Background
Vulvodynia is a chronic vulvar pain disorder and fibromyalgia is a chronic widespread musculoskeletal pain disorder, both of unknown etiology. Association of these conditions is well documented. Intravaginal algometer measurement of tenderness to pressure applied to the pelvic floor muscles helps define vulvodynia associated with musculoskeletal factors. Women with both vulvodynia and fibromyalgia might have increased pelvic muscle pain compared to women with vulvodynia alone, defining the possible link of these 2 conditions.
Objective
We sought to: (1) correlate pain intensity during the nongenital tender point tenderness examination to pain intensity with the vaginal algometer in women with provoked vestibulodynia, and (2) determine whether subjects with provoked vestibulodynia and fibromyalgia had higher pain intensity scores with the vaginal algometer than those without fibromyalgia.
Study Design
In all, 92 subjects referred for vulvar pain were confirmed to have provoked vestibulodynia using the cotton swab test. A diagnosis of fibromyalgia was made if pain was present (numeric rating scale >1) in at least 11 sites of the 18-point nongenital tender point tenderness exam. Vaginal pain sensitivity was measured using an intravaginal pressure algometer, where 0.1, 0.3, and 0.5 kg/cm 2 forces were applied digitally in random assignment by force and location to the right and left iliococcygeus muscle regions and the posterior vaginal wall. Both tender point tenderness and algometer pain intensity were reported on a 0 (no pain) to 10 (worse pain) numeric rating scale. Correlations were computed between the composite pain intensity (total of rating scale from each pressure threshold at specified site) of nongenital and those of iliococcygeus regions and the posterior vaginal wall. Independent t tests were used to determine differences in iliococcygeus regions and the posterior vaginal algometer pain ratings and presence or absence of fibromyalgia. The significance level was at P < .05. The data were expressed as mean ± SD.
Results
A significant correlation was found between numeric rating scale pain scores on the nongenital tender point tenderness exam and algometer testing on the iliococcygeus region (r = 0.44, P < .0001) and the posterior vaginal wall (r = 0.45, P < .0001). Subjects with fibromyalgia by tender point tenderness had significantly higher iliococcygeal pain (6.14 ± 2.07 vs 3.74 ± 2.22, P = .0001) and posterior vaginal wall pain (5.67 ± 2.10 vs 3.07 ± 2.16, P < .0001) than women without fibromyalgia by tender point tenderness.
Conclusion
Women with provoked vestibulodynia who experience more severe pain with nongenital tender point palpation also experience more deep vaginal pain on pelvic exam. Those who fulfill the diagnosis of fibromyalgia show significantly more intense deep vaginal pain to palpation of iliococcygeus muscles and posterior vaginal wall. Further research using a more precise definition of fibromyalgia is necessary to confirm this relationship, but findings suggest that women with provoked vestibulodynia coexisting with fibromyalgia have greater risk of superimposed vaginal muscle pain and may be candidates for early adjunctive pelvic floor physical therapy. These findings need to be explored in women with generalized, nonprovoked vulvodynia.
Introduction
Vulvodynia is a chronic pain disorder of the vulva, occurring in the absence of relevant findings or a specific clinically identified neurologic disorder. Vulvodynia is estimated to affect 8-15% of women and has been described as the leading cause of dyspareunia in women age <50 years. Symptoms of vulvodynia may include stinging, burning, irritation, or itching. The etiology of vulvodynia is unknown, and likely multifactorial.
In 2015, a consensus vulvar pain terminology committee redefined vulvodynia as vulvar pain of at least 3 months’ duration, without clear identifiable cause, which has potential associated factors ( Table 1 ). A key objective of the new terminology introduced in 2015 was to identify potential factors associated with vulvodynia, such as genetic or hormonal factors, inflammation, musculoskeletal or neurological mechanisms, neuroproliferation, and psychosocial or structural issues. The recognition of these factors in a given patient could be used to assist in developing individualized treatment plans. For example, those women with a perceived neuropathic etiology might benefit from tricyclic antidepressants or gabapentin, whereas those with musculoskeletal factors might respond better to pelvic floor physical therapy.
| Vulvodynia Definition: vulvar pain of at least 3-mo duration, without clear identifiable cause, which may have potential associated factors Descriptors:
|
Provoked vestibulodynia (PVD), the most common subset of vulvodynia, is localized to the vaginal vestibule (entry to the vagina, including the introitus, and extending to the hymenal ring) and presents only with contact, such as from tampon insertion or intercourse. Diagnosis of PVD is based on history, physical exam (which excludes other pathology), and a positive cotton swab test, whereby pain is elicited when the vestibule is gently touched with a cotton swab at the 2-, 4-, 6-, 8-, and 10-o’clock positions. Complete evaluation should also include palpation of the levator muscles immediately inside the vagina. Pelvic floor dysfunction with hypertonicity and pain has been demonstrated in PVD patients vs controls.
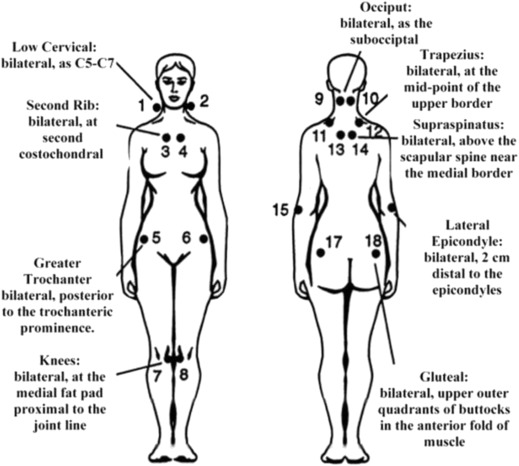
Association of vulvodynia with fibromyalgia (FMS) is well documented. FMS is a syndrome of unknown etiology, associated with chronic widespread musculoskeletal pain. FMS is diagnosed by history, absence of other identified pathology, and the presence of pain in 11 of 18 specified tender points on physical exam (tender point tenderness [TPT] exam) ( Figure 1 ). In 2010, an alternative diagnostic criterion for FMS that did not require TPT examination was developed and subsequently validated. Investigators and clinicians still disagree on the utility of the TPT exam.
The vaginal algometer is a device developed by researchers to assess pain deeper in the vagina than could be evaluated with the cotton swab test. The device consists of a probe containing a pressor sensor that is inserted into the vagina and a measurement circuit that converts the signal from the probe into a force measurement, with a resultant threshold value. The vaginal algometer was originally intended to measure pressure pain threshold (PPT) over the lateral walls of the vagina, over the area of the pudendal nerve, but has been subsequently validated in women without pain in vaginal sites including the pubococcygeus and iliococcygeus muscles, and the anterior and posterior vaginal wall. The intravaginal algometer has also been shown to assess muscle PPT independently of mucosal pain in women with vulvodynia.
The vaginal algometer may be considered a TPT examination of the vagina. In this regard, the objective of this study was to correlate ratings of pain intensity during the nongenital TPT examination to ratings of pain intensity with the intravaginal algometer in women with PVD, and to determine whether subjects with PVD and nongenital TPT scores consistent with the diagnosis of FMS had higher pain intensity scores with the vaginal algometer compared to those without FMS.
Materials and Methods
Women included were enrolled in a multisite, randomized, double-blind, placebo-controlled crossover study of extended release gabapentin in the treatment of PVD. Institutional review board approval was obtained at all 3 study sites: the University of Tennessee Health Science Center, Rutgers Robert Wood Johnson Medical School, and the University of Rochester Medical Center ( clinicaltrial.gov ). Women were enrolled in the study if they were age >18 years; had >3 continuous months of insertional dyspareunia, pain to touch, or pain with tampon insertion (modified Freidrich criteria for vulvodynia); and demonstrated an average score of ≥4 on the 11-point tampon test (0 = no pain at all; 10 = worse pain ever) during the 2-week screening period.
Exclusion criteria included: (1) other vulvar conditions or active infections identified clinically or by a positive Affirm VPIII microbial identification test (BD Molecular Diagnostics, Franklin Lakes, NJ); (2) a prior vestibulectomy; (3) pregnant or at risk for pregnancy and not using a reliable contraceptive for 3 months prior to and during the study; (4) a major medical or psychiatric condition, including substance abuse; (5) a score of ≥12 on the hospital anxiety and depression scale, indicating a major depressive episode ; (6) use of centrally acting medications, excluding selective-serotonin receptor inhibitors; and (7) use of topical lidocaine.
At the screening visit, an interviewer-administered questionnaire collected detailed subject demographic data and a complete medical and gynecological history, including current medications. A visual inspection of the vulva, speculum exam, and bimanual pelvic exam were performed. A cotton swab test was used to clinically confirm PVD, an Affirm test collected, and a Rakoff stain evaluated to determine vaginal estrogen status. If the Affirm test was positive for yeast, Gardnerella , or trichomonas, the patient was treated and rescreened. If the Rakoff stain showed >10% parabasal cells, patients were treated with local estrogen, if appropriate, and rescreened after 6 weeks. Nongenital TPT and intravaginal algometry was performed at a separate visit, only after screening criteria were met.
TPT was performed by using the thumb pad of the dominant hand to apply 4 kg of pressure in a perpendicular direction for 4 seconds to 18 tender points. Vaginal pain sensitivity was measured using a prototype intravaginal pressure algometer, where 0.1, 0.3, and 0.5 kg/cm 2 forces were applied digitally in random assignment by force and location to the right and left iliococcygeus muscle regions and the posterior vaginal wall, for a total of 9 data points. Both TPT and algometer pain intensity were reported on a 0 (no pain) to 10 (worse pain) numeric rating scale (NRS). A diagnosis of FMS was made if pain was present (NRS >1) in at least 11 of the tender point sites.
Correlations were computed between the composite pain intensity of TPT and those of iliococcygeus regions and the posterior vaginal wall. Composite scores were calculated by totaling the NRS at individual nongenital TPT, and for intravaginal algometry by totaling the NRS from the right and left iliococcygeus muscle. Independent t tests were used to determine differences in iliococcygeus regions and the posterior vaginal algometer pain intensity ratings and presence or absence of FMS. The significance level was at P < .05 and the data were expressed as mean ± SD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


