Background
Human papillomavirus and Chlamydia trachomatis share the same route of sexual transmission and possess similar risk factors, indicating that coinfection may act synergistically in the induction of epithelial cell abnormalities.
Objective
This study aimed to determine the prevalence of human papillomavirus and Chlamydia trachomatis in adolescents and young women and identify factors associated with coinfection.
Study Design
This cross-sectional study included 276 female participants, aged 15–24 years, who were sexually active. Interviews were conducted and cervical specimens were collected for cervical smears and molecular tests. All cervical specimens were tested for 27 human papillomavirus genotypes by polymerase chain reaction amplification and hybridization to a human papillomavirus linear array. Detection of Chlamydia trachomatis was performed by polymerase chain reaction using primers directed to the region encoding the cryptic plasmid. Bivariate and multivariate analyses were performed to evaluate the factors associated with coinfection with human papillomavirus and Chlamydia trachomatis . The odds ratio, the adjusted odds ratio, and the 95% confidence interval were calculated.
Results
The prevalence of infection by Chlamydia trachomatis and human papillomavirus was 9.1% (95% confidence interval, 5.61–12.4) and 47.1% (95% confidence interval, 41.0–53.2), respectively. The prevalence of coinfection with human papillomavirus and Chlamydia trachomatis was 5.8% (95% confidence interval, 3.3–9.2); coinfection with 1 human papillomavirus type was 3.3% (95% confidence interval, 1.5–6.1) and with multiple types was 2.5% (95% confidence interval, 1.0–5.2). The prevalence of cytological abnormalities was 12.3% (95% confidence interval, 8.6–16.79). Human papillomavirus infections of high oncogenic risk were more prevalent (85.4%). Factors independently associated with coinfection of human papillomavirus/ Chlamydia trachomatis obtained by multivariate analysis were the initiation of sexual activity under 16 years of age with an an odds ratio of 4.9 (95% confidence interval, 1.0–23.63; P = .05) and cytological abnormalities with an odds ratio of 10.7 (95% confidence interval, 1.9–59.5; P = .01), which indicates there is risk for the detection of cytological abnormalities in adolescents and young women coinfected with human papillomavirus/ Chlamydia trachomatis .
Conclusion
The prevalence of coinfection among our study population was of a magnitude that warrants attention by public health services. Adolescents and young women should be monitored for Chlamydia trachomatis infection and vaccinated against human papillomavirus. The association between cytological abnormalities and coinfection with human papillomavirus and Chlamydia trachomatis indicates the potential synergistic role of these infections in carcinogenesis of the cervix.
Coinfection by human papillomavirus and Chlamydia trachomatis is an important public health problem owing to the high prevalence in young women. Human papillomavirus is considered a critical factor in the development of cervical cancer, and there is evidence that infection by Chlamydia trachomatis acts in a synergistic manner facilitating infection and reinfection by human papillomavirus and contributing to the viral persistence that is necessary for the process of carcinogenesis. However, Zhu et al in a meta-analysis study have demonstrated that individuals infected with Chlamydia trachomatis have a higher risk of cervical cancer. Nevertheless, some studies have shown conflicting results. In fact, in a systematic review, Ghosh et al showed that there is heterogenecity of data regarding a causal association of Chlamydia with cervical cancer; reports differ according to the population studied.
There are indications that women infected with Chlamydia trachomatis are at increased risk of persistent human papillomavirus infection compared with uninfected women. In addition, young women with chronic Chlamydia trachomatis infection have a high prevalence of infection with multiple human papillomavirus types.
The prevalence of human papillomavirus and Chlamydia trachomatis infections is higher in young women, and factors that are associated with their acquisition, such as age and a greater number of sexual partners, are also shared. Coinfection with Chlamydia trachomatis and human papillomavirus may increase a woman’s risk of developing cervical neoplasia.
Adolescents and young women are a vulnerable group of the population with regard to sexually transmitted diseases. This is thought to be because of the relative immaturity of the genital tract, making it prone to both trauma and infection, particularly in the developing transformation zone of the cervix. The cells that are the primary target for infection may be those close to the squamocolumnar junction, such as the epithelial reserve cells that lie immediately underneath the columnar epithelium of the endocervix and that eventually form the stratified epithelial layers of the transformation zone as the cervix matures. For some time now, the general hypothesis has been that lesion formation begins with the infection of a stem cell and that the longevity of the stem cells is a key factor in the formation of a persistent lesion.
Information on the prevalence of coinfection with human papillomavirus and Chlamydia trachomatis in different age groups, especially in adolescents and sexually active asymptomatic young women, is limited. This study aimed to determine the prevalence of coinfection with human papillomavirus and Chlamydia trachomatis in these 2 groups of the population and to investigate the potential predisposing factors such as sexual behavior, gynecological and obstetric background, and cytological abnormalities.
Materials and Methods
Study design
This study was part of a bigger project conducted in the cities of the central-west region of Brazil from 2007 to 2009. The design and study population have been described previously. The population of these cities at the time of the study was 141,046 inhabitants, with an estimated 4500 women under the age of 25 years monitored by the Family Health Program. These cities were selected randomly to represent the urban population outside the capital, in central-west Brazil.
Study population and sampling
All women aged between 15 and 24 years, monitored by the Family Health Program, were potentially eligible. Census information was provided by the local health department. The sample size was calculated using the Open Source Epidemiologic Statistics in the Public Health software (OpenEpi version 2.3.1). The number of participants was found to be 646 nonpregnant sexually active women, aged between 15 and 24 years, based on a minimum predicted prevalence of sexually transmitted infections of 2.0%, with an estimated accuracy of 1.0% and a 95% confidence interval.
For these calculations, syphilis was considered the sexually transmitted infection with the lowest prevalence. Considering that approximately 20% of young women could not be located at the registered address, 40% had not initiated sexual activity (not eligible), 10% were pregnant or had used antibiotics in the last 15 days (not eligible), and there was a refusal rate of 25%, the final sample was estimated as 1250 women.
The local health department provided a list of households with potential participants (women aged 15–24 years registered at a family health care unit). A number was assigned to each potential participant, and simple sampling was carried out using random numbers generated by a computer (Epi Info version 3.4). From a population of approximately 4500 young women, 1250 were invited by letter to attend the closest family health care unit. In the second phase, all of the women who accepted the invitation and met the inclusion criteria were included in the study.
Our study was conducted in one of the cities with a population of 46,786 inhabitants monitored by the Family Health Program, which had 13 service units. In total, 651 adolescents and young women were recruited. More than 65% of these (4n = 28) reported being sexually active and were invited to participate ( Figure ).
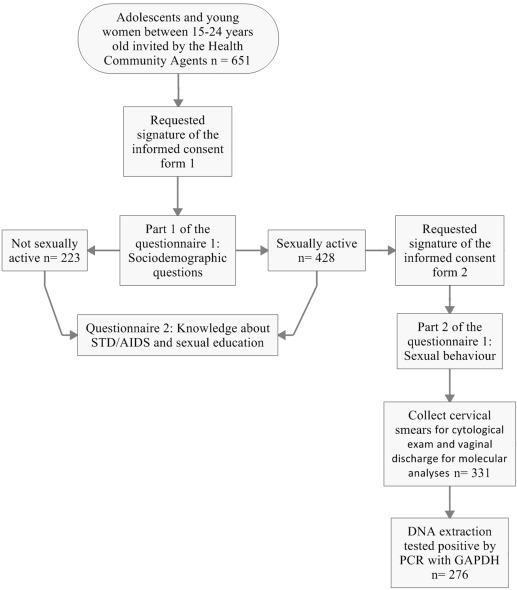
The study protocol was approved by the institute’s internal review board (CAAE0042.0.168.000-08), and all patients signed an informed consent form. The collection of cytological and cervical samples was conducted in 331 adolescents and young women, DNA was successfully extracted from 276 of these samples, and these samples were therefore included in the study ( Figure ).
Data collection
Data were obtained using a structured questionnaire including demographics; age; education level; maternal education; household income (measured in units relating to the Brazilian minimum wage: 213 USD at the time of the study); sexual behavior; and gynecological and reproductive background, including age at first intercourse, number of partners, condom use, and number of pregnancies. Participants who reported the use of antibiotics in the last 15 days and those who were pregnant were excluded.
Sample processing
A cervical sample was taken for a second conventional smear test using a cervical brush, and the residual material was rinsed with and then stored in 1.0 mL universal collection medium (QIAGEN Sample and Assay Technologies, São Paulo, Brazil) for human papillomavirus and Chlamydia trachomatis DNA testing.
Cervical cytology assessment
Conventional cervical smears were screened at the Cytology Laboratory, Federal University of Goiás, Goiânia, Brazil, which performs rapid rescreening of all negative cytology smears as a quality-control measure. The suitability of the samples and the degree of abnormalities were classified in accordance with the 2001 Bethesda System.
DNA extraction
DNA extraction was performed using purification reagents and a method based on the selective binding of DNA to a silica membrane in the presence of chaotropic salts (PureLink; Invitrogen, Carlsbad, CA). First, 200 μL of the universal collection medium solution containing the cervical sample was added to 20 μL of proteinase K and 20 μL of ribonuclease. After this lysis step, 200 μL of a 96% ethanol solution was added and the mixture was applied to the column, and the purification procedure was performed according to the 3 steps described on the manufacturer’s instructions. The DNA bound to the column was then extracted and stored at −20°C.
Human papillomavirus-DNA testing
For detection and genotyping of human papillomavirus DNA, a genotyping protocol using a linear array (Roche Molecular Systems Inc, Pleasanton, CA) was used. Human papillomavirus genotyping used biotinylated indicators to define a region of the L1 nucleotide sequence of the human papillomavirus genome via the specific primer set PGMY09/PGMY11, which amplifies a fragment of 450 bp. This set of primers is able to amplify 37 human papillomavirus types: 6,11, 16, 18, 26, 31, 33, 35, 39, 40, 42, 45, 51, 52, 53, 54, 55, 56,58, 59, 61, 62, 64, 66, 67, 68, 69, 70, 71, 72, 73 (MM9), 81, 82 (MM4), 83 (MM7), 84 (MM5) IS39, and CP6108. Primers to amplify the β-globin gene, GH20, and PC04 were also included as a positive control.
The reagents used for polymerase chain reaction were as follows: 100 μL of amplification mixture with 4 mM MgCl 2 ; 50 mM KCl; 7.5 U AmpliTaq Gold DNA polymerase (Perkin-Elmer, Foster City, CA); 200 mM of each deoxyadenosine triphosphate, deoxycytosine triphosphate, and deoxyguanosine triphosphate; 600 mM deoxyuridine triphosphate; 100 pmol of primers PGMY09/PGMY11; and 2.5 pmol of primers GH20/PC04 labeled with biotin.
The amplification profile was as follows: AmpliTaq Gold activation for 9 minutes at 95°C, denaturation for 1 minute at 95°C, annealing for 1 minute at 55°C, and extension for 1 minute at 72°C for a total of 40 cycles, followed by a terminal extension step for 5 minutes at 72°C. The amplified products were separated on an 8% polyacrylamide gel, using 100-bp molecular weight markers, and visualized by staining with silver nitrate.
After polymerase chain reaction amplification, the β-globin and human papillomavirus amplicons were chemically denatured with a denaturation solution to form single-stranded DNA. Aliquots of denatured amplicon were transferred to the typing tray containing hybridization buffer and the genotyping strip, the linear array human papillomavirus, which was coated with the human papillomavirus DNA and β-globin.
After the hybridization reaction, the genotyping strip was rigorously washed to remove any unbound material. Streptavidin-peroxidase conjugate was added to the strip, which binds to the amplicons hybridized to the biotin-labeled oligonucleotide probes. The strip was washed to remove the substrate, and then a substrate solution containing hydrogen peroxide and 3,3′,5,5′-tetramethylbenzidine was added. The strip was visually interpreted by comparing the pattern of blue bands shown on the manufacturer’s instructions (genotyping reference guide human papillomavirus linear array; Roche Molecular Systems Inc).
Chlamydia trachomatis -DNA detection
Genomic DNA extraction from Chlamydia trachomatis was performed using the commercial Ultra Clean kit (Mobio Laboratories Inc, Carlsbad, CA) according to the manufacturer’s specifications. The hybrid capture technique was employed using 500 μL of the denatured DNA sample. The final elution volume was 50 μL.
The AMPLICOR Chlamydia trachomatis / Neisseria gonorrhoeae test was used for the amplification of Chlamydia trachomatis DNA, a multiplex qualitative assay that allows for the amplification of Chlamydia trachomatis DNA, Neisseria gonorrhoeae , and the internal control reaction, simultaneously. A 25 μL aliquot of the denatured amplified DNA was added to 100 mL of hybridization buffer in 2 microplates coated with oligonucleotide probes complementary to the Chlamydia trachomatis target DNA sequence and the internal control sequence, respectively.
The plates were incubated for 1 hour at 37°C and then washed 7 times with wash buffer. After this, 100 mL of the avidin-peroxidase conjugate was added, and the plates were incubated again at 37°C and washed 7 times for 15 minutes. The substrate containing hydrogen peroxide and 3,3′,5,5′-tetramethylbenzidine was prepared fresh, and then 100 mL was immediately added to the plates. After 10 minutes in the dark at room temperature, the reaction was stopped by the addition of 100 μL of sulfuric acid. The absorbance was determined at 450 nm on a microplate reader (Behring EL 311, Hoechst, Akasaka, Japan).
Samples were considered negative if the optical density was <0.2, with the internal control optical density was ≥0.2. Samples were considered positive if the observed optical density was ≥0.8, regardless of the internal control optical density. If a sample presented an optical density of ≥0.2 but <0.8, the result was considered inconclusive and the test was repeated. In the case of reaction inhibition (ie, when the sample and internal control gave an optical density <0.2), the polymerase chain reaction was repeated, diluting the sample to 1:10.
Data analysis
A descriptive analysis was performed of the sociodemographic and behavioral characteristics of subjects and their gynecological and obstetrical backgrounds. The results of the diagnostic sample tests were also analyzed. The normal distribution of variables was expressed by the average and SD and categorized according to the average values.
The prevalence of human papillomavirus/ Chlamydia trachomatis coinfection was calculated along with their respective 95% confidence intervals. The potential risk factors for coinfection were evaluated using a bivariate and multivariate logistic regression analysis. The results were compared with uninfected participants for the calculation of odds ratios, both unadjusted and adjusted to 95%. Variables with values of P < .20 in the bivariate analysis were included in the multivariate model. Values of P < .05 were considered significant. Analysis was conducted with SPSS software (version 16; SPSS Inc, Chicago, IL).
Results
The study included 276 participants aged between 15 and 24 years; the average age was 19.5 years and the SD was 2.6 years. Of these participants, 148 (53.6%) were adolescents and 128 (46.4%) were young women, according to the World Health Organization classification. The absence of a stable marital union was reported by 172 participants (37.5%), and a family income of less than 4 minimum wages was reported by 235 participants (86.5%).
The onset of sexual activity after 16 years was reported by 97 participants (35.1%), and 39 subjects (14.8%) reported more than 4 sexual partners prior to the study. Condom use during intercourse in all cases was reported by 46 participants (16.7%) and 93 subjects (34.1%) reported at least 1 pregnancy ( Table 1 ).
| Variables | n | % |
|---|---|---|
| Age, y | ||
| 15–19 | 148 | 53.6 |
| 20–24 | 128 | 46.4 |
| Average (SD) | 19.5 (2.6) | |
| Marital status | ||
| No common-law marriage | 172 | 37.7 |
| Married/stable union | 104 | 62.3 |
| Family income, minimum wage a | ||
| Below 4 | 235 | 86.1 |
| Above 4 | 38 | 13.9 |
| Age at the first intercourse, y | ||
| 16 and younger | 179 | 64.8 |
| Older than 16 | 97 | 35.1 |
| Number of sexual partners b | ||
| ≤4 | 236 | 85.8 |
| >4 | 39 | 14.2 |
| Preservative use c | ||
| Always | 46 | 16.7 |
| Never/occasionally | 229 | 83.3 |
| Pregnancy background d | ||
| Yes | 93 | 34.1 |
| No | 180 | 65.9 |
a Three participants without information
b One participant without information
c One participant without information
The prevalence of infection by Chlamydia trachomatis and human papillomavirus was 9.1% and 47.1%, respectively. The prevalence of Chlamydia trachomatis infection was greater in adolescents and young women positive for human papillomavirus infection, although, this difference was not statistically significant; however, the value of P = .076 may indicate a tendency for higher Chlamydia trachomatis prevalence in adolescents and young women positive for human papillomavirus ( Table 2 ).
| CT-DNA | HPV-DNA positive | HPV-DNA negative | Total | OR (95% CI) |
|---|---|---|---|---|
| CT-DNA (positive) | 16 (12.3%) | 9 (6.2%) | 25 (9.1%) | 2.15 (0.85–5.46) |
| CT-DNA (negative) | 114 (87.7%) | 137 (93.8%) | 251 (90.9%) | |
| Total | 130 (47.1%) | 146 (52.9%) | 276 (100%) |
The total prevalence of human papillomavirus was 49.0% (103 of 209) in women with negative cytological results and 82.3% (28 of 34) in women diagnosed with positive cytological results. The prevalence of human papillomavirus infection in women with atypical squamous cells of undetermined significance was 76.5% (13 of 17), 82.0% (9 of 11) in women with low-grade squamous intraepithelial lesions, 100% (1 of 1) in women with atypical squamous cells-cannot exclude high-grade squamous intraepithelial lesions, 100% (4 of 4) in cases of high-grade squamous intraepithelial lesions, and 100% (1 of 1) with atypical glandular cells.
With respect to Chlamydia trachomatis , the overall prevalence was 7.4% (18 of 243) in women with negative cytology results, 23.5% (4 of 17) in women with atypical squamous cells of undetermined significance, 18.2% (2 of 11) in women with low-grade squamous intraepithelial lesions, and 100% (1 of 1) in women with atypical squamous cells-cannot exclude high-grade squamous intraepithelial lesions (data not shown).
Table 3 shows the prevalence of infection by Chlamydia trachomatis , human papillomavirus, and human papillomavirus/ Chlamydia trachomatis coinfection and the prevalence of cytological abnormalities in this population. The prevalence of Chlamydia trachomatis infection was 9.1% (95% confidence interval, 5.61–12.4).
| Variables | n | % | 95% CI |
|---|---|---|---|
| CT infection a | 25 | 9.1 | (5.61–12.4) |
| HPV infection | 130 | 47.1 | (41.0–53.2) |
| Only HPV-type infection | 72 | 26.1 | (21.3–32.1) |
| Multiple types of HPV infection | 56 | 20.2 | (15.8–25.6) |
| CT/HPV coinfection | 16 | 5.8 | (3.3–9.2) |
| CT coinfection/only type HPV | 9 | 3.3 | (1.5–6.1) |
| CT coinfection/multiple type HPV | 7 | 2.5 | (1.03–5.16) |
| Cytological abnormalities | 34 | 12.3 | (8.6–16.79) |
| ASC-US | 17 | 6.2 | (3.6–9.7) |
| LSIL | 11 | 4.0 | (2.0–7.0) |
| HSIL | 4 | 1.4 | (0.4–3.7) |
| ASC-H | 1 | 0.4 | (0.0–2.0) |
| AGC | 1 | 0.4 | (0.0–2.0) |
Among the 276 study participants, 36 types of human papillomavirus were detected, with a prevalence of 47.1% (95% confidence interval, 41.0–53.2). In 26.1% of participants (95% confidence interval, 21.3–32.1), the infection was from 1 human papillomavirus type, whereas in 20.2% of participants (95% confidence interval, 15.8–25.6), more than 1 type of human papillomavirus was detected.
Of the human papillomavirus types present in the currently available vaccines, human papillomavirus-16 was the most frequently detected (27.7%), followed by human papillomavirus-18 (2.6%) and human papillomavirus-6 (1.9%); by contrast, human papillomavirus-11 was not detected in this study.
The prevalence of simultaneous infection by Chlamydia trachomatis and human papillomavirus was 5.8% (95% confidence interval, 3.3–9.2). When analyzed further, the prevalence of simultaneous infection by Chlamydia trachomatis and a single human papillomavirus type was 3.3% (95% confidence interval, 1.5–6.1), compared with a prevalence rate of 2.5% (95% confidence interval, 1.03–5.16) for coinfection by Chlamydia trachomatis and more than 1 human papillomavirus type.
The prevalence of cytological abnormalities among the study population was 12.3% (95% confidence interval, 8.6–16.79); 6.2% were represented by a diagnosis of atypical squamous cells of undetermined significance, 4.0% by low-grade squamous intraepithelial lesions, 1.4% by high-grade squamous intraepithelial lesions, and 0.4% by atypical squamous cells-cannot exclude high-grade squamous intraepithelial lesions and atypical glandular cells.
The results of bivariate analysis revealed that the participants who became sexually active at 16 years of age were 5.0 times more likely (95% confidence interval, 1.1–22.8; P = .04) to become coinfected with Chlamydia trachomatis and human papillomavirus compared with those who became sexually active after 16 years of age.
This breakpoint was chosen according to a study that evaluated the risk factors associated with human papillomavirus positivity and with a diagnosis of cervical neoplasia. These authors showed that first sexual intercourse before 16 years of age was significantly associated with a positive human papillomavirus test.
Participants possessing cytological abnormalities were 14.9 times more likely (95% confidence interval, 3.0–74.4; P = .01) to become infected. There were no significant associations between infection and participants who were 19 years of age, had no stable marital union, or had a family income of less than 4 minimum wages, which showed odds ratios of 1.8 (95% confidence interval, 0.6–5.2; P = .28), 1.8 (95% confidence interval, 0.6–5.5; P = .29), and 0.40 (95% confidence interval, 0.1–1.4; P = .15), respectively.
There were also no significant associations with condom use and pregnancy history, which showed odds ratios of 0.9 (95% confidence interval, 0.2–3.6; P = 0.91) and 0.6 (95% confidence interval, 0.2–1.9; P = .36), respectively. The variables associated with coinfection of human papillomavirus and Chlamydia trachomatis were then included in a hierarchical logistic regression model. After controlling for confounding factors, these combinations of variables remained associated with cytological abnormalities (odds ratio, 10.7; 95% confidence interval, 1.9–59.5; P = .01) ( Table 4 ).



