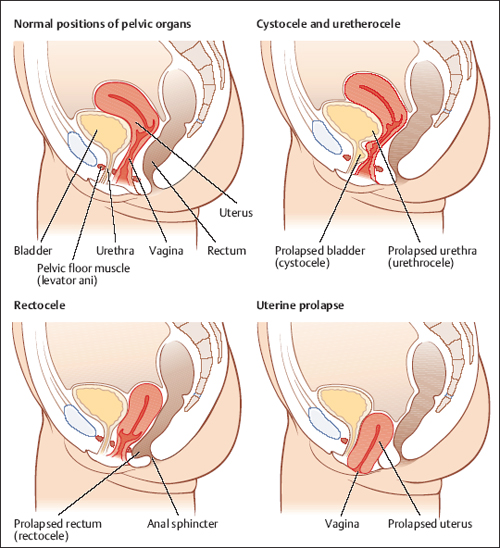
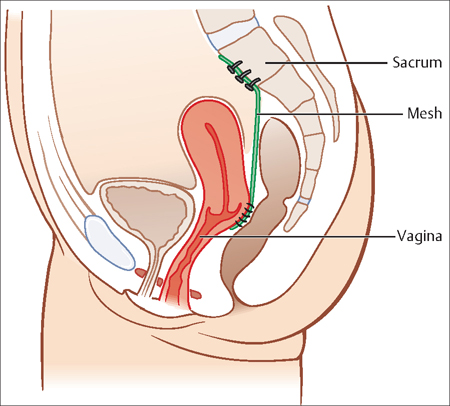
35 Pelvic Relaxation, Urinary Incontinence, and Urinary Tract Infection Jon I. Einarsson Pelvic relaxation or pelvic organ prolapse is a common condition, with a recent study finding the prevalence of stage 2 and greater pelvic organ prolapse to be 37% in a population of 1004 women seeking care at a gynecologic clinic. While some of these women are asymptomatic, genital prolapse remains one of the most common reasons for gynecologic surgery in women after the fertile period. Pelvic organ prolapse is often divided into three main subtypes, depending on where the prolapse is located (Fig. 35.1). In anterior prolapse (cystocele), the urinary bladder protrudes into the vagina. In posterior prolapse (rectocele), the rectum and/or the rectosigmoid protrudes into the vagina. Apical prolapse occurs when the cervix or the vaginal apex (following a hysterectomy) falls down through the vagina. Anterior and posterior prolapse are usually defects in the endopelvic fascia, which is a thick layer of connective tissue in the vagina, that is, the muscularis layer of the vaginal wall. This connective tissue can become detached from the normal attachments to the pelvic sidewall and/or become weakened or torn during childbirth or through wear and tear such as with chronic cough or constipation. Apical prolapse is more commonly associated with detachment or tearing of the uterosacral ligaments and the cardinal ligaments that connect to the pericervical ring to maintain the vaginal apex in a normal anatomic position. Pelvic organ prolapse causes pelvic pressure, pain, painful intercourse and significantly impacts the quality of life of those who sufer from it. A cystocele can cause frequent urination or urinary retention, and a rectocele can cause difficulty in emptying the rectum during bowel movements. Several etiologic factors that contribute to pelvic organ prolapse have been identified such as higher age, increased parity, obesity, and heritability.Recent evidence also suggests that women with pelvic organ prolapse have smaller amounts of collagen in the fibrous connective tissue of the endopelvic fascia. Diagnosis is made during a detailed pelvic exam. It is important to distinguish between prolapse in different vaginal compartments, since surgical treatment varies. A standardized system to evaluate and report pelvic organ prolapse, called the POP-Q system, is widely used in research and clinical practice. Some consider this to be too complex and prefer a simpler system, such as the Baden— Walken halfway system. In this system, 1st degree prolapse extends halfway to the introitus, 2nd degree prolapse extends to the introitus, 3rd degree prolapse extends halfway outside the introitus and 4th degree prolapse means that there is complete eversion of the pelvic organs (procidentia). Fig. 35.1 Anatomy of the most common types of pelvic organ prolapse. It is important to point out that asymptomatic pelvic organ prolapse usually does not require any therapy. Since conservative measures such as Kegel exercises or physical therapy do not seem to be effective, the main therapeutic option for symptomatic pelvic organ prolapse is reconstructive surgery, where defects in the endopelvic fascia are identified and repaired. While these surgical therapies can be effective, relapse rates of up to 50–60% have been reported. In order to reduce relapse rates, synthetic polypropylene mesh has been used to improve long-term success. While effective, synthetic mesh is costly and can cause erosions and, rarely, pelvic infections. The anterior and posterior compartment are usually repaired by re-approximating the endopelvic fascia with or without a mesh overlay. The “gold standard” treatment for apical prolapse is abdominal sacrocolpopexy with mesh (Fig. 35.2). Less invasive vaginal approaches such as the sacrospinous ligament fixation are especially applicable to older or less active patients. Recently, laparoscopic apical repairs have become more commonplace, thereby combining long-term durability and low morbidity. These are especially applicable to younger active women, since sacrocolpopexy is associated with a lower rate of dyspareunia than the vaginal repairs. Fig. 35.2 Sacrocolpopexy involves attaching the vaginal apex to the promontory of the sacrum. Urinary incontinence, or involuntary leakage of urine, affects about 25% of premenopausal women and 40% of postmenopausal women. The two most common types of urinary incontinence are stress incontinence and urge incontinence. Women who leak urine during coughing, sneezing, laughing, or lifting are considered to have stress urinary incontinence, and women who leak urine immediately following a strong urge to urinate have urge incontience. Urge incontinence is also associated with frequent urination (more than 12 times during the day) and nocturia (urinating more than once at night). Some women have mixed urinary incontinence, with components of both stress and urge incontinence. Overflow incontinence is a rare type of urinary incontinence, where women do not have normal bladder sensation or are unable to adequately empty the bladder. This leads to frequent urination, urinary leakage, and frequent urinary tract infections because urine stays in the urinary bladder at all times. If the urethral sphincter is weak, this can result in a subtype of stress urinary incontinence called intrinsic sphincter deficiency. The more common type is caused by too much mobility of the urethra (urethral hypermobility). The urethra is supported by connective tissue that can be weakened during childbirth, due to genetic defects in collagen or other connective tissue building blocks, or due to chronic cough or constipation. When the support of the urethra is weak or soft, the urethra sinks into the weakened connective tissue with increased intra-abdominal pressure, such as during cough or exercise. The pressure inside the bladder then becomes more than the pressure in the urethra leading to leakage of urine. This is similar to trying to stop a flow of water through a rubber hose by stepping on it. If the rubber hose is lying on soft grass, it is difficult to stop the flow of water by stepping on the hose, since the hose sinks into the grass and mud beneath it. However, if the hose is sitting on a hard surface, such as a sidewalk, it is much easier to stop the flow of water. The causes of urge incontinence are more complex and often no specific cause is found. The most common cause is overactivity of the detrusor muscle of the bladder. The detrusor muscle is designed to be relaxed during bladder filling and only contract during bladder emptying. However, for a variety of reasons that are not fully understood, the bladder muscle sometimes becomes over-active, which leads to a strong urge to urinate. If the muscle contractions are very strong, this can lead to a sudden leakage of urine. Sometimes triggers can cause this, such as the sound of running water, but this may be completely unprovoked. The contractions of the bladder muscle are controlled by the autonomic nervous system. Therefore, women who have sustained an injury to the spine or have neurologic disorders such as multiple sclerosis and diabetes often have symptoms of urge incontinence. A detailed history is the first step in diagnosing urinary incontinence, inquiring about duration of symptoms, medications, fluid intake, when the leaking occurs and how much this afects quality of life. A urinary diary can be helpful both for the patient and the physician. The patient notes freqency and amount of urination as well as frequency and amount of fluid intake. She will also be asked to note any urine leakage, if there was a strong sense of urgency prior to the leak and what she was doing when it happened. A simple, validated three-item questionnaire can also be useful to discern between urge and stress incontinence in clinical practice (Fig. 35.3). Simple urodynamics can be performed in the doctor’s office with minimal equipment. The patient first produces a urine sample to check for an infection. The post-void residual can then be measured by using ultrasonography or by inserting a narrow catheter into the bladder. Normally, the bladder should empty completely during urination, but a post-void residual greater than 100 mL is generally considered abnormal.
Pelvic Relaxation
Incidence
Subtypes and Anatomy
Symptoms
Etiology
Diagnosis
Treatment
Urinary Incontinence
Incidence and Subtypes
Pathogenesis
Diagnosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


