecular agents are responsible for the gross organ development through growth and necessary apoptosis of varying stages to obtain a normal urinary tract (8,9,10,11). Renal and ureteral agenesis with absence of the ipsilateral genital ducts in the male arise if the mesonephros does not develop; if the mesonephric duct develops but the mesonephros does not, there will be renal agenesis with the genital ducts present and possibly a blind-ending ureter. In these instances, in addition to renal agenesis, there will be a congenital absence of the vas deferens where the ipsilateral mesonephric duct does not develop (12).
Normal nephrogenesis depends on the ureteral bud meeting normal metanephrogenic blastema (13). If the ureter fails to meet the metanephric blastema, a blind-ending ureter might result. When the ureter meets a degenerating portion of the metanephrogenic blastema (i.e., the cephalic or caudal end of the blastema), renal dysplasia may result (13).
Renal Agenesis
Renal agenesis can be unilateral or bilateral. Bilateral renal agenesis obviously is incompatible with extrauterine life. There is no in utero urine production with bilateral renal agenesis, which markedly decreases amniotic fluid, and the affected fetus may exhibit the deformational changes of Potter syndrome (14). Adequate amniotic fluid is also required for normal lung development so lungs are generally hypoplastic. The incidence of bilateral renal agenesis is roughly 1 in 4,000 to 5,000 births (14). Renal agenesis may be associated with sirenomelia (14). Bilateral renal agenesis can be diagnosed antenatally by a combination of sonographic findings that include lack of identifiable renal masses, no demonstrable renal vessels on Doppler imaging, absent bladder, and severe oligohydramnios (6). Interestingly, some infants with this diagnosis have normal or near-normal levels of amniotic fluid. Renal agenesis must be considered postnatally when Potter facies (Fig. 40.2) are noted, when there is no urinary output within 24 to 48 hours, or when there is evidence of ventilatory failure with hypoplastic lungs on chest radiographs. Postnatally, this diagnosis can be inferred ultrasonographically by the absence of identifiable kidneys or renal vessels with Doppler and the absence of urine in the bladder. Renal scintigraphy is used to prove that there is no identifiable functioning renal tissue. When the postnatal diagnosis of bilateral renal agenesis is made and confirmed, attempts at life support, which may have been initiated because of respiratory distress, should, in our opinion, be abandoned. There may be a familial inheritance of bilateral renal agenesis, with one review reporting up to 3% of siblings of probands having bilateral renal agenesis (15).
Unilateral renal agenesis incidence is roughly 1 in 500 to 1,500 (14,16). An associated higher incidence of contralateral renal abnormality, usually obstructive or refluxing, in patients with unilateral renal agenesis occurs when compared to the general population. One-third of the patients with a solitary kidney in one series required some form of surgical procedure on that solitary unit (17). Unilateral renal agenesis may be associated with congenital scoliosis and also with vaginal and uterine agenesis (18,19) (Fig. 40.3). It is the most common nonskeletal anomaly seen with imperforate anus (20). Unilateral renal agenesis is not thought to affect longevity or health as long as the contralateral kidney is normal. Studies in rodents have suggested that hyperfiltration produced by the solitary kidney may cause long-term renal injury and that a reduced protein diet may be somewhat protective (21). However, clinical studies of patients with a solitary kidney (e.g., transplant donors, trauma victims) have failed to confirm this (22).
Brenner et al. have noted that most people with unilateral renal agenesis do not develop progressive renal disease. However, longstanding hyperfiltration in people with a solitary kidney from any etiology could cause glomerular hypertension, which might then be the culprit for developing progressive glomerular damage with subsequent proteinuria and renal insufficiency (22). Goldfarb et al. (23) reviewed renal function in donor nephrectomy patients and found that renal function was well preserved in most donors over a prolonged follow-up averaging 25 years with some increase in proteinuria found in some patients but with only marginal significance in the group as a whole. Muzaale et al. (24) showed that there was slight increase in the incidence of end-stage renal disease (ESRD) in kidney donors when compared over 15 years to healthy nondonors, but the overall risk of ESRD in donors was only 30.8/10,000.
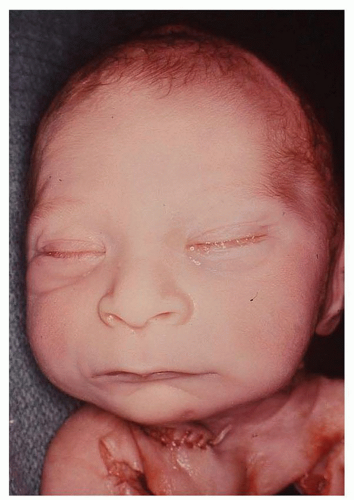 FIGURE 40.2 Potter facies, found in stillborn infant with bilateral renal agenesis, due to compression of fetus from absence of amniotic fluid. |
It has been postulated that chronic hypertension and renal disease is associated with low-birth-weight infants (LBW), primarily due to prematurity and intrauteral growth restriction (IUGR).
Because these infants are born before a full complement of nephrons can form, they may be “programmed” to have lower than expected numbers of nephrons with associated abnormal renal development and function. These premature LBW or IUGR infants may have a higher association of developing hypertension and renal disease when they become adults (25).
Because these infants are born before a full complement of nephrons can form, they may be “programmed” to have lower than expected numbers of nephrons with associated abnormal renal development and function. These premature LBW or IUGR infants may have a higher association of developing hypertension and renal disease when they become adults (25).
Renal Ectopia and Fusion
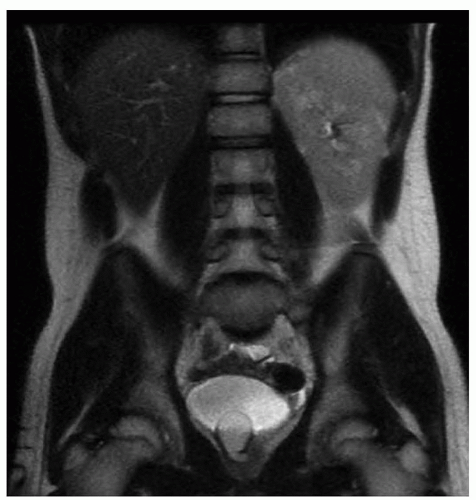
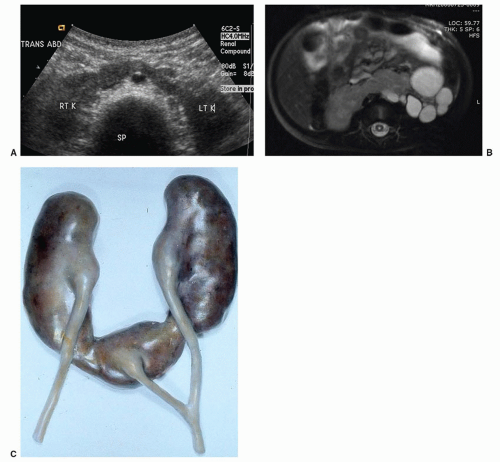
Failure of renal ascent will result in a pelvic kidney and may also be associated with vaginal or vertebral anomalies (18). If the two metanephrogenic masses come into contact with each other in the pelvis, they could fuse and form a pancake or a horseshoe kidney (26) (Fig. 40.4A-C). Horseshoe kidneys are found with increased frequency in girls with Turner syndrome (27). There is also an increased incidence of ureteropelvic junction obstruction (UPJO) in horseshoe kidneys (26). Some patients with horseshoe kidneys may have increased stone formation, as a result of relative urinary stasis with drainage from the nondependent renal pelvis.
The embryogenesis of crossed ectopia, with or without fusion, is harder to explain but might result from lateral bending and rotation of the tail bud of the embryo, thereby altering the course of ascent (19). When crossed ectopia occurs, the left kidney more commonly crosses to the right side than vice versa (28). There is an increased incidence of vesicoureteral reflux (VUR) and of UPJO in crossed ectopic kidneys (26). Patients with crossed ectopia have an increased incidence of skeletal and cardiac abnormalities (19).
Renal malrotation, or incomplete rotation, occurs when the ascending kidney maintains its early fetal (anterior-posterior) orientation with the renal pelvis remaining anteriorly directed. Malrotation is present in fusion anomalies as well as in pelvic and crossed ectopias, but it is also occasionally seen in kidneys located in the renal fossa. Incomplete rotation is of no clinical significance but may make imaging study interpretation difficult and should be considered when planning reconstructive procedures.
Abnormalities of renal position (i.e., ectopia) are interesting anomalies but are generally of no clinical import and may only become apparent after renal trauma (i.e., hematuria), a palpable mass, or some associated urologic abnormality. The ectopic kidney may be located in the chest or the pelvis. Thoracic kidneys usually are associated with eventration of the diaphragm and are of no
clinical significance except as a finding on a chest radiograph (29). Pelvic ectopia is the most common of the position abnormalities and often is associated with VUR or UPJO (26). Girls with müllerian anomalies also have an increased incidence of pelvic kidney compared to the general population; hence, the finding of a pelvic kidney in a girl warrants further investigation of the genital tract to uncover associated anomalies (30).
clinical significance except as a finding on a chest radiograph (29). Pelvic ectopia is the most common of the position abnormalities and often is associated with VUR or UPJO (26). Girls with müllerian anomalies also have an increased incidence of pelvic kidney compared to the general population; hence, the finding of a pelvic kidney in a girl warrants further investigation of the genital tract to uncover associated anomalies (30).
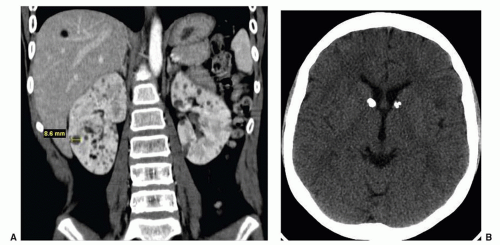
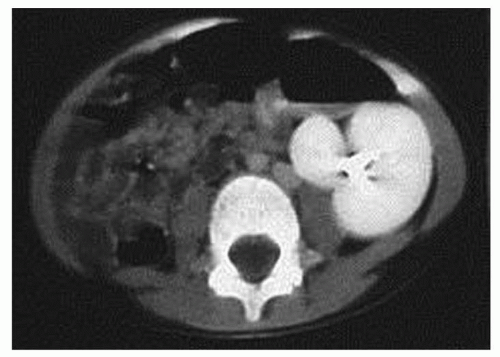 FIGURE 40.5 CT scan of supernumerary kidney on the left (smaller, medial segment). Docimo SG, Canning DA, Khoury A, eds. Clinical pediatric urology. London: Informa Publishers, 2007:289, Chapter 19, Fig. 19.6I. |
Supernumerary Kidney
The presence of a supernumerary (i.e., third) renal mass is a very rare anomaly; the clinical significance of this is determined by associated pathologic conditions (31). The supernumerary kidney usually is small and more often caudal than cranial to the normally placed kidney. Many patients and some physicians confuse a supernumerary kidney with duplication of the collecting system and incorrectly refer to ureteral duplication as a third kidney (Fig. 40.5).
Cystic Disease
Renal cystic diseases are a group of disorders that frequently present in the neonatal period and are increasingly diagnosed with antenatal ultrasonography. Table 40.1 is a classification scheme that has been clinically useful for accurate diagnosis of these conditions for prognosis and for genetic counseling.
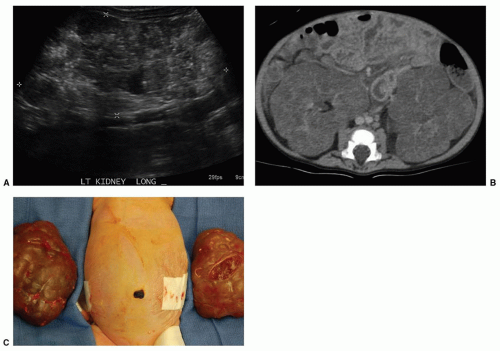
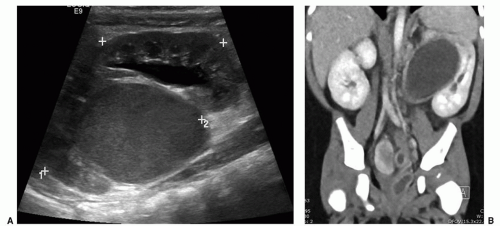
Autosomal recessive polycystic kidney disease (ARPCKD), as the name implies, is an inherited disorder whose mode of transmission follows an autosomal recessive pattern. Its reported incidence is between 1 in 6,000 and 1 in 14,000 pregnancies. These kidneys are very large and often occupy the entire retroperitoneum (Fig. 40.6A-C). The cysts are small and are actually enlargements of the collecting ducts (32). The liver almost always is abnormal. At times, there will be periportal hepatic fibrosis as a significant part of this complex. Death in the neonatal period is secondary to either renal or pulmonary failure. Pulmonary failure can be reversed by removing both kidneys so that the lungs can expand. If this is done using an experitoneal approach, peritoneal dialysis can be used to maintain homeostasis until the child can receive a renal transplant. Those who survive the neonatal period without the need for nephrectomy usually will exhibit decreased renal function and hypertension, but at times, liver failure as a result of hepatic fibrosis may be the most prominent part of the clinical picture (33). Some of these children may be considered for transplantation of the most affected organs as many are surviving past infancy with improved medical care. Imaging studies, including antenatal or postnatal ultrasonography and CT, usually are diagnostic with very large kidneys demonstrating a sunburst streaking pattern or small echodense or “bright” cystic kidneys.
TABLE 40.1 Classification of Renal Cystic Disease | ||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||
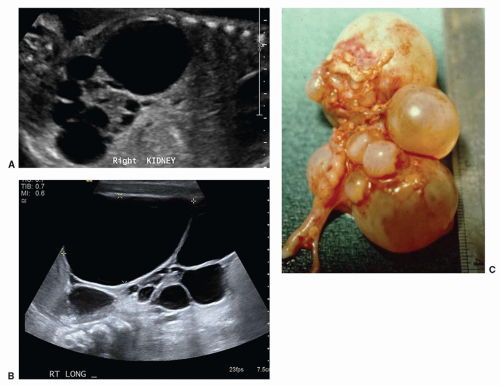
Autosomal dominant polycystic kidney disease (ADPCKD) is inherited in a dominant fashion and is obviously more common than the recessive form. Typically, it presents in adult life but is now being diagnosed at early ages due to improved imaging techniques. Presenting symptoms with this disorder include hypertension, hematuria, urinary tract infection (UTI), or renal failure. When this problem is found in childhood, it may present as an abdominal mass or may be found with ultrasound as an antenatal evaluation, screening for polycystic disease, or coincidentally when an ultrasound is obtained for some other evaluation. Imaging studies are diagnostic when multiple large cysts are found that splay and distort the collecting (Fig. 40.7A and B). There often are associated hepatic cysts, but liver failure is not usually found in this disorder. Microdissection studies have shown that the cysts are as a result of abnormal branching of the collecting tubules and cystic dilations of portions of the nephron (34). Generally, detectable cysts may not develop until middle to late adult life; hence, the disease is undetectable clinically until they appear.
Tuberous sclerosis can mimic both autosomal recessive and autosomal dominant polycystic disease in that lesions grossly similar to either form of polycystic disease can be found in the tuberous sclerosis complex (35) (Fig. 40.8A and B). Microscopically, lesions characteristic of tuberous sclerosis will be seen on biopsy of the affected kidneys. Angiomyolipomas (i.e., renal hamartomas) are the more commonly seen renal lesions in patients with tuberous sclerosis.
Multicystic dysplastic kidney (MCDK) disease, with a frequency of 1 in 3,000 pregnancies (17), is the most common form of cystic disease seen in neonates. Originally defined by Spence et al. (36), this may be a unilateral (or bilateral) lesion where the entire kidney or part of the kidney is replaced by cysts of varying sizes. Grossly, there is no recognizable renal tissue present, but microscopically, there may be dysplastic renal elements in the septa between the cysts (Fig. 40.9A-C). Bilateral multicystic kidney disease, like bilateral renal agenesis, is incompatible with life. MCDK is sporadic and is not inherited. Some multicystic kidneys involute, probably by absorption of the cyst fluid. Involution can occur antenatally or in the first few months of life but may take many years to completely resolve. Some cases of presumed renal agenesis may be
involuted multicystic kidneys. Multicystic kidneys are increasingly detectable with antenatal ultrasonography, sometimes early in gestation, but occasionally may still present during infancy as palpable masses. Ultrasonography will demonstrate multiple, variably sized cysts in a random pattern (Fig. 40.9A and B), and the affected kidney is generally without function on renal scan.
involuted multicystic kidneys. Multicystic kidneys are increasingly detectable with antenatal ultrasonography, sometimes early in gestation, but occasionally may still present during infancy as palpable masses. Ultrasonography will demonstrate multiple, variably sized cysts in a random pattern (Fig. 40.9A and B), and the affected kidney is generally without function on renal scan.
A great deal of controversy still exists surrounding the management of these lesions. Traditionally, nephrectomy has been performed. Many pediatric urologists now advocate observation because the incidence of sequelae such as infection, pain, hypertension, or malignancy is very low. At the present time, a Multicystic Kidney Registry is collecting data on cases that are followed with observation.
Roughly 25% of the patients with multicystic kidney disease have either a refluxing or an obstructive lesion such as UPJO on the contralateral side, which will determine the patient’s ultimate prognosis. Since the inception of the Multicystic Kidney Registry, VUR has been found to be more common than is obstruction. Up to 50% of those followed for 3 to 5 years had no change in the multicystic kidney appearance on ultrasound although involution may occur (37). As VUR was only found in 21% to 26% in two studies with the reflux being low grade, routine VCUG in this group may not be indicated unless another indication for VCUG exists (38,39).
Roughly 25% of the patients with multicystic kidney disease have either a refluxing or an obstructive lesion such as UPJO on the contralateral side, which will determine the patient’s ultimate prognosis. Since the inception of the Multicystic Kidney Registry, VUR has been found to be more common than is obstruction. Up to 50% of those followed for 3 to 5 years had no change in the multicystic kidney appearance on ultrasound although involution may occur (37). As VUR was only found in 21% to 26% in two studies with the reflux being low grade, routine VCUG in this group may not be indicated unless another indication for VCUG exists (38,39).
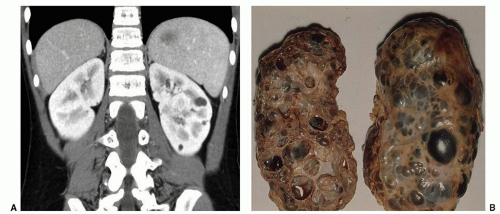 FIGURE 40.7 A: CT scan confirming ADPCK (autosomal dominant polycystic kidney) disease of young child with prior ultrasound demonstrating small cysts in both the kidneys. B: Gross specimen of ADPCKs. |
▪ ANOMALIES OF THE URETERS AND BLADDER
Duplication and Triplication of the Ureters
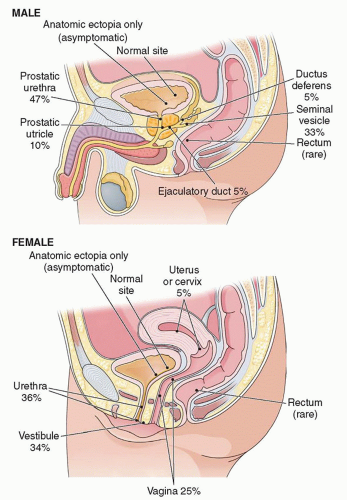
Multiple ureteral buds or premature division of the ureteral bud could produce ureteral duplication or triplication (40). If there are multiple ureteral buds, one bud is likely to meet degenerating rather than normal nephrogenic tissue thus accounting for the increased incidence of renal dysplasia in the upper pole of duplicated systems (4). Duplication of the urinary collecting system is one of the more common abnormalities seen in the urinary tract; its occurrence is about 0.8% (40). Approximately 12% of sibs and parents were affected with ureteral duplication when reviewing family inheritance probands (15). Duplication can be either complete or incomplete. Incomplete duplication is usually of no clinical significance, although there can be ureteroureteral reflux between the two limbs of the partial duplication resulting in dilation of one of the ureters, usually the lower one. Complete duplication occurs once in every 500 cases (40). Complete duplication is generally of no clinical significance but is associated with a higher incidence of VUR and obstruction.
VUR probably is more common with ureteral duplication and usually occurs into the lower moiety of the duplicated system (Figs. 40.10A-C and 40.11). Duplication is seen in approximately one in five people with VUR, having a much higher incidence than
in the general population (41). The grade of reflux associated with a complete duplication usually is higher than that seen with a single system. Obstruction is more common when the upper moiety of a complete duplication is abnormal. Both obstruction and VUR associated with duplications may present as either mass lesions or urosepsis. Many of these duplications are diagnosed in utero because hydronephrosis is seen in the upper or lower segments of the duplicated systems using ultrasonography.
in the general population (41). The grade of reflux associated with a complete duplication usually is higher than that seen with a single system. Obstruction is more common when the upper moiety of a complete duplication is abnormal. Both obstruction and VUR associated with duplications may present as either mass lesions or urosepsis. Many of these duplications are diagnosed in utero because hydronephrosis is seen in the upper or lower segments of the duplicated systems using ultrasonography.
If the ureteral bud arises more cranially or caudally than normal, ureteral ectopia, VUR, or paraureteral diverticula might be produced (42) (Figs. 40.12A-E and 40.13). Ectopic ureteroceles probably result from abnormalities of the ureteral bud and ureteral ectopia (43) (Fig. 40.14A-C). Simple ureteroceles are thought to be produced by persistence of the Chwalla membrane (the membrane covering the distal end of the ureter during development) (44).
Ureteral obstruction, when present, usually occurs either at the ureteropelvic or at the ureterovesical junction but may also rarely occur in the mid to distal ureter. These obstructions usually are intrinsic in nature, and the ureter may be of normal or reduced caliber externally (45,46). Multicystic kidney disease may be secondary to ureteral obstruction early in gestation or due to disordered induction of the metanephrogenic mass by a faulty ureteral bud as previously discussed (47). Kitagawa et al. (48) developed an animal model for producing a multicystic kidney by obstructing the fetal lamb urethra (male) or ureter (female) at 60 days of gestation; they proposed that the cysts developed only when the obstruction occurs after the glomeruli start to produce urine.
Bladder Anomalies
Agenesis of the bladder could result if the allantoic stalk failed to develop (49); it also could occur if there is bilateral failure of ureteral migration with resultant bilateral ureteral ectopia, since migration of the ureters is necessary for formation of the trigone, which, in turn, may be necessary for enlargement of the allantoic stalk (50). Urachal anomalies occur because of a general mesodermal failure, as in the triad or prune belly syndrome (PBS), or because of delayed closure of the urachus (51) (Fig. 40.15). Duplications of the bladder and urethra often are associated with duplications of the hindgut and lower spinal cord. It would then seem that splitting of the hind end of the embryo might be responsible for this type of anomaly (52).
Posterior urethral valves (PUVs) probably result from abnormal insertion and persistence of the mesonephric ducts distal to the müllerian tubercle (type I), or from persistence of the cloacal membrane (type III) (53). Type II valves probably do not exist as an obstructing lesion (see Fig. 40.23).
Ureteral Ectopia
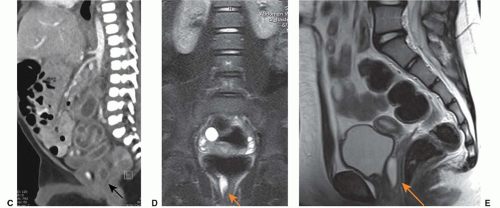
Ureteral ectopia exists when the ureter opens in a position other than its normal location at the corner of the trigone. Ectopia may occur in ureters of single or duplex kidneys (Fig. 40.12A-E). The most common form of ureteral ectopia is lateral ureteral ectopia, in which the ureteral orifice lies within the bladder lateral to its normal position. This is the etiologic mechanism for primary VUR (see “Vesicoureteral Reflux”). Significant medial or distal ureteral
ectopia, less common than lateral ureteral ectopia, may cause variable clinical pathologic conditions depending on the location of the ureteral orifice and the gender of the patient. An abnormal proximal budding locus of the ureteral bud on the mesonephric duct allows the ureteral bud to remain in prolonged contact with the wolffian duct, so that the medially ectopic ureteral orifice may open anywhere along the course of the wolffian duct (Fig. 40.13). In males, this includes the posterior urethra, seminal vesicles, vas deferens, or epididymis (54). In females, the ectopic ureter may open into the urethra, the uterus, or proximal vagina, or along the course of Gartner duct in the anterolateral wall of the vagina. If a medially ectopic ureter opens within the confines of the bladder, no clinical abnormality occurs. If the ureter opens at the bladder neck location, obstruction of the involved renal unit or VUR may occur.
ectopia, less common than lateral ureteral ectopia, may cause variable clinical pathologic conditions depending on the location of the ureteral orifice and the gender of the patient. An abnormal proximal budding locus of the ureteral bud on the mesonephric duct allows the ureteral bud to remain in prolonged contact with the wolffian duct, so that the medially ectopic ureteral orifice may open anywhere along the course of the wolffian duct (Fig. 40.13). In males, this includes the posterior urethra, seminal vesicles, vas deferens, or epididymis (54). In females, the ectopic ureter may open into the urethra, the uterus, or proximal vagina, or along the course of Gartner duct in the anterolateral wall of the vagina. If a medially ectopic ureter opens within the confines of the bladder, no clinical abnormality occurs. If the ureter opens at the bladder neck location, obstruction of the involved renal unit or VUR may occur.
In females, ectopic ureteral orifices located distal to the internal sphincter mechanism of the bladder neck can cause incontinence (55). Older girls usually present with constant urine leak or dampness that is associated with an otherwise symptom-free, normal voiding pattern. Infant girls may be constantly wet, have a persistent diaper rash, or have a purulent vaginal discharge if the system becomes infected. Physical examination suggests the diagnosis if urine can be seen welling up in the vagina or if a spurt of urine is seen coming from the perineal ectopic ureteral orifice. Many ectopic ureters are not diagnosed by physical findings alone. Eighty percent of these ectopic ureters arise from the upper pole segment of a total ureteral duplication. Ultrasonography may suggest a duplicated system with ureteral ectopia, but frequently, CT or MR imaging may be necessary to define the ectopic ureteral anatomy. An ectopic segment may be visible on CT or excretory urography, but it frequently functions poorly and may not be visible on this type of imaging even with delayed radiographs. A high index of suspicion and an awareness of radiographic clues to a nonvisible duplication such as a “drooping lily” collecting system often will lead to the diagnosis. Because an ectopic vaginal ureter may drain a poorly functioning, nonvisualized, single renal unit, congenital absence of one kidney in a girl with incontinence requires a thorough investigation to prove that there is not a contralateral but poorly functioning kidney with an ectopic orifice. Investigation should include abdominal sonography and nuclear renal scan, but CT or MRI may be the only way to define the anatomy (56). Renal
scintigraphy using dimercaptosuccinic acid may find a functioning renal unit, but MRI may better delineate the anatomic details of a small poorly functioning ectopic kidney.
scintigraphy using dimercaptosuccinic acid may find a functioning renal unit, but MRI may better delineate the anatomic details of a small poorly functioning ectopic kidney.
Treatment of the ectopic ureter depends on the presence or absence of significant function in the involved renal unit. If the ureter drains an otherwise healthy system, ureteral reimplantation into the bladder will correct the problem and preserve maximal renal function. If the ureteral anomaly is associated with a duplex kidney, ipsilateral ureteroureterostomy may be performed whether or not there is good function in both segments of the kidney. Alternatively, excision of the involved segment may be performed if the involved renal unit functions poorly, but generally, this is not needed unless recurrent infection can be localized to the poorly functioning segment. The distal ureteral stump is left undisturbed to avoid compromise of the normal sphincter continence mechanism. Male infants with an ectopic ureter frequently present with antenatal ultrasound findings suggestive of ureteral dilatation, an abdominal mass, UTI, or epididymitis (54). In boys, an ectopic ureter will arise more frequently from a nonduplicated kidney and may drain into the male genital tract anywhere from the prostatic urethra to the epididymis. Treatment is similar to that for females.
Ureterocele
A ureterocele is a cystic dilation of the distal submucosal or intravesical portion of a ureter. Ureteroceles account for a broad spectrum of associated or secondary pathologic conditions and constitute one of the more complex and confusing groups of anomalies of the lower urinary tract (57).
Ureteroceles in children most commonly involve the intravesical end of the upper pole ureter of a duplex kidney (i.e., ectopic ureterocele) but may less commonly involve a single-system ureter (i.e., simple ureterocele) (58). Although simple ureteroceles involving a single system are common in adults, they are rare in children; conversely, ectopic ureteroceles are the more commonly seen ureteroceles in infants and children. The etiology of ureteroceles is uncertain. Failure of reabsorption of the Chwalla membrane from over the ureteral orifice has been proposed as an obstructive etiology
(44). It seems more likely that ureteroceles result from an intrinsic defect in the ureteral bud itself and from faulty or delayed incorporation of the ureteral bud into the urethra and bladder base (55).
(44). It seems more likely that ureteroceles result from an intrinsic defect in the ureteral bud itself and from faulty or delayed incorporation of the ureteral bud into the urethra and bladder base (55).
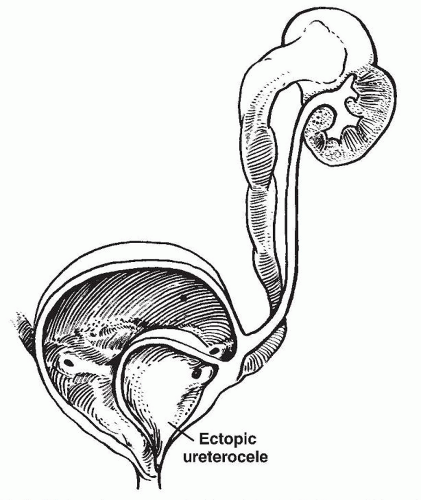 FIGURE 40.15 Ectopic ureterocele. From Malek RS, Kelalis PP, Burke EC, et al. Simple and ectopic ureterocele in infancy and childhood. Surg Gynecol Obstet 1972;134:611, with permission. |
Ureteroceles associated with a single-system ureter (i.e., simple ureteroceles) tend to be intravesical, in the normal position, and are more likely to be found in boys. Intravesical ureteroceles in children may also be associated with hydronephrosis of the affected renal unit (59).
Ureteroceles may be associated with significant derangement of the upper and lower urinary tract. The ureterocele originating from the upper pole ureter of a duplex kidney is associated with secondary pathology, generally, hydronephrosis, with impaired function or dysplasia of the upper pole system and often obstruction or reflux in the ipsilateral lower pole system (Fig. 40.14A-C). Contralateral reflux or obstruction also may occur. The pathophysiology of the associated findings is easily understood by recognizing that the ureterocele may dissect under the trigonal epithelium and deform the ipsilateral or contralateral ureterovesical junction, causing the various combinations of VUR or obstruction in any or all of the ureters (60). Ten percent of ureteroceles occur bilaterally (57). A ureterocele prolapsing into the bladder neck or urethra may occlude the bladder outlet causing bilateral hydronephrosis and relative bladder outlet obstruction with urinary retention or infection (Fig. 40.15).
Ureteroceles occur more commonly in females and usually manifest in early childhood; the ratio of occurrence in males and females is 1:6 cases (57). Now, most cases of ureterocele are diagnosed antenatally with ultrasound, but, historically, the most common presentation was that of a febrile infant found to have a UTI. If the ureterocele prolapses into the urethra, difficult voiding or azotemia may prompt evaluation. Ureterocele is the most common cause of urinary retention in the female infant. Rarely, a ureterocele will prolapse through the external urethral meatus in a female and present as an introital mass.
Classically, the diagnosis of a ureterocele is fairly straightforward. Renal and bladder ultrasonography will reveal the upper tract dilation and the wall of the ureterocele in the bladder (61). This can be seen antenatally. Voiding cystography (VCUG) is necessary to establish the presence or absence of associated VUR, potential obstruction of the bladder neck, and to assess the integrity of the detrusor muscle backing the ureterocele. A diuretic renal scan can outline the function of the involved upper pole segment and any measurable obstruction of any of the segments, and consequently can be helpful in determining the best surgical approach.
The choice of treatment for ureteroceles depends on several factors. The age and clinical condition of the patient, the presence or absence of significant function in the involved nephroureteral unit, and the presence of reflux or obstruction in the ipsilateral or contralateral uninvolved ureters all influence the choice of therapy. In the critically ill, septic infant, transurethral or transvesical unroofing or puncture of the ureterocele may provide decompression and allow stabilization of the child until his or her clinical condition allows definitive treatment. Alternatively, placement of a temporary percutaneous nephrostomy into the involved renal unit often can be done without the need for general anesthesia. The best form of definitive treatment has been debated over the years and continues to be a source of debate.
Most intravesical single-system ureteroceles do not require any surgical treatment. If an intravesical ureterocele associated with a single kidney is a source of infection and is obstructing the kidney or bladder neck, simple excision of the ureterocele and reimplantation of the involved ureter should resolve those problems caused by the ureterocele. Cystoscopic puncture of the ureterocele may also correct the problem without need for further surgical intervention, particularly in single-system intravesical ureteroceles (62). If the intravesical ureterocele involves duplex ureters, an en bloc ureteral reimplantation can be performed if the ureters are not too dilated (57).
Treatment options have included various combinations of partial nephrectomy, ureterectomy, marsupialization or excision of the ureterocele, ureteroneocystostomy, and ureteroureterostomy. Cystoscopic puncture of the ureterocele may occasionally correct the problem without need for further surgical intervention (62).
Ureteropelvic Junction Obstruction
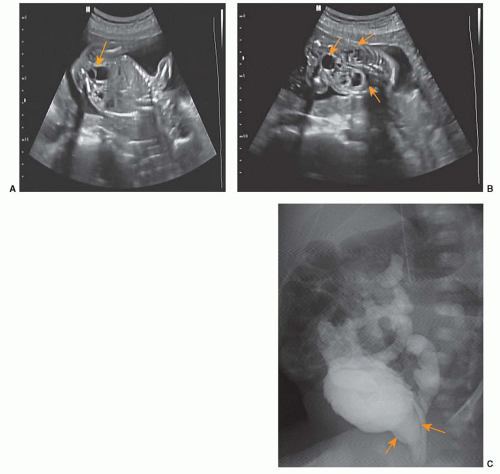
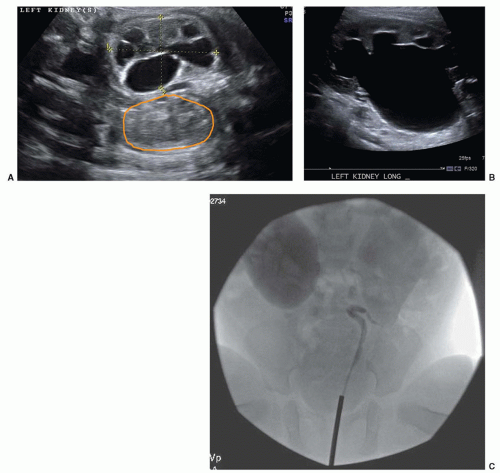
Obstruction at the ureteropelvic junction probably is the most common cause of a palpable abdominal mass in the newborn and is the most common cause of antenatal hydronephrosis requiring surgical treatment. This lesion usually is the result of narrowing of the ureter at the junction of the renal pelvis with the ureter. Because the renal pelvis is compliant, there can be a great deal of renal preservation despite massive dilation of the kidney behind the obstruction (Fig. 40.16A-D) (63).
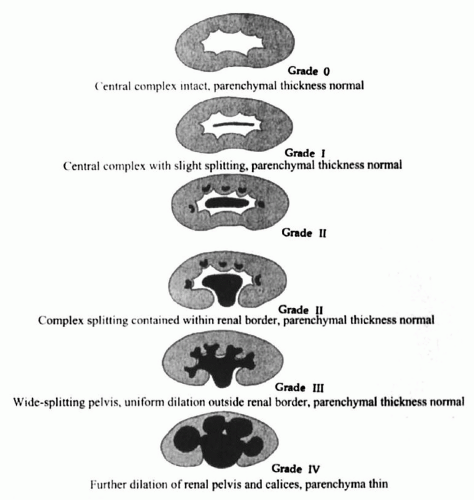
Diagnosis of UPJO can be detected sonographically because there is a sonolucent central mass within the renal area surrounded by thin renal parenchyma (Fig. 40.16A-D). A grading system has been suggested by the Society for Fetal Urology to better standardize terminology and interpretation of renal ultrasound findings (64). The system is based on the severity of renal pelvis and calyceal dilatation and the renal parenchymal thickness (Fig. 40.17). VUR should be excluded from the differential diagnosis using voiding cystography. The relative function of the obstructed kidney should be determined by radionuclide scanning (Fig. 40.16D). One of the advantages of radionuclide scintigraphy is that the physiologic significance of dilatation can be determined by administering furosemide (65). If the dilatation is of significance, there will be retention of the radionuclide behind the obstruction, whereas if there is no physiologic significance to the hydronephrosis, the administered diuretic will cause the radionuclide to wash out rapidly from the dilated system. To obtain valid results, the infant or young patient must be adequately hydrated and have adequate bladder drainage to prevent false interpretation of obstruction on the scan as a result of dehydration or bladder distention (66). In many instances, hydronephrosis in the newborn is physiologically insignificant, and
those cases that are physiologically insignificant will stabilize or improve with time and require no treatment. Obstructive hydronephrosis at the ureteropelvic junction requires repair, generally dismembered pyeloplasty, which may be performed with open or laparoscopic techniques resulting in improved drainage and occasionally improved renal function (63). Robotic pyeloplasty procedures are becoming more common but generally are difficult and not indicated in an infant or young child due to their small size.
those cases that are physiologically insignificant will stabilize or improve with time and require no treatment. Obstructive hydronephrosis at the ureteropelvic junction requires repair, generally dismembered pyeloplasty, which may be performed with open or laparoscopic techniques resulting in improved drainage and occasionally improved renal function (63). Robotic pyeloplasty procedures are becoming more common but generally are difficult and not indicated in an infant or young child due to their small size.
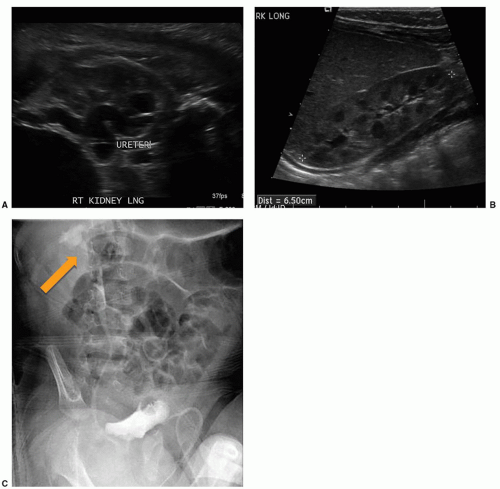
Ureterovesical Obstruction
Obstruction at the ureterovesical junction is not nearly as common as is obstruction at the ureteropelvic junction (46). Lower ureteral obstruction may present as marked hydroureteronephrosis (i.e., a mass) but may sometimes present as urinary infection (Fig. 40.18A and B). As with ureteropelvic obstruction, it has become apparent that not all presumed ureterovesical obstructions are physiologically significant and some require no treatment. VCUG is recommended to evaluate for vesicourinary reflux or other bladder pathology. Radionuclide scanning with diuretics may help diagnose physiologic obstruction (65). MRI with intravenous contrast may be necessary to better define the anatomy and possible area of obstruction in cases of lower ureteral obstruction. At times, however, an antegrade pyelogram with a pressure perfusion study is necessary to determine the significance or lack of significance of an apparent narrowing at the ureterovesical junction (67). These lesions, if identified as obstructive, are treated by excision of the obstructing segment, tailoring or tapering of the dilated ureter, and reimplantation of the ureter into the bladder (68). Recently, balloon dilation of the obstructed distal ureter with ureteral stenting with one or two stents has been advocated for surgical correction of lower urinary tract obstruction, but the long-term results of this technique are not well known, and significant morbidity could be associated with the technique (69).
Vesicoureteral Reflux
VUR is the most common abnormality of the urinary system seen in children; it may occur in 1 of 100 births (70). The actual incidence is unknown, but it is at least as common as cryptorchidism or
hypospadias. Genome mapping, performed on families with primary VUR who also have associated reflux nephropathy, has found an association with a locus on chromosome 1, which is also seen in some families with VUR (71). VUR is known to be a familial problem. When one child in a family is identified as having reflux, as many as 30% to 50% of the siblings of that child may have VUR (72). Recently, the American Urological Association (AUA) published VUR guidelines and found in their meta-analysis that VUR occurs in about 27.4% of siblings and 35.7% in offspring of children with reflux. Screening of all siblings or offspring of children with VUR, as was done in the past, does not seem warranted unless the child to be screened has had a history of UTI, especially febrile, or an abnormal renal bladder ultrasound (73). The normal ureterovesical junction is an efficient mechanism that allows egress of urine into the lumen of the bladder and prevents the bladder urine from reentering the ureter because of its oblique course through the bladder wall (Fig. 40.19) (74). It is obvious that there is maturation of the ureterovesical junction with both time and patient growth, as infants have a much higher incidence of VUR than do older children (75).
hypospadias. Genome mapping, performed on families with primary VUR who also have associated reflux nephropathy, has found an association with a locus on chromosome 1, which is also seen in some families with VUR (71). VUR is known to be a familial problem. When one child in a family is identified as having reflux, as many as 30% to 50% of the siblings of that child may have VUR (72). Recently, the American Urological Association (AUA) published VUR guidelines and found in their meta-analysis that VUR occurs in about 27.4% of siblings and 35.7% in offspring of children with reflux. Screening of all siblings or offspring of children with VUR, as was done in the past, does not seem warranted unless the child to be screened has had a history of UTI, especially febrile, or an abnormal renal bladder ultrasound (73). The normal ureterovesical junction is an efficient mechanism that allows egress of urine into the lumen of the bladder and prevents the bladder urine from reentering the ureter because of its oblique course through the bladder wall (Fig. 40.19) (74). It is obvious that there is maturation of the ureterovesical junction with both time and patient growth, as infants have a much higher incidence of VUR than do older children (75).
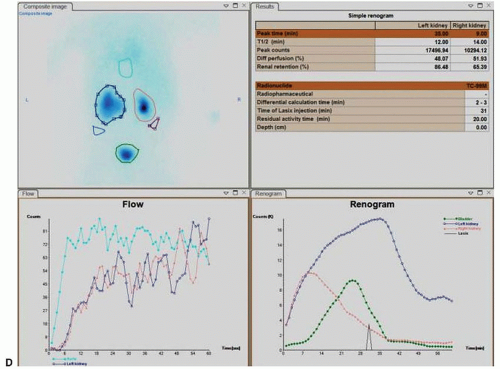 FIGURE 40.16 (Continued ) D: Renal scan (different patient) demonstrating relative function in both the kidneys and probably obstruction in the left kidney (see arrows). |