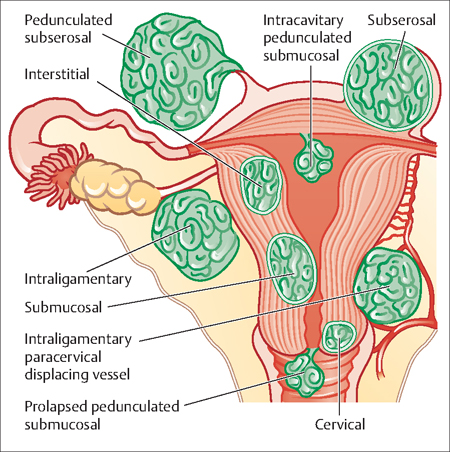
49 Uterine Leiomyomas Jon Ivar Einarsson Uterine leiomyomas, more commonly referred to as uterine fibroids, are benign tumors that arise from the myometrium of the uterus. The uterus is mostly composed of smooth muscle cells, designed to expand with the growing pregnancy and to help with vaginal delivery by contracting forcefully at the end of gestatation. Uterine fibroids can form underneath the endometrium (submucosal), in the myometrium (intramural), or underneath the uterine serosa (subserosal) (Fig. 49.1). Why fibroids are formed is not well understood. There are some genetic abnormalities in the smooth muscle cells that increase the risk for developing fibroids, and they seem to be under hormonal control, although the precise mechanism of this is not fully understood either. Fig. 49.1 Various subtypes of uterine fibroids based on location. Reproduced courtesy of Dr William J Mann Uterine fibroids are very common and are found in 40– 60% of reproductive age women. When examining surgically removed uteri from women of all ages, up to 80% of them are found to have some fibroids present. Some of the factors that influence the development of uterine fibroids are listed in Table 49.1. African-American women have higher risk for developing uterine fibroids than Caucasian women. Other risk factors for developing uterine fibroids include nulliparity (never carried a pregnancy beyond 20 weeks’ gestation), obesity, alcohol consumption, and genetic predisposition. It has also been proposed that high consumption of red meat and ham could increase the risk of fibroids, while consumption of fruit and vegetables could decrease the risk for fibroids; however, this has not been conclusively proven. Consistent use of birth control pills may lower the risk for developing uterine fibroids, although some studies show contrary findings.
Etiology
Epidemiology
| Increased risk |
| 40 years or older |
| African-American race |
| Family history of uterine fibroid tumors |
| Nulliparity |
| Obesity |
| Decreased risk |
| More than five pregnancies |
| Postmenopausal status |
| Prolonged use of oral contraceptives |
| Smoking |
| Use of depot medroxyprogesterone acetate (Depo-Provera) |
Symptoms
Uterine fibroids can cause abnormal uterine bleeding, pelvic pressure, and can have a negative effect on fertility. In general, fibroids that press on and distort the endometrium can cause abnormal bleeding. This includes submucosal fibroids and large intramural fibroids. When the fibroids grow larger, the uterus expands and puts pressure on adjacent organs, such as the rectum and the urinary bladder. This can lead to a feeling of fullness, constipation, and frequent urination. In extreme cases the uterus can be the size of a full-term pregnancy, reaching all the way up to the liver and diaphragm. Fibroids usually do not cause extreme pain; however, sometimes a fibroid might lose its blood supply due to rapid growth. This causes the fibroid to die (degenerate), which can cause severe pain. The pain will usually get better over a period of few days, but sometimes requires a surgical intervention. Fibroids that press on the endometrium probably decrease fertility, since this can interfere with the implantation of the embryo. Currently, no well-designed randomized clinical trials evaluating the effects of fibroids on fertility have been published. However, based on the best available evidence, it seems that removing uterine fibroids that distort the uterine cavity improves fertility in such women.
Diagnosis
Large fibroids can usually be identified during a regular abdominal exam or a pelvic exam. Ultrasonography can identify most fibroids and is easily performed in a doctor’s office. The addition of saline infusion sonohysterography can help to identify fibroids that are inside the uterine cavity. Office hysteroscopy is also an excellent tool to detect uterine fibroids inside the uterine cavity. Magnetic resonance imaging (MRI) gives very accurate information about the exact location and size of the fibroids. It is a useful tool to determine appropriate treatment options, such as removal of the uterine fibroids (myomectomy), embolization or focused ultrasound (see below), or a hysterectomy. MRI can also be helpful in determining if there is something else in the uterus that is causing the symptoms, such as adenomyosis or a leiomyosarcoma (cancer of the uterine muscle). It is, however, the most expensive diagnostic option and should be used selectively.
Treatment for Uterine Fibroids
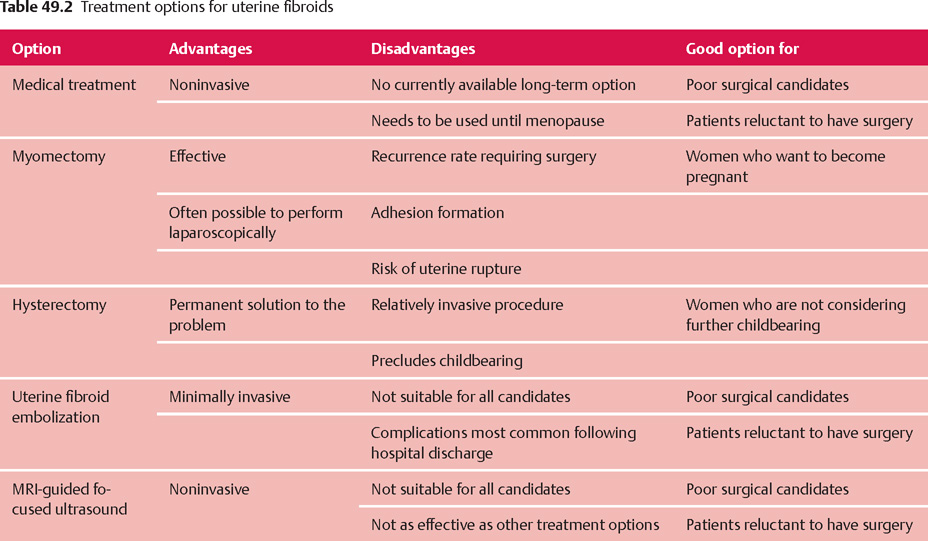
It is important to note that since fibroids are not cancerous, no treatment at all is probably the best option for women who are asymptomatic. The traditional treatment for uterine fibroids involves either removing the fibroids or the uterus via a laparotomy incision. Hysterectomy has usually been recommended for women who are not planning to have any more children, since there is a 15–20% risk that the symptoms will not improve following a myomectomy, thereby requiring additional surgery. However, some women may want to conserve their uterus even though they are not planning a future pregnancy. It is important to respect their wishes as long as they fully understand the risks and benefits associated with their decision. In addition to performing a hysterectomy or a myomectomy via a laparotomy incision, there are a number of minimally invasive and noninvasive options currently available, or in development, for this condition. Some of these surgical and nonsurgical options are discussed below (Table 49.2).
Medical Treatment
Gonadotropin-Releasing Hormone Agonists
The growth of uterine fibroids seems to be influenced by estrogen and progesterone. By modulating the effects of these hormones it is possible to significantly decrease the size of the fibroids. Gonadotropin-releasing hormone (GnRH) is normally produced in the hypothalamus and controls the ovarian production of estrogen and progesterone by influencing pituitary production of luteinizing hormone and follicle-stimulating hormone.
When a synthetic version of GnRH (GnRH agonist) is administered to a woman, there is an inital 2-week period of stimulation of hormone production, but then the system becomes oversaturated and the production of estrogen and progesterone shuts down temporarily. GnRH agonists are usually injected into muscle in long-acting formulations that have an effect for 1 or 3 months. They can also be administered daily using a nasal spray. In 3 months, GnRH agonists can shrink uterine size by one-third and the fibroid size by half. In addition, vaginal bleeding usually stops completely. Symptom relief from pressure or bleeding is therefore common. Unfortunately, GnRH agonists have significant side effects associated with hypoestrogenism, such as night sweats, hot flushes, irritability, vaginal dryness, and difficulty sleeping. In addition, long-term use is associated with significant bone loss (estrogen stimulates bone formation). Because of this, use GnRH agonists for longer than 6 months is not recommended. It is possible to reduce the side effects of the GnRH therapy by using a very low dose of estrogen or progesterone (add-back therapy). It is generally recommended to wait at least 4 weeks before starting the add-back therapy, in order to get a maximum effects on the fibroids.
Because GnRH agonist therapy can only be used for a short period and because the effects are quickly reversed, GnRH agonist therapy is mostly used to reduce the size of uterine fibroids before surgery. This facilitates the removal of the uterus or fibroids at the time of surgery. The maximal effect on uterine size is reached at 3 months, and therefore it is not necessary to treat women longer preoperatively.
Selective Progesterone Receptor Modulators
An intense search is in progress for a suitable long-term medical treatment for fibroids. One promising option seems to be medications called selective progesterone receptor modulators (SPRMs). These medications interact with cell receptors that respond to progesterone and change the effect that progesterone has on cells. One of these, called Mifepristone, has been found to be effective in reducing the size and symptoms of fibroids. However, the effects of long-term use are unknown and Mifepristone has been associated with an increased risk for endometrial hyperplasia. Another SPRM that shows promise is Asoprisnil. Early studies indicate that this medication is effective in decreasing symptoms and uterine size with no effect on endometrial function (Evidence Box 49.1). Time will tell whether this type of medication may be generally adopted, but early results are encouraging.
Birth Control Pills
Birth control pills do not seem to be very helpful to treat symptoms associated with uterine fibroids; however, they are effective in treating abnormal bleeding due to problems with ovulation and may decrease the growth rate of uterine fibroids. Possibly, the abnormal bleeding experienced might not be due to the fibroids, and therefore a 3 month trial of birth control pills is appropriate in selected cases.
Hormonal Intrauterine Device
The progesterone intrauterine device (IUD) marketed as Mirena might be effective in reducing abnormal uterine bleeding associated with fibroids; however, the size and growth of the uterine fibroids are probably not afected.
Surgical Treatment
Myomectomy should be the surgical option of choice in women who want retain their fertility. Other options such as uterine artery embolization, uterine artery occlusion, cryomyolysis, and focused ultrasound are usually not recommended for women who want to have more children. There are nevertheless some women who have become pregnant after these procedures and successfully carried their babies to term without complications. Most of these women became pregnant following uterine artery embolization. The number of complications associated with such pregnancies was significantly greater than in women who did not have these procedures. This may in part be explained by other, underlying health problems which might have increased the risk for pregnancy complications in these women. Nevertheless, women who want to become pregnant in the future should choose to have either an abdominal or a laparoscopic myomectomy.
Myomectomy
Myomectomy, or removal of uterine fibroids, is commonly performed in women who want to retain their fertility. It depends largely on the surgeon’s skill and experience as to which cases can be performed laparoscopically rather than via laparotomy. In general, cases where intramural fibroids larger than 10 cm across and more than three fibroids are removed at the time of surgery are associated with a higher complication rate. Fibroids that are located in the broad ligament or in the cervix can also be challenging to remove laparoscopically.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


