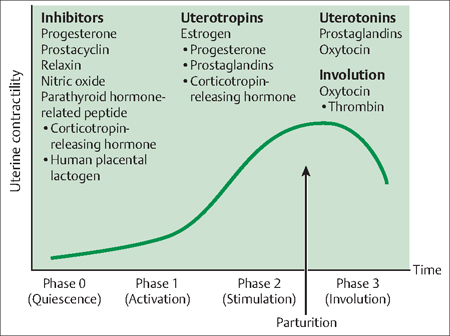
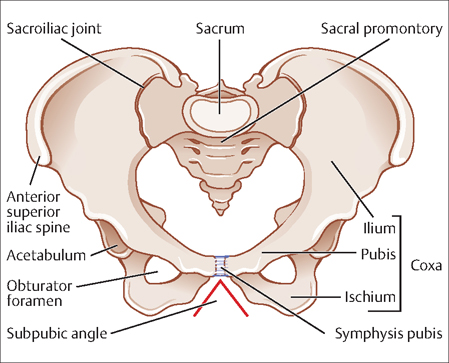
11 Labor and Delivery Vanina S. Fishkel and Gustavo F. Leguizamòn This chapter reviews the determinants of human parturition, or labor. Labor is a physiologic process consisting in organized uterine contractions of adequate intensity, frequency, and duration to affect complete cervical dilatation and expulsion of the fetus, placenta, and fetal membranes through the birth canal. Labor progresses from a state of uterine quiescence (latent phase) to a phase characterized by uterine contractions and cervical dilatation (active phase). Maternal structures (e.g., pelvis) and functions (e.g., uterine contractions) as well as fetal structures (e.g., presenting parts) and functions (e.g., fetal cardinal movements) are of utmost importance in the progression of labor. The physiology of term labor initiation is not fully elucidated, but during the past several decades significant information has been added to our understanding of this process. Uterine activity can be classified as having four distinct phases (Fig 11.1): Fig. 11.1 Uterine activity in pregnancy Adapted from Challis JRG, Gibb W: Control of Parturition Prenatal and Neonatal Medicine 1996;1:283. Adequate interaction between the fetus’ features and maternal pelvis allows vaginal delivery. Thus, maternal contractions to propel the fetus through the birth canal and the ability of the fetus to pass through the mother’s pelvic bones are crucial to successful labor and birth. Uterine contractions are characterized by the following measurable parameters: Amplitude or intensity: The ability of the external tocodynamometer or manual palpation to determine contraction intensity is limited and of no clinical value. Intensity can be measured more precisely by an intrauterine pressure catheter. This device is placed transcervically inside the uterine cavity after membrane rupture and above the fetal presenting part. The Montevideo Unit attempts to measure objectively the intensity of the contraction. It is calculated by the average strength of contractions in millimeters of mercury multiplied by the number of contractions in 10 minutes. During the active phase of labor, 200–250 Montevideo Units are considered normal. Since an internal catheter is not routinely used in clinical practice, the ability to measure intensity of uterine contractions is limited. Frequency: Laboring patients in the active phase usually contract 3–5 times in 10 minutes. The presence of more than 5 contractions in 10 minutes for a period of 20 minutes is abnormal and is defined as tachysystole. When an alteration in the fetal heart rate accompanies tachysystole it is called hyperstimulation. Duration: The sensitivity to detect the uterine contractions varies with different methods. The highest sensitivity is observed with internal catheters followed by palpation and, finally, patient perception. External tocodynamometer determinations are biased by the sensitivity of the device as well as maternal body habit. Since the progression of labor and fetal descent are determined in part by the relationship of the fetal presenting part and the bony pelvis, the obstetrician must become familiar with the evaluation of the pelvic dimensions, which is traditionally determined by a pelvimeter (Fig. 11.2). Overall, four different shapes of female bony pelvis have been described. Two of them with favorable characteristics for vaginal delivery (gynecoid, anthropoid), and two (android, platypelloid) more frequently associated with cephalopelvic disproportion (CPD). The bony pelvis (Fig. 11.3) is composed of the sacrum, ilium, ischium, and pubis. The pelvic brim separates the false (greater) pelvis from the true (lesser) pelvis. The true pelvis is further divided into three sections: 1) the pelvic inlet, 2) midpelvis, and 3) pelvic outlet. The following are the measurable parts of the pelvic inlet. Diagonal conjugate: This is the distance from the sacral promontory to the inferior margin of the symphysis pubis. This measure can be obtained by vaginal examination. Fig. 11.2 A Martin pelvimeter. Fig. 11.3 Anatomyof the bony pelvis, anterior view. True or obstetric conjugate: This is the distance from the sacral promontory to the superior margin of the symphysis pubis. It is the shortest diameter of the pelvic inlet. Values below 10 cm are frequently associated with CPD. Although this measure cannot be obtained by vaginal examination, it can be calculated by subtracting 2 cm from the diagonal conjugate. The interspinous diameter: This is the distance between the ischial spines. It is the shortest diameter and measures below 10 cm are associated with CPD. Clinical examination allows evaluation of the pubic angle, prominence of the coccyx, and intertuberous diameter of the pelvic outlet. Fetal characteristics are of utmost importance in the progression of labor. Important parameters include fetal size, lie, presentation, attitude, position, and station. Fetal size: The impact of this measure in the progression of labor is relative to the maternal pelvis. However, macrosomic infants (>4500 g) need to be delivered by cesarean section significantly more often than normal birth weight babies. Lie: This term refers to the relation between the fetal and maternal longitudinal axis. It can be longitudinal, transverse, or oblique. Longitudinal lie is required to achieve a successful vaginal delivery. Presentation:
Labor Physiology
Mechanics of Labor
Contractions
The Pelvis
Pelvic Inlet

Midpelvis
Pelvic Outlet
The Fetus
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


