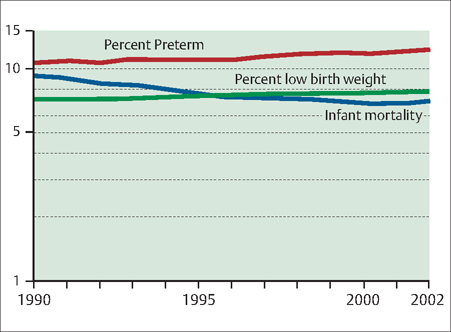
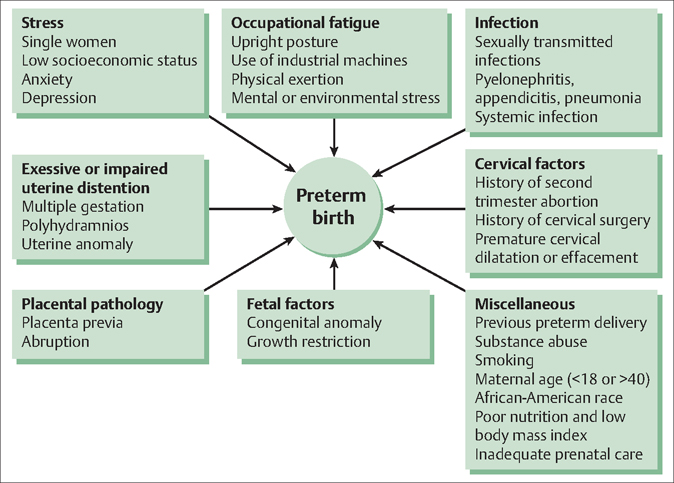
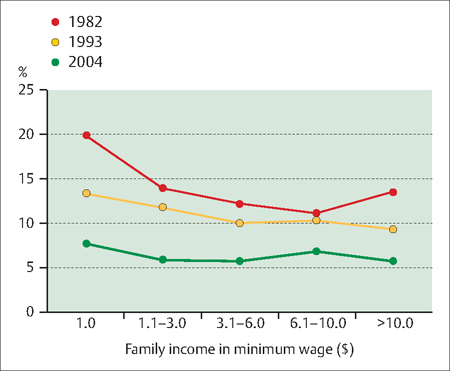
15 Pathological Labor and Delivery Adi Y. Weintraub, Fernanda Press and Arnon Wiznitzer In order for labor and delivery to occur, uterine quiescence, which is the norm throughout pregnancy, is disrupted. Labor and delivery begin when regular uterine contractions activate and continue to the delivery of the fetus and the placenta. For a successful delivery, the fetus should be lying longitudinally, the presenting part is usually vertex, and there are effective contractions and an adequate relation between maternal pelvis and the passenger (i. e., the fetus). These conditions are termed the three “P’s” for: An abnormal labor is defined as labor dystocia (see Definitions below) and refers to any deviation from the norm. The causes of abnormal labor may include maternal pathologic conditions (related or unrelated to gestation), fetal abnormalities, or problems in the relationship between both. This chapter will focus on pathologies in the timing of labor, most notably preterm labor, and problems that occur during labor and delivery, or abnormal labor. Cervical insufficiency: Also called incompetent cervix, this is a condition where the cervix begins to dilate during pregnancy (without contractions) before the fetus is ready to be born, such as in the second trimester. Depending on the point in pregnancy at which this occurs, cervical insufficiency can lead to miscarriage, stillbirth, or preterm delivery. Cervical insufficiency tends to be a recurring problem. Cervical ripening: Refers to a change in the cervix with respect to its readiness to become softer, more fexible, more distensible, and shorter during the final weeks of pregnancy. These cervical changes can also be chemically induced (i. e., induced labor). Contractility: This property relates to the ability of the uterus to shrink or contract. Cervicovaginal secretions: Secretions that contain cytokines of maternal origin, inflammatory cells, and proteolytic enzymes, which act to protect the intra-amniotic compartment from infectious agents that may ascend along the birth canal. Dystocia: A slow or difficult labor or delivery caused by an obstruction or constriction of the birth passage or the abnormal shape, size, position, or condition of the fetus. Low birth weight neonates: Infants who weigh less than 2500 g at birth are regarded as low birth weight neonates. Those born with weights of 1500 g or less are considered very low birth weight neonates, and those who weigh less than 1000 g are defined as extremely low birth weight neonates. Preterm birth: A human birth that occurs before 37 completed weeks of gestation (less than 259 days) is called preterm birth (PTB). A very preterm birth is typically defined as one of less than 32–34 weeks’ gestation, and an extremely preterm birth is one that occurs at less than 28 weeks’ gestation. Infants born prematurely at 34–36 weeks’ gestation are referred to as “near-term” infants. Preterm Labor: Labor that begins after 20 weeks, when the fetus is considered viable and before the 37th week, when the fetus is considered full-term, is referred to as preterm labor (PTL). The use of transvaginal cervical ultrasonography and assays to detect fetal fibronectin (fFN) in cervicovaginal secretions has greatly improved the diagnosis of preterm labors that have a likelihood of leading to PTBs. The value of these tests is that, if they are negative, they can help the physician avoid unnecessarily hospitalizing or transferring a woman who is experiencing false PTL. Other bio-markers have been found to have some association with the timing of birth but are not routinely used to predict PTB in women with symptoms of PTL. PTL that eventually leads to preterm delivery affects approximately 5–7% of live births in developed countries. significantly higher rates are found in developing countries. Prematurity due to PTL is one of the leading causes of infant mortality and accounts for approximately 28% of neonatal mortality worldwide. Around 45–50% of PTBs are idiopathic, or spontaneous; 30% are related to premature rupture of membranes (PROM) (see Chapter 20); and another 15–20% are attributed to medically induced or elective preterm deliveries for maternal or fetal indications. The percentage of preterm and low birth weight deliveries has been increasing steadily since the mid-1980s. The preterm delivery rate has been reported to be 11% in the United States, between 5% and 7% in Europe, and approximately 6.5% in Canada. In the United States, there has been a 20% rise in the overall proportion of PTBs since 1990. However, due to better management of this condition, infant mortality rates in the United States have declined during this same period (Fig. 15.1). The major reason for the increase in PTBs is a higher rate of multiple gestation. The shift toward earlier delivery that is observed among singletons is even more profound among multiples. Between 1990 and 2005, the percentage of twins delivered preterm has risen from 48% to 60% with large increases seen among twins born both at less than 34 weeks, and at 34–36 weeks. A marked trend to shorter pregnancies is also observed among triplets. Additional contributors to the increase in the rate of PTBs include changes in obstetrical management (e. g., expanded use of ultrasound imaging and induction of labor for abnormal findings), patient demographic factors (e. g., more women giving birth at advanced maternal ages), and patient behavioral characteristics (Fig. 15.2). Income level also has been implicated in the rate of PTBs. Researchers, for example, studied the trends in PTBs, low weight births, and intrauterine growth restriction rates in southern Brazil from 1982 to 2004. During this time, they found a slight increase in the prevalence of low weight births from 9% to 10%. Intrauterine growth restriction decreased from 14.8% in 1982 to 12% in 2004, whereas PTBs more than doubled from 6.3% in 1982 to 14.7% in 2004. This dramatic increase in PTBs was only partially explained by pregnancy interruptions due either to caesarean sections or to labor inductions. When the investigators looked at other factors, they found that PTB rates more than doubled between 1982 and 2004 from 5.7% to 13.5% among higher income families (Fig. 15.3). Fig. 15.1 Infant mortality rate per 1000 preterm births, and low birth weight per 100 live births Rates are plotted on a log scale. Preterm is defined as less than 37 completed weeks of gestation and low birth weight as less than 2500 g Reproduced from the National Vital Statistics System, National Center for Health Statistics, Centers for Disease Control and Prevention. Birth weight and gestational age are the two most important predictors of an infant’s subsequent health and survival. Infants born too small or too soon or who weigh 2500 g or more have an increased risk of death or short-term and long-term disability than normal sized and weight infants born at term. There is a remarkable relationship between gestational age and infant mortality. Infant mortality falls exponentially until term. Because of their much greater risk of death, infants born at the lowest gestational ages have a large impact on overall infant mortality. For example, in the United States only 0.8% of births occurred at less than 28 weeks’ gestation, but they accounted for nearly half (46.4%) of all infant deaths in the United States in 2005. The morbidity associated with prematurity is equally concerning. Disability occurs in 60% of survivors of birth at 26 weeks and in 30% of those born at 31 weeks. The morbidity and mortality rates of near-term infants approach those of term infants, but are still higher. In one study, mortality rates at 34, 35, and 36 weeks of gestation were 0.11, 0.15, and 0.05%, respectively, compared with 0.02% at 39 weeks. Fig. 15.2 Risk factors for preterm birth. Fig. 15.3 Prevalence of preterm birth according to family income Pelotas, southern Brazil, 1982, 1993, and 2004. Preterm delivery is associated with immediate and long-term neonatal complications. Immediate neonatal complications include ventilator-treated respiratory distress, transient tachypnea, grade 1 or 2 intraventricular hemorrhage, sepsis work-ups, culture-proven sepsis, and hyperbilirubinemia. Intubation in the delivery room often is required to manage respiratory distress. Long-term morbidity for the child may include cerebral palsy, neurodevelopmental delay, chronic lung disease, and visual impairment. Greater uncertainty exists in the assessment of gestational age than in the assessment of birth weight (see Chapter 27, Posterm Pregnancy). Therefore, perinatal outcomes are often reported in terms of birth weight rather than gestational age, even though gestational age is a more predictive parameter. It should be noted that not all infants of low birth weight are premature; some are born at term but are small for gestational age, while others are both premature and appropriate for gestational age. Among preterm deliveries, approximately 80% occur spontaneously due to premature rupture of the membranes (PROM). Other reasons for spontaneous PTB include: Many risk factors have been associated with PTB (see Fig. 15.2). Approximately 10–30% are related to multiple gestations and other reasons, such as cervical insufficiency. Additionally, 20% are the result of iatrogenic intervention due to maternal or fetal indications. Clinical and laboratory evidence suggest a final common pathway leading to PTL and delivery, which may result from a number of different pathogenic processes. Table 15.1 presents pathological processes that are associated with preterm parturition. Intrauterine infection or inflammation is the most important process leading to PTB. It is the only factor for which causality has been directly established. Laboratory and clinical data show a link between spontaneous PTB and both systemic and ascending genital tract infections. Both clinical and subclinical chorioamnionitis are much more common in preterm than term deliveries, and may account for 50% of PTBs before 30 weeks’ gestation. Intrauterine infection is involved in 25–40% of preterm deliveries. Finding bacterial particles in the sterile amniotic fluid is always abnormal. One study found a positive amniotic fluid culture in 13% of women with PTL. When the process progressed to preterm delivery, the rate of positive cultures was 22%. When labor started with PROM, the rate was found to be 32% and as high as 75% during active labor in this group. A high rate of positive cultures was found in women with cervical insufficiency, those with a short cervix, and those with twins and PTL as well (Table 15.2). The final common pathway for triggering PTB is a maternal or fetal inflammatory response to infection in the amnion, chorion, or decidua. This response is characterized by the presence of activated neutrophils and macrophages that induce proinflammatory mediators, including interleukins (ILs) 1, 6, and 8; tumor necrosis factor-alpha (TNF-a); granulocyte colony-stimulating factor (G-CSF); and matrix metalloproteinases.
Preterm Labor
Definitions
Diagnosis
Epidemiology and Prevalence
Etiology and Pathophysiology of Preterm Birth
Intrauterine Infection/Inflammation
| Intrauterine infection/inflammation |
| Uterine ischemia |
| Uterine overdistension |
| Abnormal allograft reaction |
| Allergy |
| Cervical insufficiency |
| Hormonal disorders (progesterone related and corticotropinreleasing factor related) |
| Positive amniotic fluid culture | Percentage |
| Preterm labor | 13 |
| Progression to preterm delivery | 22 |
| Initial pPROM | 32 |
| Active labor in women with pPROM during active labor | 75 |
| Women with cervical insufficiency | 51 |
| Women with a shortened cervix (<25 mm by TVS) | 9 |
| Preterm labor in twins | 12 |
pPROM, preterm premature rupture of membranes;
TVS, transvaginal sonography.
In addition to inducing an inflammatory response, bacteria may also have a direct role in the pathogenesis of PTB. Some organisms (e. g., Pseudomonas, Staphylococcus, Streptococcus, Bacteroides, and Enterobacter) are capable of producing proteases, collagenases, and elastases that can degrade the fetal membrane. Bacteria also produce phospholipase A2 (which leads to prostaglandin synthesis) and endotoxin, a substance that stimulates uterine contractions and can cause PTL. The presence of bacteria, without an inflammatory response, does not always lead to an adverse outcome.
Uterine Ischemia
Maternal and fetal vascular lesions are second only to inflammatory lesions as a factor in PTB. Such lesions are the most common pathological features in the placenta of women with PTB. Maternal lesions observed in the placenta of patients with a spontaneous PTB include failure of physiological transformation of the myometrial segment of the spiral arteries, atherosis, thrombosis of the spiral arteries (a form of decidual vasculopathy), and a combination of these lesions. Fetal lesions may include a decrease in the number of arterioles in the villi and fetal arterial thrombosis. Uteroplacental ischemia could be the cause of PTL in women with placental vascular lesions.
The precise mechanisms responsible for the onset of PTB in women with uteroplacental ischemia have not been determined. Some of these proposed mechanisms include a role for the following:
- The renin—angiotensin system: Fetal membranes are rich in functional renin—angiotensin system, and uterine ischemia increases the production of uterine rennin.
- Angiotensin II: Myometrial contractility can be induced directly by angiotensin II or through the release of prostaglandins.
- Thrombin: When uteroplacental ischemia is severe enough to lead to decidual necrosis and hemorrhage, thrombin may activate the common pathway of parturition. Also, fetal vascular lesions (i. e., abnormal development due to defective angiogenesis or fetal thrombosis) may lead to fetal compromise and PTL.
Uterine Overdistension
Women with müllerian duct abnormalities, polyhydramnios, and multiple pregnancies are at increased risk for spontaneous PTL and PTB. Intra-amniotic pressure remains relatively constant throughout gestation despite the growth of the fetus and placenta. This has been attributed to progressive myometrial relaxation caused by the effects of progesterone and endogenous myometrial relaxants such as nitric oxide. Stretching can, however, induce increased myometrial contractility, prostaglandin release, expression of gap junction protein or connexin-43, and increased oxytocin receptor expression in the myometrium of pregnant and nonpregnant women.
Progesterone inhibits the gene expression of a protein that is associated with stretch-induced contraction. The effect of stretch increases in late gestation. It is at its maximum level during labor as a result of the relative reduction in uterine growth compared with fetal growth, as well as due to declining circulating and/or local concentrations of progesterone. Not only may stretch induce increased myometrial contractility, it may also modify the contractile response through “mechanoelectrical feedback” similar to that seen in the heart. The chorioamniotic membranes are distended by 40% at 25–29 weeks of gestation, 60% at 30–34 weeks of gestation, and 70% at term.
Mechanical forces associated with uterine overdistension may result in activation of mechanisms leading to membrane rupture. In women with multiple gestations, premature cervical ripening is seen as well as certain müllerian duct anomalies (e. g., incompetent cervix in diethylstilbestrol-exposed daughters).
Abnormal Allograft Reaction
The fetoplacental unit is considered nature’s most successful “graft.” Reproductive immunologists have suggested that abnormalities in the recognition and adaptation to a set of foreign antigens (fetal) may be responsible for recurrent pregnancy loss, intrauterine growth restriction, and pre-eclampsia.
It has been observed that some women in PTL, without demonstrable infection, have elevated concentrations of the IL-2-soluble receptor. Also seen is an inverse pattern in IL-2 and IFN-gamma production in peripheral blood between weeks 20 and 30 in preterm delivery compared with patients delivering at term. Elevated plasma concentrations of the IL-2 receptor are an early sign of rejection in women with renal transplants.
The complement system is a group of proteins that are activated during an inflammatory response triggered by foreign invaders. It plays a central role in the first line of defense against invading pathogens, and its activation involves the release of potent pro-inflammatory mediators (C3a, C4a and C5a). Recent studies support the hypothesis that some components of the innate limb of the immune response may have a role in the development of PTL.
Allergy
Another potential mechanism for PTL and PTB is an immunologically mediated phenomenon induced by an allergic mechanism. There is some evidence that an allergylike immune response (type I hypersensitivity) is associated with PTL. However, this finding remains controversial.
Cervical Insufficiency
Although cervical insufficiency is traditionally considered a cause of midtrimester miscarriage, a wide spectrum of related diseases probably exists. This spectrum includes recurrent pregnancy loss in the midtrimester, some forms of PTL (presenting with bulging membranes in the absence of significant uterine contractility or rupture of membranes), and probably precipitous labor at term.
Cervical disease may be the result of:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


