Reduction of Common Joint Dislocations and Subluxations
Frederick C. Johnson
Pamela J. Okada
Introduction
Extremity injuries are a common reason for children to visit the emergency department (ED). When a joint is involved, a range of injuries are possible. The patient may sustain a simple subluxation or dislocation or may have an open fracture through the joint space. The focus of this chapter is the management of subluxations and dislocations. In most cases, these injures can be definitively managed by the emergency physician, while in other cases the emergency physician must perform a limb-saving reduction before transferring the patient to a specialist for further management. The methods of reduction likewise range from the simplest of maneuvers to rather complex techniques requiring multiple operators and muscle relaxants. Before proceeding with a description of the injuries and reduction techniques, two important definitions should be understood. The subluxation of a joint refers to an incomplete disruption where there is partial communication of the articular surfaces. The dislocation of a joint refers to a complete dissociation of its articular surfaces.
Radial Head Subluxation
Radial head subluxation is one of the most common upper extremity injuries in children (1). The classic history involves a child who has traction applied to an arm and then refuses to use that arm. This can occur after a caretaker pulls the arm to prevent a fall, pulls the child up after a fall, pulls the arm of a stubborn toddler, or swings the child by both arms. This has led to the common term “nursemaid’s elbow.” However, it should be noted that the classic history of traction is often not elicited; in many cases, the mechanism of injury appears to be a simple fall. Radial head subluxation is commonly seen in toddlers, although it has been reported in infants younger than 6 months as a result of rolling over in bed (2). An increased incidence in females has also been reported (3,4). The left arm is more commonly injured than the right, perhaps reflecting the fact that a right-handed caretaker is most likely to grasp a child’s left arm. The recurrence rate is up to 33% (3). It most commonly recurs in children 24 months of age or younger. Sex, family history, and the elbow involved in the initial episode are not risk factors for recurrence (5).
Anatomy and Physiology
Radial head subluxation typically occurs in children 1 to 4 years of age as a result of a sudden forceful longitudinal traction on the hand or wrist while the forearm is extended and pronated. The pulling episode is immediately followed by acute onset of pain and resistance to using the arm. The abrupt force affects the humeroradial articulation between the capitellum of the humerus and the head of the radius. Normally, the capitellum fits into the cupped surface of the radial head. A fan-shaped ligament known as the “radial collateral ligament” attaches proximally to the lateral epicondyle of the humerus and distally blends into the annular ligament of the radial head. The abrupt axial tension on the forearm pulls the radial head distally, tearing the distal attachment of the annular ligament and causing the radial head to pull out of the torn annular ligament. The distal aspect of the annular ligament, which slips free from the periosteum of the radial neck, becomes entrapped between the head of the radius and the capitellum. The child holds the forearm in pronation because supination is painful. Forced supination brings the annular ligament into its appropriate position over the radial head by using the radius as a lever (6).
Indications
The physical examination typically reveals a nondistressed child with a flexed elbow and slightly pronated wrist held to the side in the absence of significant point tenderness, ecchymosis, or focal edema. The child will appear content and normal, with the exception of a refusal to use the injured arm. Clinical diagnosis of radial head subluxation can be made when a typical history and physical examination is obtained, and these are usually sufficient grounds to perform the reduction maneuver without first obtaining radiographs. Even in those cases in which a child presents with a nonclassic history, there is little risk of fracture as long as the child has the typical physical examination findings of mild flexion of the elbow and pronated wrist position (7).
Equipment
No equipment is required for reduction of a radial head subluxation.
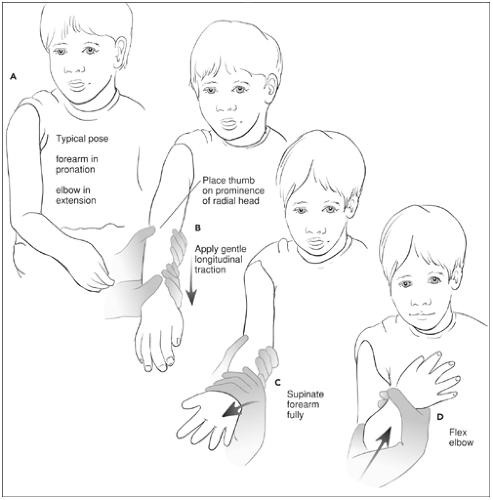
Procedure
Three reduction techniques are commonly employed. Supination at the wrist followed by flexion at the elbow is the classically taught and most commonly used method. The supination technique is performed by first gripping the patient’s elbow using the nondominant hand, with the clinician’s thumb on the patient’s radial head. Using the dominant hand, the clinician grasps the patient’s wrist, applies mild traction, and then in one swift movement supinates the wrist and flexes the forearm up toward the shoulder (Fig. 105.1A–D).
The effectiveness of the second technique, hyperpronation with flexion at the elbow, has been reported in multiple series (3,8,9). This maneuver involves gripping the patient’s elbow using the nondominant hand, forcefully hyperpronating the child’s wrist, and then flexing the forearm toward the shoulder (Fig. 105.2). This technique has shown superior success rates compared with supination-flexion (3,9). Furthermore, when used for the first reduction attempt, the pronation technique appears to be significantly less painful than the supination-flexion method (9). In fact, reduction often occurs with pronation alone.
A third option involves moving the elbow to a 90-degree position, supinating the wrist, and then extending the forearm (10). Regardless of the technique used, an audible or palpable “pop” usually indicates a successful reduction (4). Typically, the child will begin to use the arm within 5 to 10 minutes, although in many cases the child must be enticed to do so with a toy or other desired object (9).
Complications
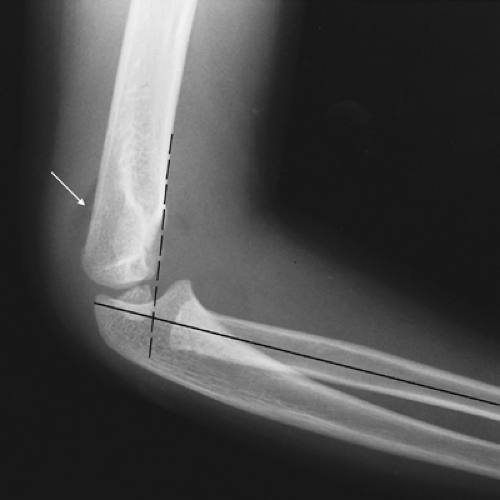
The main pitfall involves overlooking a radial or humeral fracture. The patient must be carefully examined before attempting reduction. Radiographs should be obtained if external signs of trauma, such as swelling, abrasions, or ecchymosis are present. Additionally, failed attempts at reduction warrant radiographs of the elbow to look for signs of a fracture. On radiographs, elevation of the posterior fat pad or misalignment of the intersection of the anterior humeral line and the central radial line away from the middle third of the capitellum should raise suspicion of a fracture (Fig. 105.3) (11). Fractures in children who present with classic history and examination findings are rare; however, if a fracture is present, the reduction techniques will neither return function of the arm nor relieve the pain.
Digit Dislocations
Digit dislocations are common among physically active adolescents and school-age children. The direction of the displacement of the middle or distal phalanx determines the type of dislocation for the proximal interphalangeal (PIP) or distal interphalangeal (DIP) joint, respectively. They are categorized as dorsal, volar, or lateral dislocations.
Dislocation of the DIP joint is less common than dislocation of the PIP joint. This is related to the additional stability provided to the DIP by the insertion of the flexor and extensor tendons to the proximal aspect of the distal phalanx. Closed reduction of the DIP and PIP joints is done in a similar fashion using a combination of traction and either extension or flexion.
Prior to any attempt at reduction of a suspected subluxed or dislocated joint, a thorough joint examination should be performed. Stability of the joint can be determined by testing the range of motion of the interphalangeal and metacarpophalangeal joints of the hand. As with all aspects of the physical examination, range of motion is influenced by pain, so accurate assessment typically requires a digital or wrist block (Chapter 35).
Active range of motion is tested by having the patient move the digit. Completing full range of motion without displacement of the phalanges demonstrates adequate joint stability. Passive joint stability is assessed by applying gentle radial and ulnar stress to each collateral ligament. Passive hyperextension is used to assess volar plate integrity. Stress testing should be done in both extended and moderately flexed positions to eliminate the stabilizing effect of the volar plate. The inability to actively extend the flexed PIP joint against resistance suggests a rupture of the central band of the extensor tendon, which can progress to a boutonniere deformity. Comparison with the same joint of the uninvolved hand may assist in the diagnosis. Thorough examination should occur after any successful joint reduction to ensure stability (12).
Regardless of the type of dislocation, pre- and postreduction radiographs are required to ascertain the presence of a fracture. Radiographic examination should include an anteroposterior (AP) and lateral image. Failure to obtain a true lateral radiograph may result in missing a fracture or a loose body in the joint.
Anatomy and Physiology
The metacarpophalangeal joints are condyloid joints that allow flexion, extension, abduction, adduction, and circumduction. The joints are enclosed by a fibrous capsule. They are strengthened on each side by a triangular collateral ligament that extends from the sides of the head of the proximal bone to the sides of the base of the distal bone. The collateral ligaments are attached to the palmar ligaments, which are strong, thick plates that are firmly attached to the phalanx and loosely attached to the metacarpal. This volar plate is a dense fibrous connective tissue that simultaneously provides support and allows for flexion at the joint (6). The interphalangeal joints are uniaxial hinge joints that only permit flexion and extension. The articulations join the head of one phalanx with the base of the more distal one. Like the metacarpophalangeal joints, they have collateral and palmar ligaments; however, they are reinforced dorsally by the extensor expansions of the digits (Fig. 105.4) (6).
Dorsal dislocations are the most common, resulting from some combination of hyperextension, longitudinal compression, and dorsal translation. Hyperextension of the PIP joint
can cause an avulsion of the volar plate from the middle phalanx (13,14). Volar dislocations of the PIP joint are rare. The most common mechanism is a rotational longitudinal compression force on a semiflexed middle phalanx that results in unilateral disruption of a collateral ligament and partial avulsion of the volar plate (15,16). This force can cause the distal aspect of the proximal phalanx to interpose itself between the central and lateral bands of the extensor tendon. Additionally, it can disrupt the central band as it inserts onto the proximal aspect of the middle phalanx. Because volar dislocations of the PIP joint can be very difficult to reduce, some specialists advocate an orthopaedic consultation for further evaluation and possible open reduction.
can cause an avulsion of the volar plate from the middle phalanx (13,14). Volar dislocations of the PIP joint are rare. The most common mechanism is a rotational longitudinal compression force on a semiflexed middle phalanx that results in unilateral disruption of a collateral ligament and partial avulsion of the volar plate (15,16). This force can cause the distal aspect of the proximal phalanx to interpose itself between the central and lateral bands of the extensor tendon. Additionally, it can disrupt the central band as it inserts onto the proximal aspect of the middle phalanx. Because volar dislocations of the PIP joint can be very difficult to reduce, some specialists advocate an orthopaedic consultation for further evaluation and possible open reduction.
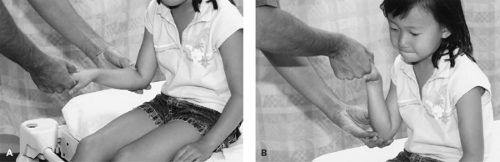 Figure 105.2 Pronation with flexion technique for reduction of radial head subluxation. Reduction of the radial head involves hyperpronation of the forearm (A) followed by flexion of the elbow (B). |
Indications
An interphalangeal joint subluxation is usually associated with forced hyperextension or hyperflexion of the digit during participation in physical activities. The patient presents with acute pain, deformity, and swelling. Radiographs are used to confirm the joint dislocation, identify fractures, and document successful reduction.
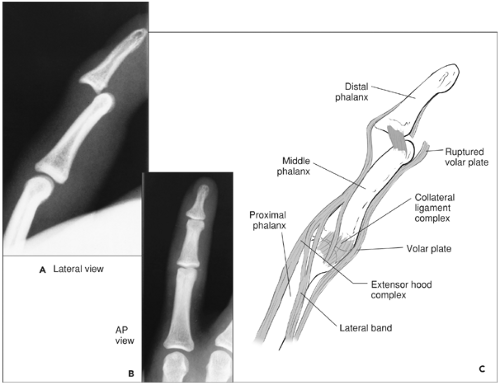 Figure 105.4 Radiographic (A, B) and schematic (C) representation of an interphalangeal joint dislocation. |
Consultation with an orthopaedic surgeon should occur when findings consistent with neurovascular compromise, joint instability, or fracture are present. Additionally, an orthopaedist should be consulted when a lateral or volar PIP joint dislocation occurs. These subluxations may require open reduction and internal fixation (17).
Equipment
For digital block anesthesia:
Antiseptic solution (povidone-iodine or alcohol swabs)
Lidocaine 1% without epinephrine
Sodium bicarbonate 8.4%
27- or 30-gauge, 0.63-inch needle
For reduction:
Gauze pad
For immobilization:
Foam-padded malleable splint, appropriately sized
Tape
Procedure
Prior to reduction, digital block anesthesia should be provided. If rings are present on the affected digit, these should be removed. The reduction technique for a dorsal dislocation consists of three maneuvers. First, the affected joint is hyperextended. Then longitudinal traction is applied to the distal phalanx while hyperextension is maintained. Finally, the dislocated phalanx is gently pushed into its proper position (Fig. 105.5A–D). In some cases, the distal phalanx may be more easily grasped by first wrapping a 4″ × 4″ gauze pad around the finger. Postreduction radiographs are needed to re-evaluate for fracture.
After reduction, stabilization can be accomplished by a variety of means. Many operators choose to apply a splint such as a foam-padded, malleable digit splint. Should this option be chosen, the type of splint applied should be tailored to the injury. Splints for DIP dislocations are applied so that only the DIP is immobile. The DIP is splinted in extension, and the PIP has full range of motion. For dorsal PIP dislocations,
the splint is applied dorsally, with the joint in 20 to 30 degrees of flexion. Splints applied for PIP dislocation should remain in place for 14 to 21 days, whereas those for DIP dislocations should remain in place for 10 to 14 days. Buddy taping to an adjacent finger is an acceptable alternative for younger children (13,14). If the dislocation is irreducible or unstable after reduction, referral to an orthopaedic or hand subspecialist is advised.
the splint is applied dorsally, with the joint in 20 to 30 degrees of flexion. Splints applied for PIP dislocation should remain in place for 14 to 21 days, whereas those for DIP dislocations should remain in place for 10 to 14 days. Buddy taping to an adjacent finger is an acceptable alternative for younger children (13,14). If the dislocation is irreducible or unstable after reduction, referral to an orthopaedic or hand subspecialist is advised.
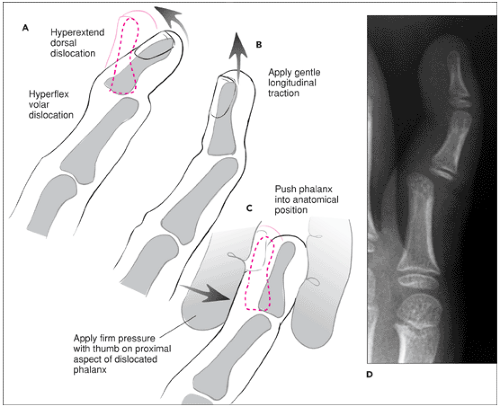 Figure 105.5 Procedure for reduction of dorsal DIP joint dislocation (A–C). Radiograph of PIP joint dislocation (D). |
The reduction of a volar dislocation is more complex than a dorsal reduction. The typical maneuver of longitudinal traction can create a noose around the interposed proximal phalanx and hinder reduction. Some specialists advocate flexing the metacarpophalangeal and PIP joints, followed by gentle traction of the middle phalanx. Because the phalanx can be trapped between the extensor tendons, other specialists view this dislocation as irreducible and requiring open reduction (13,15).
Lateral dislocation of the PIP joint occurs when a radial- or ulnar-directed force leads to disruption of the collateral ligaments and a portion of the volar plate. Reduction is achieved with longitudinal traction and gentle maneuvering of the dislocated segment back into its normal position. The PIP joint is usually stable after reduction and can be treated with buddy taping or splinting. Patients should be referred to a hand specialist for follow-up (13,15).
Dislocation of the interphalangeal (IP) joint of the thumb is similar to dislocation of the DIP joints of the other phalanges. Dorsal dislocation of the thumb is more common than volar dislocation. The mechanism of injury is commonly hyperextension of the joint that results in a rupture of the proximal portion of the volar plate and at least a portion of the collateral ligaments. Reduction involves hyperextension and gentle traction on the distal phalanx (13,15).
Dislocation of the metacarpophalangeal joint of the thumb results from a hyperextension force that ruptures the volar plate, joint capsule, and a portion of the collateral ligament. Reduction is achieved by relaxing the hand with the wrist in flexion, the first metacarpal in flexion and adduction, and the
IP join in flexion. Hyperextension of the joint with continued traction of the proximal phalanx should allow reduction of the joint (13,15).
IP join in flexion. Hyperextension of the joint with continued traction of the proximal phalanx should allow reduction of the joint (13,15).
Complications
Timely reduction of an interphalangeal dislocation rarely results in complications. Complications can be further minimized by obtaining radiographs prior to and after reduction. Radiographs should detect fractures or incompletely reduced joints. Inadequate immobilization can result in redislocation. Delayed reduction can result in joint instability, decreased range of motion of the joint, or decreased function of the joint. Unsuccessful reduction can occur when there is intra-articular entrapment of the volar plate, extensor hood ligaments, or an osteochondral fragment from an associated avulsion fracture.
Shoulder Dislocation
Traumatic dislocation of the glenohumeral joint, or “shoulder dislocation,” is the displacement of the humeral head from its normal articulation in the glenoid fossa. It is an unusual injury in children and occurs most commonly in older adolescents involved in sporting activities. Over 90% of traumatic shoulder dislocations are anterior dislocations and usually result from a force applied to the arm when it is abducted, extended, and externally rotated (18,19,20,21,22). Posterior and inferior dislocations occur rarely. Posterior dislocations may result from direct force to the anterior shoulder or an indirect force when the arm is adducted, flexed and internally rotated (23,24). An inferior glenohumeral dislocation, also known as “luxatio erecta,” is rare, but when it occurs, it is the result of a high-energy hyperabduction force. This injury is so forceful that the humeral head may be driven through the soft tissues of the axilla, producing an open injury (25,26,27,28).
Although many methods have been described for reduction of a shoulder dislocation, few are appropriate for the child or adolescent. Maneuvers using leverage (Kocher) (29,30), overhead traction (Milch, Cooper) (31,32,33,34), external rotation (35,36), or lateral traction (Eskimo) (37,38) are not recommended in children. Reduction by these techniques is associated with complications that include further neuromuscular, vascular, and soft-tissue injury; fractures of the humeral neck and glenoid rim; and spiral fractures of the humeral shaft.
For the pediatric patient, reduction by forward flexion with gravity (Stimson) (39,40), scapular manipulation (Anderson) (41,42,43), or traction-countertraction (modified Hippocrates) are recommended. These reduction techniques are 70% to 90% effective on the first attempt and are commonly performed by emergency physicians in the ED (38).
In general, immediate orthopaedic consultation is required for posterior and inferior dislocations and for dislocations involving neurovascular compromise, humeral neck fractures, or intra-articular bony fragments. Intra-articular fractures often require open reduction and internal fixation. Because posterior and inferior dislocations are rare in children, this discussion will focus on the management of anterior dislocations.
Anatomy and Physiology
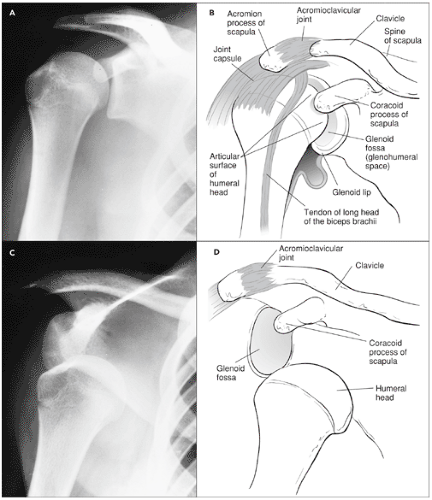
The glenohumeral joint is one of the most mobile joints in the body, owing to the roughly hemispherical humeral head and shallow scapular glenoid fossa. Support of this joint comes mostly from the surrounding muscles and ligaments. The fibrous joint capsule, glenohumeral ligament, coracohumeral ligament, transverse humeral ligament, glenoid labrum, and muscles of the rotator cuff (supraspinatus, infraspinatus, teres minor, and subscapularis) all provide stability to the shoulder. The anteroinferior glenohumeral ligament is the most common site of injury in anterior shoulder instability (Fig. 105.6A,B) (44). With an anterior dislocation, the inferior glenohumeral ligament and anterior labrum are usually disrupted, and this can result in a fracture of the glenoid rim (Bankart lesion) (45,46). Additionally, as the anterior aspect of the glenoid rim impacts against the posteromedial aspect of the humeral head, an indentation fracture of the humeral head (Hill-Sachs lesion) can occur. A Hill-Sachs lesion further destabilizes the shoulder joint, predisposing it to recurrent dislocations (47).
In the child, vascular and nerve injuries are rare after an uncomplicated shoulder dislocation. In the adolescent, the rotator cuff muscles may tear; a young child may sustain a fracture of the proximal humerus. Axillary nerve dysfunction may occur and results in decreased deltoid muscle contraction and decreased light touch sensation over the area of the deltoid muscle. The brachial plexus and circumflex nerves are infrequently injured. The axillary artery may sustain traction or compression injury during dislocation or secondary to forceful reduction (22,38,44,48).
The forward flexion and abduction maneuvers for reducing an anterior shoulder dislocation use the traction-countertraction principle to lever the humeral head into the glenoid fossa. Both maneuvers fatigue the shoulder girdle muscles, relax the biceps muscle, protect neurovascular structures, and help prevent humeral head impaction on the glenoid. The forward flexion technique allows spontaneous reduction using gravity, time, and muscle relaxation. The abduction technique applies active opposing forces.
Scapular manipulation causes the glenoid to release the humeral head impaction and allow reduction. When the humeral head dislocates from forced abduction and external rotation, the glenoid fossa is forced medially, and the inferior tip of the scapula is abducted. Although scapular manipulation has not been studied in patients younger than 17 years, this technique is atraumatic, uses minimal force, and has no reported complications in adults (41,42,43).
Traumatic shoulder dislocations are acutely painful. With anterior dislocations, the arm is held in slight abduction and external rotation. Movement of the arm is extremely painful
secondary to muscle spasms. The humeral head is palpable anteriorly, and there is a “sunken” space inferior to the acromion. With posterior dislocations, the arm is usually held in adduction and internal rotation. External rotation and abduction are extremely painful. The shoulder will appear “flat” anteriorly and have a prominent coracoid process.
secondary to muscle spasms. The humeral head is palpable anteriorly, and there is a “sunken” space inferior to the acromion. With posterior dislocations, the arm is usually held in adduction and internal rotation. External rotation and abduction are extremely painful. The shoulder will appear “flat” anteriorly and have a prominent coracoid process.
Patients undergoing shoulder reduction should first receive adequate analgesia and then should undergo a complete neurovascular examination. The physician should assess radial, median, ulnar, and axillary nerve function and should remember that the axillary nerve is the most commonly injured nerve with an anterior dislocation. Axillary nerve function can be assessed by testing pinprick and light touch over the deltoid muscle.
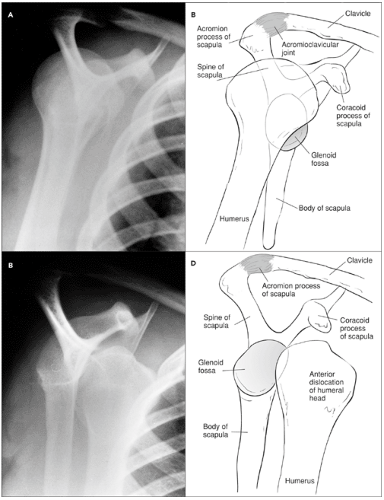
After the initial examination, the care provider should obtain radiographs of the shoulder. AP, axillary, and scapular Y views will accurately delineate the dislocation, the position of the humeral head, and any associated fractures. The AP projection provides information about the glenohumeral space (Fig. 105.6C,D). The axillary projection delineates the coracoid, acromion process, and humeral head and identifies an impaction fracture. The scapular Y view best demonstrates the position of the humeral head in relation to the Y-shaped projection of the scapula. The humeral head normally lies centrally within the glenoid between the coracoid process and the acromion process (Fig. 105.7A–D). Even in cases of apparently uncomplicated dislocations, both pre- and postreduction radiographs should be obtained. Such films can provide medicolegal protection by demonstrating that injuries were present prior to the reduction attempt and were not caused by it (49,50,51,52,53). When dislocated, the humeral head is shifted to an abnormal anterior, posterior, inferior or, rarely, superior position. To better identify a fracture of the humeral head or glenoid rim, an apical oblique view, a computed tomography (CT) scan, or even a magnetic resonance imaging (MRI) scan of the shoulder can be obtained. However, such images are rarely required in the emergent management of shoulder dislocations.
Indications
The presence of a radiographically confirmed shoulder dislocation is an indication for a reduction procedure. For posterior or inferior (luxatio erecta) dislocations or when a dislocation is complicated by neurovascular compromise, humeral neck fracture, or intra-articular bony fragments, an orthopaedic consultation should be obtained.
Equipment
Medications for procedural sedation
Monitoring equipment
Weights, 2 to 5 kg
Two sheets
Sling and swathe
Shoulder immobilizer
Procedure
After interposed intra-articular fragments are excluded, the following reduction maneuvers are appropriate for a child or adolescent.
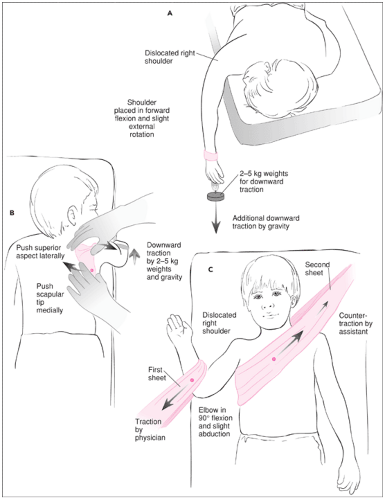
Stimson Technique
The patient is placed in the prone position with the affected arm hanging vertically over the edge of the examination table (Fig. 105.8A). The shoulder is in forward flexion and slight external rotation. With adequate sedation and analgesia, the shoulder will sometimes reduce spontaneously due only to the effect of gravity. However, in most cases additional weight is required. Weights from 2 to 5 kg can be strapped onto the wrist of the affected arm to provide additional downward traction. As the shoulder muscles fatigue, the humeral head will gradually relocate into the glenoid fossa. This gentle procedure is simple and safe but may take up to 20 to 25 minutes, and analgesics and sedatives are often required.
Scapular Manipulation
As with reduction by gravity, the patient is placed in the prone position with the affected arm hanging vertically over the edge of the examination table (Fig. 105.8B). The operator can place 2- to 5-kg weights hanging from the wrist of the affected arm or have an assistant provide gentle downward traction. In either case, traction should be applied for approximately 5 minutes. When the patient’s muscles relax, the scapula will usually become readily visible beneath the skin. It can be gently rotated by pushing its tip medially and its superior aspect laterally. A palpable or audible “clunk” may accompany successful reduction.
This procedure may also be performed with the patient seated. The patient is positioned facing the back of a stable chair and with the chest supported against the back of the chair. Then with the affected arm held parallel to the floor anteriorly, an assistant applies gentle longitudinal traction to the arm. After approximately 5 minutes of traction, the operator manipulates the scapula as previously described. It may be necessary to have a second assistant stabilize the chair so that it does not slide forward or to the side.
Traction-Countertraction
With the patient in a supine position, a sheet is placed around the patient’s chest under the affected axilla and then around an assistant (Fig. 105.8C). Using this sheet and standing on the patient’s unaffected side, the assistant provides countertraction. The affected arm is placed in slight abduction, with the elbow in 90 degrees of flexion. A second sheet is wrapped around the patient’s flexed forearm just distal to the elbow and then is wrapped around the operator’s body. The operator is positioned on the affected side approximately even with the patient’s waist. Once adequate sedation is achieved, longitudinal traction is applied by pulling the sheet attached to the affected arm laterally and caudally while keeping the patient’s arm abducted and elbow flexed. Both the operator
and the assistant can gain mechanical advantage by leaning back against the sheet. As traction causes the muscles to fatigue, gentle internal and external rotation will often help to disengage the humeral head. Reduction of the humeral head into the glenoid fossa is usually obvious and may be associated with an audible “clunk.” This procedure is effective for both anterior and posterior dislocations.
and the assistant can gain mechanical advantage by leaning back against the sheet. As traction causes the muscles to fatigue, gentle internal and external rotation will often help to disengage the humeral head. Reduction of the humeral head into the glenoid fossa is usually obvious and may be associated with an audible “clunk.” This procedure is effective for both anterior and posterior dislocations.
Internal Rotation Technique
The patient is placed in a reclined or seated position. This procedure may require an assistant to aid in the reduction. The operator faces the patient and applies constant anteroposterior pressure using one hand placed over the patient’s distal clavicle at the level of the humeral head. The affected arm is held flexed at the elbow and in slight abduction and internal rotation at the shoulder and is supported in this position by the operator or an assistant. After adequate sedation and analgesia, continuous longitudinal traction is applied to the affected arm, and it is gradually abducted to 90 degrees. The affected arm is brought toward the midline and then to the opposite side so that the hand is gently forced to touch the opposite shoulder. This maneuver is performed with a smooth arclike motion of the arm, and reduction usually occurs as the hand nears the opposite shoulder. This approach is useful in anterior dislocations.
Following any successful reduction, active motion and a normal contour of the shoulder are usually evident immediately. Distal neuromuscular status should be assessed after reduction to identify brachial plexus or vascular injury. AP and scapular Y radiographs should also be obtained to confirm successful reduction and evaluate for subtle fractures of the humeral head, glenoid tip, or humeral tip. A sling and swathe or shoulder immobilizer should be applied for 1 to 3 weeks (it can be removed for bathing). Immobilization allows healing of the anterior capsule and glenoid ligaments. The patient should be referred for orthopaedic evaluation and physical rehabilitation within 1 to 2 weeks of the reduction and should not participate in sports or other vigorous activities for 3 to 6 weeks.
Complications
The most common complication of traumatic shoulder dislocation is recurrent shoulder instability. This is due to a stretched subscapular tendon and to capsular laxity. Young age appears to be the highest predictor of recurrence. If a child has a shoulder dislocation before 10 years of age, the recurrence rate is 100%; if the first dislocation occurs between the ages of 10 and 20 years, the recurrence rate is 80% to 90%; and if the first dislocation occurs after age 20 but before age 30, the recurrence rate is 64% to 70% (18). Glenoid rim fractures and humeral head impaction fractures (Hill-Sachs) also increase the rate of recurrence (18,39,54,55,56,57,58,59,60). In some cases, soft tissues (e.g., the long head of the biceps tendon) or boney fragments within the joint prevent closed reduction. These patients usually require operative intervention.
Other rare but reported complications include fractures, neuromuscular injuries, and, rarely, osteonecrosis of the humeral head. Nerve injury involving the brachial plexus occurs in 10% to 25% of cases, most commonly involving the axillary nerve. In younger children, avascular necrosis of the humeral head, axillary artery injury, or degenerative arthritis can occur. Complications of the reduction technique, although infrequent, result from excessively forceful traction and compression on neurovascular structures in the axilla. Humeral neck and spiral humeral shaft fractures occur rarely from an overly forceful reduction and can be avoided with adequate sedation, analgesia, and muscle relaxation (36,38,46,48,54,61).
Patella Dislocation
Patellofemoral instability is a common cause of ED visits in the adolescent population. Contrary to the stereotype of an overweight, sedentary child with patellar dislocation after little or no trauma, most patellar dislocations occur in athletically active children. Injuries can occur from either indirect or direct trauma to the knee, although a noncontact mechanism is more common (62,63,64). The average annual incidence of first-time patellar dislocation is 5.8 per 100,000. Females aged 10 to 17 years are at the greatest risk for first-time dislocation, with an annual incidence of 33 per 100,000 (62). Patients with a first-time dislocation were found to have a recurrence rate of 17%, whereas patients with a history of multiple dislocations had a recurrence rate of 49% (62).
Anatomy and Physiology
The patellofemoral articulation is a complex joint that relies on both bones and soft tissues for stability. The medial patellofemoral ligament (MPFL) and the vastus medialis muscle provide the greatest amount of resistance to lateral patellar movement. The MPFL runs from the medial femoral epicondyle to the superomedial aspect of the patella. This is the structure that is almost universally injured in lateral patellar dislocations. The patella commonly dislocates in a lateral direction and is frequently associated with injury to the MPFL and the cartilaginous surfaces of both the patella and femur (Fig 105.9A–D) (65).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree