Principles of Orthopedics
Paul D. Sponseller
Orthopaedic Surgery, Johns Hopkins University, Johns Hopkins Hospital, Baltimore, Maryland 21287.
Pediatric surgeons should be familiar with the principles of pediatric orthopedics in order to deal with trauma, recognize skeletal manifestations of systemic diseases, and evaluate congenital or developmental abnormalities. This chapter is intended to help in the initial understanding of the broad range of orthopedic conditions encountered in children and is therefore intended for breadth of coverage. Conditions isolated to one anatomic region are presented first, followed by generalized musculoskeletal conditions. The references provided at the end of this chapter can serve as a guide for further study of any particular condition (1,2,3,4). For more information on orthopedic principles of trauma, refer to Chapter 27.
Because orthopedic terminology is not always straightforward, the following definitions are provided to assist the reader. The term physis refers to the growth plate (Fig. 105-1); therefore, the epiphysis is the portion of a bone “on top of” the physis (i.e., nearer the joint), the metaphysis is the widened portion of the shaft adjacent to and arising from the growth plate, and the diaphysis is the narrow portion of a tubular bone midway between two physes. The skeleton is largely formed from a cartilaginous precursor, with ossification of the cartilage beginning in the diaphysis. Secondary ossification centers at the ends of each long bone. The small bones of the wrist and foot begin from a single ossification center.
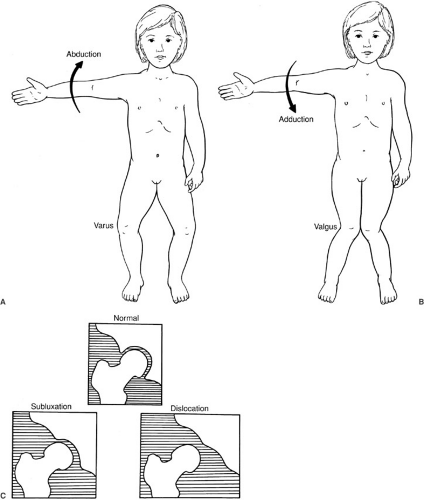
The Greek root genu refers to knee, coxa to hip, and pes to foot. When two bones or two fracture fragments form an angle, they are in varus when the apex of the angle points away from the midline (Fig. 105-2) and valgus when it points toward the midline. Alternatively, angulation may be stated in any of the three standard anatomic planes by the direction of the apex—that is, genu valgus is medial angulation of the lower extremity at the knee. Dislocation refers to complete loss of contact of two joint surfaces, and it is specified by the direction of displacement of the most distal part. Subluxation is a partial or incomplete dislocation. For example, in a dislocated hip, the femoral head is completely out of the acetabulum; a subluxated hip has been only partially offset. Abduction refers to movement away from the midline, whereas; adduction refers to movement toward the midline.
ABNORMALITIES BY REGION
Foot
Isolated idiopathic adduction of the forefoot or metatarsals is designated by the terms metatarsus adductus, metatarsus varus, or C-foot. In contrast to clubfoot, the hindfoot and ankle are normal. The ankle joint itself has normal dorsiflexion and plantar flexion. The etiology may be increased medially directed pressure in the uterus. Children with metatarsus adductus also may have an increased incidence of other molding deformities, such as developmental dislocation of the hip or torticollis (5).
The natural history of untreated metatarsus adductus is spontaneous correction in 85% of children. In 10% of children, mild adduction persists, and in only 5% is it severe (6). Therefore, the preferred treatment is observation and stretching for the first 4 to 6 months, with corrective casts or splints if severe metatarsus adductus persists beyond this time. The casts are changed every 1 to 2 weeks until the adduction is clinically corrected, then followed by holding casts or shoes. Surgery (osteotomy) for very late deformities, in children older than 3 years, is only rarely necessary.
Clubfoot, or equinovarus congenita, is a more complex disorder that includes not only metatarsal adduction, but also abnormalities of the hind part of the foot—that is, malrotation of the calcaneus under the talus and equinus (plantar flexion) of the ankle. The incidence of clubfoot is 1 per 1,000 births, and it is more common in males than in
females. Clubfoot may be unilateral or bilateral. Etiology is unknown. Abnormalities have been found in the leg muscles or tarsal bones.
females. Clubfoot may be unilateral or bilateral. Etiology is unknown. Abnormalities have been found in the leg muscles or tarsal bones.
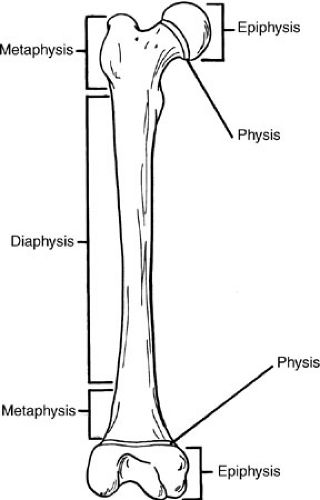 FIGURE 105-1. Regions of a long bone. The physis or growth plate is the main reference point. The epiphysis refers to the segment on top of the physis, and so forth. |
The clubfoot appears smaller than normal for age, and the combination of deformities results in a 90-degree rotation of the forefoot in all planes so the leg and foot truly resemble a club (Fig. 105-3). There is a deep crease on the medial border of the foot. The deformity may be correctable to neutral only in the neonatal period, and the range of motion is limited in all directions. Radiographs show an abnormal parallelism of the talus and calcaneus. Neuromuscular disorders (especially lipomeningocele, myelomeningocele, spasticity, or arthrogryposis) may produce similar deformities.
Clubfoot ranges from a mild, postural, and easily correctable form to a severe and resistant form. However, cast correction is indicated in all. This is most successful in the perinatal period when ligamentous laxity is greatest. The casts are changed every week. A percutaneous tenotomy of the Achilles tendon is performed after the rotation of the foot is corrected. The correction of the foot is maintained by the use of night splints or braces. Overall, cast treatment is effective in about three-fourths of patients. Surgery is indicated in the others and involves complete correction of all bony malalignments and tendon contractures; it is performed most commonly at ages 6 to 12 months (7). In older patients or in those with recurrent deformity, osteotomy or fusion may be indicated.
A calcaneovalgus foot is common in newborns. The foot is dorsiflexed and in valgus so the dorsum of the foot may almost be touching the tibia (Fig. 105-4). The bones and joints themselves are normal. The condition spontaneously improves within the first few months.
Flatfoot (planovalgus) should be divided into flexible and rigid types. The flexible type is a normal variant in children and is usually asymptomatic. Development of an arch occurs spontaneously in the first 8 years of life in most children. The arch of the foot is restored. When the child is on tiptoes or when weight bearing is relieved, varus-valgus motion is normal. As a herald to a more serious condition, rigid flatfoot may be due to tarsal coalition, vertical talus, neuromuscular imbalance, or arthritis of the foot. These should be considered in the differential diagnosis.
The cause of the usual type of flexible flatfoot is ligamentous laxity. There is no primary muscle abnormality. Occasionally, a tight heel cord may contribute to producing flatfoot by pulling the foot into greater valgus. Treatment is not indicated in cases of flexible flatfoot; prospective studies (8) have shown that no orthotic or special shoe can produce a lasting change in pediatric flatfoot. Such devices may be indicated for neuromuscular flatfeet, but not in asymptomatic children with flexible flatfeet. The heel cord should be stretched if it is tight. Rarely is soft-tissue reconstruction or osteotomy indicated.
General principles to stress to parents when they ask about shoes are summarized in an article by Staheli (9):
Shoes are primarily for protection.
Corrective shoes have no effect on flat feet.
Shoes should be flat, flexible, well aerated, and high topped if needed to keep them from slipping off.
These characteristics should be found in most reasonably priced footwear available in regular shoe stores.
Tarsal coalition involves the bones of the hindfoot, with persistence of a bridge or coalition between two of them. This bridge may be fibrous, cartilaginous, or bony. Tarsal coalition is transmitted as autosomal dominant and is present in approximately 5% of the population (10). Many persons with tarsal coalition are asymptomatic. The presence of symptoms seems to be related to the degree of valgus, which places more strain on the abnormal coalition. Tarsal coalition usually presents during the second decade as an ankle sprain with persistence of pain longer than expected or as spontaneous onset of pain in the ankle. The reason for this presentation is probably that the ossification that occurs at this time, near skeletal maturity, makes the coalition stiffer and therefore symptomatic. The hindfoot shows limitation of varus-valgus motion, but it is usually tender to palpation. The foot appears to be in valgus
more often than not. Sometimes pain manifests over the peroneal muscles, which overcontract to stabilize the foot.
more often than not. Sometimes pain manifests over the peroneal muscles, which overcontract to stabilize the foot.
A plain oblique radiograph of the foot can reliably show the most common type of coalition, the calcaneonavicular bar, if it has ossified (10). However, it is not evident on the anteroposterior (AP) or lateral view. If it is fibrous or cartilaginous, there may not be a bony connection, but an irregularity of the adjacent cortices may be seen. Normal films in the presence of physeal findings of a coalition indicate the need for a coronal computed tomography (CT) scan of the foot to search for a talocalcaneal coalition, the other common type of coalition.
With rest or casting, many coalitions develop enough stability to ossify and become painless. If pain persists, however, the coalition can be excised if it is not large and if no arthritic change has occurred (11). If these conditions
are not met, fusion of the hindfoot is the best treatment for the symptomatic foot.
are not met, fusion of the hindfoot is the best treatment for the symptomatic foot.
Tibia
Internal tibial torsion is the most common cause of in-toeing between 1 and 3 years of age (12,13,14). Tibial torsion is measured by the angle between the foot and thigh, with the ankle and knee bent at 90 degrees. Normally, the foot turns out more with increasing age. Differential diagnosis includes metatarsus adductus, femoral anteversion, or neuromuscular disorders. Tibial torsion naturally improves with growth, but this often takes years. Because the benign natural history of this condition is now known, braces, such as the Denis-Browne bar, are rarely used (13). Studies have shown that braces cannot apply significant rotational force to the tibia because the force is dissipated through the foot, knee, and hip joints. The improvement attributed to the brace in years past is now believed to be due to normal growth patterns. Correction through growth is a gradual process and often frustrates parents. Prior traditional use of braces, reinforced by comments from grandparents and friends, often drive anxious parents to visit the doctor to ensure they are not missing a golden opportunity to prevent deformity. The physician should be confident in allaying the anxiety. The use of a graph may prove convincing. Minor persistent internal torsion has not been shown to be detrimental.
External tibial torsion is less common. These children often appear clumsy for their age. There is little data on the course of this condition; however, treatment is not indicated, and some spontaneous improvement can be expected.
Mild anterior and lateral bowing of the tibia are common in infancy and should be observed to ensure they correct spontaneously. Focal, sclerotic defects in the tibia may be seen with marked anterolateral bowing. Such patients may present with or develop a fracture (congenital pseudoarthrosis), and patients may be found to have neurofibromatosis. If the severe anterolateral bow is present, but the tibia is not fractured, it should be braced for protection. If it is fractured, attempts to gain union by electrical stimulation, rod insertion, vascularized fibula grafting, or bone grafting have similar success rates of 50% to 75% (15). An anterolateral bow may also be seen with congenital absence of the fibula, but this does not progress to fracture.
Posterior/medial bowing of the tibia is also benign; this usually straightens by age 4 and is not associated with fracture. However, there may be 2 to 6 cm of shortening by maturity. Treatment is stretching of the tight dorsiflexor muscles and length equalization as indicated later in childhood (16).
Knee
Extensor Mechanism Disorders (Patellofemoral Problems)
In children and adolescents, a number of conditions involving this region have been described. They are treated by attempting to improve the basic biomechanical forces.
Chondromalacia is a nonspecific term that refers to the appearance of softening and degeneration of the patellar cartilage. Patellar subluxation refers to partial lateral displacement of the patella. The terms patellofemoral stress syndrome, patellar malalignment, and excessive lateral pressure syndrome refer to the abnormal mechanics causing stress concentration and pain.
The quadriceps-patella mechanism is in valgus, as measured by the Q (quadriceps) angle from anterior superior spine to patella to tibial tubercle. Possible factors contributing to patellar pathology include increased valgus of the knee, increased anteversion of the femur or external torsion of the tibia, a high patella (patella alta), abnormal shape or development of the quadriceps, or flattening of the femoral groove. Underdevelopment of the medial side of the quadriceps restraints contributes to subluxation or dislocation. Females normally have slightly greater valgus of the knee than males. Cartilage degeneration occurs beginning in the deep layers and becoming visible later.
Clinically, patellar problems cause symptoms of aching in the anteromedial region of the knee. This is usually worse with stair-climbing or prolonged sitting because flexion increases patellofemoral force. Crepitus may be felt, but this may be painless in some patients and is not in itself pathologic. “Catching” or “locking” may be noted. A feeling of “giving way” may be related, especially with subluxation of the patella. On physical examination, the most reliable way to test patellar tenderness is by direct compression of the patella against the femur. Palpation under the patella is not diagnostic. Effusion is present only if patellar degenerative changes or extreme overuse have occurred. In most cases, there is no effusion. Reproducing patellar subluxation by laterally directed pressure may produce apprehension (the apprehension test). Radiographs are usually nonspecific, but occasionally lateral displacement or tilt of the patella may be seen on the sunrise view.
Patellofemoral stress disorders are common between the ages of 10 and 20 years, but often become less bothersome after these years and do not usually progress to arthritis.
Differential diagnosis includes a synovial fold or plica, a medial meniscus tear, tendinitis of the quadriceps or patellar tendon, and osteochondritis dissecans of the patella or distal femur.
Treatment consists of decreasing activities performed with knees flexed, such as stair-climbing and prolonged sitting. Temporary rest from sports and use of nonsteroidal antiinflammatory agents may be necessary. Exercises to strengthen the medial (stabilizing) part of the quadriceps include extension from 0 to 30 degrees, by lifting weights within this range or extending the knee on a pillow to compress it. Muscles should be stretched if they are tight. Arch supports may help if flexible flat feet are contributing to tibial torsion. Surgical measures are rarely needed, but they include release of a tight lateral patellar retinaculum, medial soft-tissue tightening, tibial tubercle transfer, or correction of valgus, anteversion, or patella alta. These all produce satisfactory pain relief in 75% to 90% of cases.
Patellar dislocations may be acute or recurrent. The patella usually dislocates laterally. An acute dislocation is associated with significant swelling and medial knee pain, and follows valgus or rotating force. This should be treated for 4 to 6 weeks with the knee extended, using a knee immobilizer, except in cases with bony avulsion. Recurrent subluxation is common; the patient has less pain and swelling, and subluxation often occurs during everyday activities. A realignment operation as described earlier is the only effective way to stop frequent and bothersome episodes.
Osgood-Schlatter disease, patellar tendinitis (jumper’s knee), and quadriceps tendinitis are all manifestations of excessive, repetitive stresses on the extensor mechanism. They are listed in order of decreasing frequency in children.
Osgood-Schlatter “disease” is a traction-induced inflammation of the tibial tubercle, not really a disease. Rather, it is a reaction of the bone and growth cartilage of this region to repetitive stress. The tibial tubercle is a distal extension of the proximal tibial epiphysis. It develops an ossification center between ages 9 and 12, but does not completely ossify until ages 15 to 17 years. It is within this age range that repetitive stresses can gradually deform the tubercle, causing enlargement of the tubercle and local inflammation. Tenderness and swelling are localized to the tubercle only and do not extend to the joint. Running, jumping, or kneeling exacerbates symptoms. Treatment involves decreasing activity to a level at which symptoms are minimal, occasionally using a knee immobilizer, crutches, and ice after activity in severe cases. The patient may be vulnerable to recurrence for up to 2 years until the tubercle matures. If he or she is educated about this likelihood, individual regulation of activities can be effective. Complete avulsion of the tubercle is extremely rare and seems more related to sudden stress than to apophysitis.
Patellar tendonitis, inflammation at the origin of the patellar tendon (at the inferior pole of the patella), is related to the same type of overuse as Osgood-Schlatter apophysitis. It is most often seen in basketball players, and is therefore known as jumper’s knee. Pain present during both rest and activity is more worrisome than pain occurring just after activity. Treatment is the same as for Osgood-Schlatter disease. Warm packs before and cold packs after activity may also be of help. Rarely, pain may occur at the proximal pole of the patella and is termed quadriceps tendinitis.
Popliteal cysts in children are localized on the medial side of the popliteal region (Fig. 105-5). They occur most commonly in boys younger than age 9 years. Unlike popliteal cysts in adults, these cysts in children are usually not associated with any intraarticular pathology (17), and they usually regress spontaneously with time. The recurrence rate is higher after surgical excision than after observation. The origin of these cysts is a slitlike communication through the joint capsules between the knee joint and the gastrocnemius-semimembranous bursa on the medial side of the popliteal region.
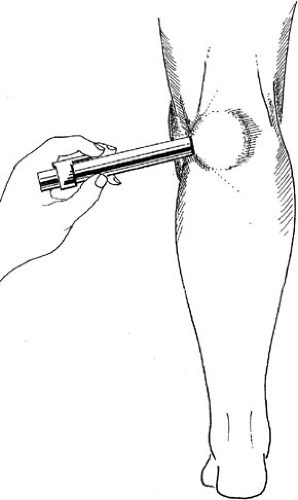 FIGURE 105-5. Popliteal cyst is characterized by a swelling in a characteristic location—the posteromedial aspect of the knee. Transillumination is confirmation of the cystic nature. |
These cysts often present as tumors but can usually be differentiated clinically by their characteristic location, firm consistency, discrete encapsulation, and slight mobility. Transillumination is helpful because the whole contents of the mass lights up when the room is darkened, distinguishing it from a blood-filled or a solid tumor. Biopsy should rarely be necessary.
A discoid meniscus is an acquired flattening and deformation of the normally semilunar lateral meniscus. In some cases, this flattening occurs because of the absence of normal peripheral attachments. Symptoms such as pain, clicking, and locking often develop in the absence of trauma in children from age 2 to adulthood (18). The meniscus should be trimmed or excised if symptoms become severe.
Bowed leg or genu varum of up to 20 degrees is normal in children until the age of 18 months. Bowing normally does not increase significantly after walking begins (12). After the age of 24 months, valgus of the knee begins to develop instead (19). Radiographs are indicated if varus is present after this age or is progressive after 1 year, if it is unilateral, if it appears to be severe, or if it occurs in a high-risk group such as heavy black children who walk early (12). Radiographic findings of benign genu varum include bowing of the tibia and femur; a normal-appearing growth plate physis, without narrowing or step-off; and a generalized, rather than focal, varus angle.
Treatment of physiologic genu varum is observation until resolution. On physical examination, the measurement should be performed with the child standing and may also be confirmed by measurement of the distance between the femoral condyles. These methods are not as accurate as radiographs, but they are a practical way of following change in patients when the presumptive diagnosis is physiologic genu varum.
Differential diagnosis of physiologic genu varum includes Blount disease, rickets, posttraumatic growth plate disturbance, enchondromatosis, achondroplasia, or other skeletal dysplasias.
Blount disease (tibia vara) is an idiopathic, mechanical overload of the medial tibial growth plate that may be unilateral or bilateral. It presents initially in two different age groups, childhood and adolescence.
If untreated, infantile tibia vara is almost always progressive; along with the varus, it includes flexion and internal rotation and often increased lateral knee laxity. Radiographs demonstrate progressive depression of the medial metaphysis, growth plate, and epiphysis. Eventually, the medial metaphysis fuses to the epiphysis in severe cases. A helpful early distinction unique to tibia vara is the focal nature of the change (Fig. 105-6), with sharp angulation of the proximal tibial metaphysis, resulting in a metaphyseal-diaphyseal angle of 11 to 16 degrees or more. This is a specific sign because such localized angulation occurs in fewer than 5% of children with physiologic varus, but in essentially all cases of Blount disease (20).
Treatment with a night brace, although not scientifically proven to be effective, is usually used for the mild but definite cases of Blount disease up until about age 3 years. Valgus-rotational osteotomy of the tibia is indicated if the angulation progresses, if growth plate depression occurs, and if the patient is older than 3 years. Recurrence is a risk if treatment begins after 4 years of age, if the epiphysis is fragmented, or if the child is obese. Persistent varus leads to early knee arthritis.
Adolescent tibia vara has onset after 9 years of age. It is to be distinguished from persistent cases of infantile tibia vara. It is most common in obese males. It is believed to be due to decreased growth of the medial tibial physis from excessive medial stresses. Radiographs show medial femoral and tibial bowing. Treatment is osteotomy to realign the limb, or closure of the lateral growth plate to allow catch-up growth medially.
The knee goes through a series of phases of normal alignment. Varus is common before age 2. Valgus of the knee is normal after age 2, reaches a mean of 12 degrees at 3 years, and remains at a mean of approximately 7 degrees in boys and 9 degrees in girls after 8 years of age. If valgus remains over 15 degrees at 10 years, early growth plate stapling or later osteotomy of the affected region may be
indicated to prevent patellofemoral problems and degenerative changes. Valgus of the proximal tibia often develops after medial tibial metaphyseal fractures, but it usually spontaneously corrects at least partially.
indicated to prevent patellofemoral problems and degenerative changes. Valgus of the proximal tibia often develops after medial tibial metaphyseal fractures, but it usually spontaneously corrects at least partially.
Hip
Developmental Dysplasia of the Hip
The hip develops from a common cartilage anlage resulting from reciprocal contact between the femur and acetabulum during growth. Loss of this contact may occur at any point in development as a result of abnormal in utero positioning; neuromuscular abnormalities such as myelodysplasia, arthrogryposis, and Larsen syndrome; or intrinsic abnormalities in the connective tissue. The earlier this loss of relationship occurs, the more severe are the femoral and acetabular abnormalities; the earlier it is corrected, the more the remodeling potential and the better the potential outcome.
The etiology of dislocation of the hip in an otherwise normal child is multifactorial. Mechanical factors play a role, and the frequency is greatly increased in breech presentation [a factor in 30% of all developmental dysplasia of the hip (DDH)], in firstborn children, and in oligohydramnios. Breech position causes the hip to be hyperflexed and the muscle forces to be increased, causing the femur to be directed out over the edge of the acetabulum. The left hip is slightly more commonly involved than the right. These factors are associated with increased force across the hip, positioning, or both. Hormonal factors may play a role because there is generalized ligamentous laxity around the time of birth due to increased circulating estrogens and relaxin. The incidence of DDH is sixfold greater in girls than in boys. Evidence for hereditary control of these and other factors is that more than 20% of patients have a positive family history.
There are three degrees of hip dysplasia—subluxable, dislocatable, and dislocated hips—in order of increasing severity. In the first type (subluxable), the femoral head rests in the acetabulum and can be partially dislocated by examination. A dislocatable hip is also located normally when at rest, but it can be fully dislocated. A dislocated hip rests in the dislocated position. The combined incidence of these three types is about 1 in 60 births; incidence of a true dislocation is only 1.5 in 1,000. Because of this variability, a change in terminology from congenital dislocation to developmental dysplasia of the hip has become widely accepted. Dysplasia better describes the spectrum of severity, from malformation to dislocation of the hip. Developmental is meant to acknowledge that some cases are not detectable at birth and may occur later; the anatomic findings are continually evolving. The pathologic anatomy includes laxity of the capsulae, which progresses to capsular contraction with time if the hip remains out. The acetabulum becomes shallow because of lack of concentric contact with the femoral head. A false acetabulum may form where the femoral head contacts the lateral wall of the ilium above the normal location. The outer rim of the acetabulum becomes rounded during the period when the femoral head is able to slide in and out of the acetabulum. The movement over this ridge is felt as the “clunk” of the Ortolani and Barlow tests. The proximal femur remains anteriorly rotated (anteverted) as the head rests against the lateral iliac wall.
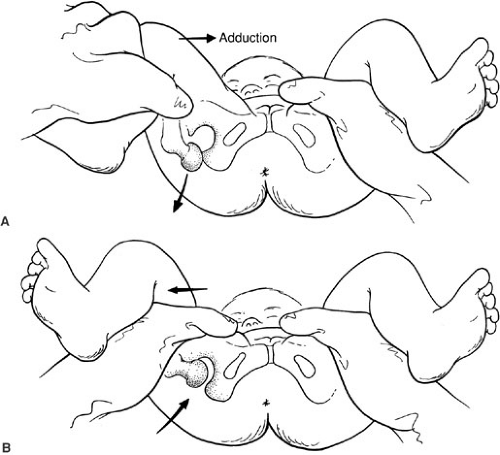
Physical examination remains the most important means of diagnosis. A general rule is that the signs in the newborn period usually consist of instability without significant fixed deformity, whereas in the later months an untreated dislocation becomes more fixed, and there is less instability and more limitation of certain motions. The Barlow and Ortolani signs should be sought in the newborn (Fig. 105-7). A positive Barlow sign consists of the ability to dislocate the hip; a positive Ortolani sign is the ability to relocate the hip with easy physical manipulation. When performing the tests, the child should be relaxed by keeping him or her warm and on the parent’s lap, and using a pacifier. Only one hip should be examined at a time. The pelvis should be held by one hand of the examiner, whereas the other hand controls the femur with fingers on the greater and lesser trochanters. With adduction
and posteriorly directed pressure, the femur can be felt to slide posterosuperiorly over the deformed acetabulum in the abnormal hip (Barlow sign; Fig. 105-5A) and back in with abduction, causing a dull clunk (Ortolani sign; Fig. 105-5B). Thus these signs, dislocation and relocation, are both aspects of the same condition of hip instability.
and posteriorly directed pressure, the femur can be felt to slide posterosuperiorly over the deformed acetabulum in the abnormal hip (Barlow sign; Fig. 105-5A) and back in with abduction, causing a dull clunk (Ortolani sign; Fig. 105-5B). Thus these signs, dislocation and relocation, are both aspects of the same condition of hip instability.
Possible errors include examining both hips at once, which impairs proprioception, and mistaking insignificant soft-tissue “clicks” for the more important and palpable “clunk.” These innocent clicks may be due to movement of fascia over the greater trochanter, clicking of the meniscus or the patella, or the stretch of a normal labrum.
Routine screening of neonates since the 1970s has resulted in a dramatic increase in early diagnosis of DDH (21), and thus more successful treatment (22). Approximately 60% of all unstable newborn hips spontaneously become normal within the first 2 to 4 weeks as perinatal laxity resolves. A severely dysplastic hip may have a negative examination due to lack of an acetabular shelf. It is important to stress, however, that not all hips are reducible at birth. This is presumably because of development of dislocation earlier in utero, with evolution of fixed-joint contractures. Similarly, it is believed that a few cases of dysplasia may develop after birth. In most large series, it has been shown that not all abnormal hips can be detected by screening, even by skilled examiners (23). This is because the physical findings are variable and may fall within the range of normal. If the hip remains dislocated, contractures develop, so by the age of about 6 months most cases cannot be relocated on physical examination in the awake patient. Findings of asymmetry, such as limitation of abduction and of full extension, as well as apparent shortening of the thigh, are more sensitive at this time. This last sign, known as the Allis or Galeazzi sign, is noted by comparing the lengths of the two flexed thighs when held together. Asymmetry of skin folds by itself is unreliable and not a highly specific sign, although it is a supportive finding. When the child begins to walk, a positive Trendelenburg sign is noted during gait: When weight is borne on the dislocated side during gait, the pelvis inclines downward, dropping on the other side. Pain is not present, and walking may begin at about the normal age.
The surgeon should be especially alert to the possibility of DDH in children with connective tissue disorders, genetic syndromes, or neuromuscular disease.
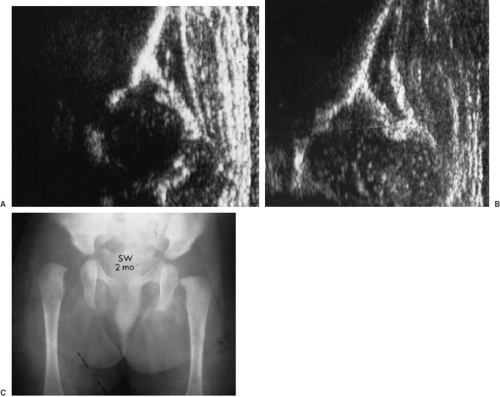
Except in teratologic conditions, radiographs are not commonly used before 6 months of age because interpretation is more difficult during this time; physical examination remains more reliable. Many centers are using ultrasonography as an objective tool, but interpretation requires much experience and should be performed by a pediatric radiologist or orthopedist who is familiar with the technique. Ultrasound is indicated for diagnosis if the neonatal examination is abnormal or questionable, as well as to guide initial treatment (22) (Fig. 105-8A and 105-8B). As the infant grows, plain films may more clearly show cephalad and lateral migration of the femur with a break in the Shenton line (Fig. 105-6C), delayed appearance of the femoral ossific nucleus, a shallow and more vertical acetabulum, and, later, formation of a false acetabulum.
Treatment involves different measures at different ages. The aim of these measures is to restore contact between femoral head and acetabulum. Because a high percentage of patients experience spontaneous improvement of lax hip capsules in the early perinatal period, most orthopedists recommend observation of a mild subluxable type of hip, with reexamination at 3 weeks. Dislocated hips are treated at the time of diagnosis. An abduction-flexion device such as a Pavlik harness is most often used. This allows some motion while maintaining the appropriate femoral-acetabular contact. The alignment should be checked by ultrasound or radiography in 1 to 2 weeks (23). The brace is worn until the clinical and radiologic examinations are normal, a duration approximately equal to one to two times the child’s age at diagnosis. If treatment is begun after 6 months of age, the child is usually too large and active to tolerate the brace. Then reduction must be preceded by traction to bring the femoral head down toward the acetabulum, decreasing the muscle forces that could contribute to avascular necrosis. A manipulative (closed) reduction is thus attempted under general anesthetic (24). If closed reduction is not successful, open surgical reduction should be carried out. This involves tightening the lax superior capsule and releasing the tight psoas tendon and inferior capsule, allowing the femoral head to be brought down to its appropriate location.
If there is extensive bony deformation, such as a shallow acetabulum or rotated femur, a femoral or pelvic osteotomy and open reduction might be indicated. This is more common after the age of 2 years.
Possible complications include persistent dysplasia from failure of normal development, redislocation, and avascular necrosis of the femoral head. The last condition is due to impairment of the epiphyseal vessels by excess pressure or capsular stretch. It is the most serious complication. Its occurrence is more likely if the hip is reduced under excessive tension or if excessive abduction is used.
The earlier treatment is carried out, the better is the resultant hip development and the safer each of the steps in treatment. Early detection, when possible, can decrease the need for complex orthopedic procedures later.
Transient (toxic) synovitis of the hip is a diagnosis of exclusion; it is a self-limited condition that is the most common cause of an irritable hip in children. The usual presentation is a painful limp or hip pain of acute or insidious onset, usually occurring unilaterally. The most common ages are 2 to 6 years, but patients from 1 to 15 years have been reported (25). There is moderate spasm on testing of hip range of motion, particularly internal rotation. Temperature, white blood cell count, C-reactive protein, and erythrocyte sedimentation rate may be normal or slightly elevated. The etiology is unknown; an immune mechanism and viral infection have been postulated. Some examples of viral-associated anthropathy have been described. Differential diagnosis should include septic arthritis, osteomyelitis, and Legg-Calvé-Perthes disease, which usually has a subchondral crescent of lucency or further changes in the femoral head on radiograph. Juvenile rheumatoid monarthritis and slipped capital femoral epiphysis should also be considered. Admission to hospital, observation, and early aspiration should be performed if septic arthritis cannot be ruled out. Treatment consists of bed rest with oral analgesics as needed for 2 to 7 days. This can sometimes be performed on an outpatient basis with frequent follow-up if septic arthritis is ruled out. Persistence of symptoms beyond 1 week should prompt the physician to perform reevaluation, although persistence of symptoms for as long as 1 month has occasionally been reported.
Legg-Calvé-Perthes disease was first differentiated from tuberculosis within a decade after clinical use of radiography at the turn of the century, but its etiology is still unknown. This disorder consists of ischemia of the proximal femoral epiphysis (26). The amount of the femoral epiphysis rendered ischemic is variable and affects the outcome. The ischemia is followed by resorption, then reossification with or without collapse of the femoral head. It most commonly affects children 4 to 8 years old, although exceptions are often seen. Males are affected four times as often as females. Affected patients as a group have slightly shorter stature and delayed bone age compared with peers. Fifteen percent of cases are bilateral, although both sides are not usually affected at the same time.
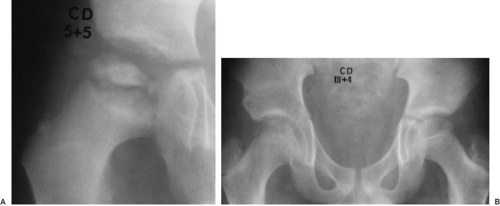
Clinical presentation is usually a limp, such as abductor lurch, with minimal pain of either short or long duration. The pain is not as acute or severe as that of transient synovitis or septic arthritis. Motions that are especially limited are internal rotation and abduction of the hip. Internal rotation is performed with the patient supine, the hip flexed, measuring the angle to which the leg may be rotated laterally. These movements may be resisted by mild spasm or guarding. At the earliest stage, radiographs may be normal or may reveal the slightly smaller size of the affected femoral epiphysis compared with the other side due to its temporary inhibition of growth (27,28). Later, there may be a narrow crescentic lucency, best seen on the lateral view (28), which is due to a microfracture of the bone just underneath the joint surface. This reveals the extent of bone involved. In some cases, revascularization may occur without collapse of the epiphysis, but in others, revascularization of the femoral head is accompanied by progressive resorption and deformation (Fig. 105-9). Reossification follows, and the femoral head continues to grow. Whether this further growth occurs spherically
depends on the patient’s age, the amount of collapse, and the method of treatment.
depends on the patient’s age, the amount of collapse, and the method of treatment.
Differential diagnosis should include transient synovitis, septic arthritis, hematogenous osteomyelitis, sickle cell infarct, hemoglobinopathies, steroid-induced necrosis, Gaucher’s disease, hypothyroidism, and the epiphyseal dysplasias. The last two are often synchronous bilaterally, whereas Legg-Calvé-Perthes is not. Avascular necrosis may also be a serious complication of femoral neck fracture or hip dislocation.
Treatment follows two principles: containment of the femoral head within the acetabulum and maintenance of range of motion. In the early stages of Perthes disease, the avascular portion of the femoral head is less likely to become deformed and more likely to regrow spherically if contained within the mold of the acetabulum by abduction. Children younger than 6 years of age or with involvement of less than one-half of the femoral head may be followed without active treatment if a full range of motion is preserved; patients in this age group have a good prognosis.(26) More aggressive treatment is indicated in patients with involvement of more than one-half of the femoral head or age older than 6 years.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree