Splinting Procedures
Jean E. Klig
Introduction
Orthopaedic immobilization techniques utilize a wide range of devices to support musculoskeletal injuries. Splints are an essential part of this spectrum and are vital to the initial management of many injuries in children (1). The goal of splinting is to provide support at key points around an injury to allow for (a) decreased pain; (b) mechanical stabilization of bones, soft tissues, and neurovascular structures; (c) decreased risk of further injury to the affected area; and (d) decreased risk of additional swelling-related injuries such as a compartment syndrome. Splints are extremely versatile and can be used either for initial injury care or as definitive treatment in certain cases. They are commonly used for the early treatment of nondisplaced closed fractures in children. In the 24 to 48 hours after an injury, a splint provides support and immobilization as well as allowing the injured extremity to swell without significant risk of external compression. In contrast, a cast often allows little room for swelling and must be promptly opened when this occurs.
A splint can be used for up to 2 weeks following a nondisplaced closed fracture, after which a cast usually is applied. Use of a splint also offers a valuable temporizing measure with equivocal injuries initially diagnosed as joint sprains. In children, an acute “sprain” of any joint where an epiphysis is known to be unfused can in fact represent a nondisplaced Salter-Harris type I fracture, even when radiographs are unremarkable. It is therefore common practice to initially treat sprains in children as nondisplaced fractures, utilizing a splint until follow-up examination and/or radiographs are obtained. For older adolescents with closed epiphyses, splints may be used as definitive treatment for more severe joint sprains. The overall rule of “when in doubt, splint” is key to the treatment of many pediatric musculoskeletal injuries (2).
The splinting methods detailed in this chapter can be used for children of all ages and are appropriate for prehospital, emergency and ambulatory settings. Splint techniques can be performed by many types of skilled medical personnel.
Anatomy and Physiology
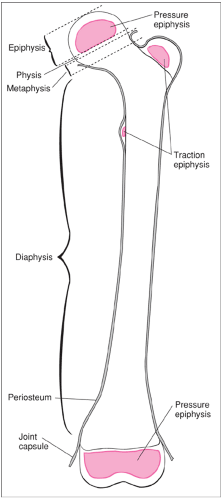
Pediatric fractures differ greatly from those seen in adults, because the bones of a child are in a continual process of growth. A growing long bone has four anatomical parts: physis, epiphysis, metaphysis, and diaphysis (Fig. 101.1). Growth occurs in two regions. Increases in bone length occur at the growth plate (physis) via endochondral ossification, while increases in bone width occur at the periosteum by membranous ossification. The strongest parts of a child’s bone are the periosteum and adjacent joint capsule and ligaments. By contrast, the growth plate is the weakest area of a child’s bone and is therefore most vulnerable to injury (3). As a result, children are less likely than adults to have dislocations, sprains, and strain injuries but are more likely than adults to have fractures, which commonly involve the growth plate.
Certain fractures are unique to children. The greater strength of the periosteum as compared with the underlying
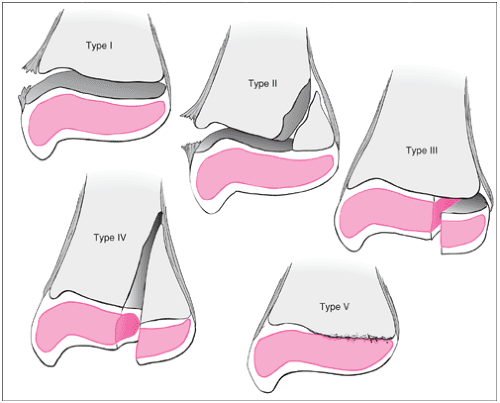
bone trabecula results in buckling (torus) fractures, bending (plastic) fractures, and fractures that extend through the bone but only disrupt one side of the periosteum (greenstick). Fractures of the growth plate, which only occur in growing children, are delineated by the Salter-Harris classification (Fig. 101.2). Five different forms of injury to the physis or growth plate region are defined by this classification. A type 1 fracture involves the zone of provisional calcification (physis) only, without fracture of the surrounding bone. A type II injury involves a slip at the epiphyseal plate with a fracture proximally through the metaphysis, while a type III involves a slip at the epiphyseal plate with a fracture distally to the articular surface of the bone. In a type IV injury, the fracture extends through the metaphysis and epiphyseal plate to the adjacent articular surface. Type V fractures are less common and involve compression of the growth plate.
bone trabecula results in buckling (torus) fractures, bending (plastic) fractures, and fractures that extend through the bone but only disrupt one side of the periosteum (greenstick). Fractures of the growth plate, which only occur in growing children, are delineated by the Salter-Harris classification (Fig. 101.2). Five different forms of injury to the physis or growth plate region are defined by this classification. A type 1 fracture involves the zone of provisional calcification (physis) only, without fracture of the surrounding bone. A type II injury involves a slip at the epiphyseal plate with a fracture proximally through the metaphysis, while a type III involves a slip at the epiphyseal plate with a fracture distally to the articular surface of the bone. In a type IV injury, the fracture extends through the metaphysis and epiphyseal plate to the adjacent articular surface. Type V fractures are less common and involve compression of the growth plate.
Two key physiologic considerations relate to use of splints for pediatric patients. First, children tend not to suffer from significant muscle stiffness or spasm due to immobilization. Use of a splint for an “equivocal” fracture in a child until the presence (or absence) of a fracture can be verified therefore poses minimal risk of complications such as musculoskeletal rigidity. Second, the dynamics of bone growth allow for significant remodeling of angulated fractures. As a result, fractures with up to 20 degrees of angulation in the plane of joint motion can often be splinted without reduction. It is generally advisable to consult an orthopaedist for fractures with over 20 degrees of angulation even though a splint may be safely used (4).
Indications
Splinting is an extremely versatile tool in the management of many pediatric extremity injuries and/or known fractures. The early diagnosis and treatment of a fractured extremity is vital to an optimal outcome in a child, given the swift rate at which pediatric bones grow and remodel. Clinical findings of a fractured extremity may include inability or reluctance to use the affected limb; pain with limb movement; reproducible bone tenderness to palpation (point tenderness); swelling, discoloration, or deformity at the fracture site; and crepitus (5).
Radiographs of the injured extremity should always be obtained when a child has positive or abnormal clinical signs. If the findings on a radiograph are unclear, then a similar view of the opposite uninjured extremity may be helpful. As mentioned previously, “negative” radiographs do not exclude the possibility of a fracture if the findings on physical examination suggest otherwise. Reproducible bone tenderness near a joint with an open epiphysis is suggestive of a Salter-Harris type I fracture and is a sufficient indication for splinting even without radiographic evidence of a fracture. Moreover, “sprains” are relatively rare in children and are commonly treated as Salter-Harris type I fractures until a follow-up assessment in 5 to 10 days (6,7).
Immediate evaluation by an orthopaedist is mandatory for any extremity fracture where signs of neurovascular compromise are present (see Chapter 106). These include extreme pain at rest, pain with passive movement, pallor, paralysis, and paresthesias. Orthopaedic consultation is also recommended for (a) open fractures, (b) elbow or femur fractures, (c)
fractures angulated greater than 20 degrees, (d) more severe Salter-Harris fractures (types III–V), and (e) unstable fractures. It is advisable to consult an orthopaedist when follow-up fracture care cannot be ensured within 2 weeks after the placement of a splint. Additionally, early placement of a temporary splint is indicated for injuries suspected to be unstable unless orthopaedic evaluation can be ensured within a brief time. In such cases, a splint can be loosely placed on the injured extremity to provide both temporary support and some pain relief, particularly during positioning for radiographs.
fractures angulated greater than 20 degrees, (d) more severe Salter-Harris fractures (types III–V), and (e) unstable fractures. It is advisable to consult an orthopaedist when follow-up fracture care cannot be ensured within 2 weeks after the placement of a splint. Additionally, early placement of a temporary splint is indicated for injuries suspected to be unstable unless orthopaedic evaluation can be ensured within a brief time. In such cases, a splint can be loosely placed on the injured extremity to provide both temporary support and some pain relief, particularly during positioning for radiographs.
Finally, splints are sometimes used in children to immobilize areas where wound healing may be impaired by motion. This includes areas with multiple complex sutures, sutures over joint areas, burns, and dirty and/or infected wounds.
Equipment
Although a wide range of prefabricated splints are available, many are not properly sized for children. Essential materials for splinting are listed below. Splints can be made with plaster, fiberglass, or prefabricated splint roll, which contains padding and fiberglass or plaster in one unit. Fiberglass is strong, durable, lightweight, and in many cases easier to apply than plaster.
Gauze roll or elastic (Ace) bandage
Cotton stocking material (stockinette)
Soft cotton roll (Webril)
Plaster roll or sheets or fiberglass roll
Commercial splint roll (optional)
Prefabricated splint (optional)
Procedures
General Principles
Guidelines for splint measurement and application are listed in Table 101.1. Most splints have four layers. A stockinette (layer 1) is placed against the skin for protection. This is optional but is often used for comfort. Webril (layer 2) is then placed around the stockinette to provide padding, especially at bony prominences (it can be omitted if commercial splint roll is used). Plaster, fiberglass, or commercial splint roll (layer 3) is
then placed to maintain the position of immobilization. An outer layer of elastic bandage (Ace wrap) or gauze wrap (layer 4) is rolled around the plaster, fiberglass or commercial splint roll to secure the splint to the limb and protect the firm layer.
then placed to maintain the position of immobilization. An outer layer of elastic bandage (Ace wrap) or gauze wrap (layer 4) is rolled around the plaster, fiberglass or commercial splint roll to secure the splint to the limb and protect the firm layer.
TABLE 101.1 Splinting Measurement and Application | ||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree