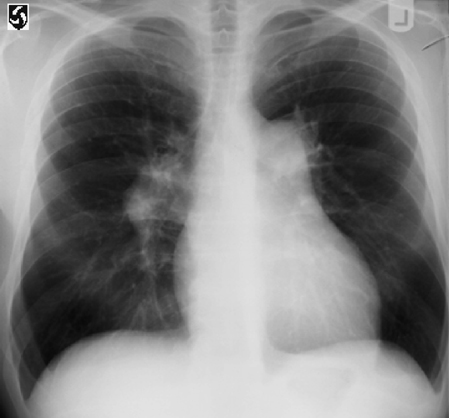
21 Hypertension in Pregnancy E. Albert Reece Hypertension is a complicating feature of 6–8% of pregnancies. It causes some of the most serious complications for both the fetus and the mother during pregnancy. Fetal complications include severe growth restriction and stillbirth. In addition, hypertensive disorders account for nearly 15% of maternal deaths in the United States, ranking second only to embolism as a leading cause of maternal mortility. Other complications for the mother can affect heart (Fig. 21.1), kidney, liver, and central nervous system functions. For these reasons, it is critical to accurately diagnose the type of hypertension that the patient has and to prescribe an appropriate therapeutic intervention. Hypertension in pregnancy is not a single entity. Rather, it is classifed into four main categories, as recommended by the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy: This terminology is preferred over the older but widely used term, pregnancy-induced hypertension (or PIH), because it is more accurate. Chronic hypertension: This is defined as a blood pressure (BP) greater than 140/90 mmHg that either predates pregnancy or develops before 20 weeks’ gestation. When hypertension is first identified during a woman’s pregnancy and she is at less than 20 weeks’ gestation, BP elevations usually represent chronic hypertension. Pre-eclampsia: This condition—which occurs in approximately 5% of all pregnancies, 10% of first pregnancies, and 20–25% of women with a history of chronic hypertension—is pregnancy-induced hypertension in association with proteinuria or edema, or both. Virtually any organ system may be afected. Pre-eclampsia superimposed on chronic hypertension: Pregnant women with pre-existing chronic hypertension may develop pre-eclampsia. Superimposed pre-eclampsia is suspected when proteinuria develops or increases suddenly; when previously controlled hypertension exhibits a sudden increase; or when the patient develops thrombocytopenia or elevated liver enzyme levels. Women with pre-eclampsia superimposed on chronic hypertension have a significantly poorer prognosis than women with either condition alone. Fig. 21.1 A radiograph of a patient with an enlarged heart due to chronic hypertension Gestational hypertension: This condition is pregnancy-induced hypertension in isolation; it may refect a familial predisposition to chronic hypertension, or it may be an early manifestation of pre-eclampsia. Pregnancy-induced hypertension, which develops after 20 weeks’ gestation, complicates 5–10% of pregnancies (see Prevalence and Epidemiology). Sometimes, determining whether hypertension identified during pregnancy is due to chronic hypertension or to pre-eclampsia is a challenge. Clinical characteristics, such as history, physical examination, and certain laboratory examinations, are used to help clarify the diagnosis. Chronic hypertension is diagnosed if there is a persistent elevation in BP to at least 140/90 mmHg on two occasions more than 24 hours apart prior to conception, prior to 20 weeks of gestation, or beyond 12 weeks postpartum. Other factors that may suggest the presence of chronic hypertension include: Chronic hypertension in pregnancy may be subclassifed into mild hypertension (diastolic [d] BP ≥90 to <110 mmHg or systolic [s] BP ≥140 to <180 mmHg) or severe hypertension (dBP ≥110 mmHg to or sBP ≥180 mmHg). For the purpose of clinical management, chronic hypertension in pregnancy may be divided into a low-risk group (hypertension with no organ damage or association with other comorbidities) or a high-risk group (hypertension with organ damage and associated comorbidities). Table 21.1 lists some of the major complications of chronic hypertension for both the mother and fetus.
Definitions
Diagnosis
Chronic Hypertension
| Mother |
| Pregnancy aggravated hypertension |
| Superimposed preeclampsia |
| Placental abruption |
| Fetus |
| Prematurity |
| Placental insufficiency |
| Intrauterine growth restriction |
| Placental abruption |
Pre-eclampsia-Eclampsia
(See Chapter 16.)
Pre-eclampsia Superimposed on Chronic Hypertension
Chronic hypertension may be complicated by superimposed pre-eclampsia (or eclampsia), which is diagnosed when there is an exacerbation of hypertension and the development of proteinurea that was not present earlier in the pregnancy. Conditions for the diagnosis of superimposed pre-eclampsia on chronic hypertension are detailed in Chapter 16.
Gestational Hypertension
Gestational hypertension is defined as dBP ≥90 mmHg or sBP ≥140 mmHg (without proteinurea) measured on two occasions at least 6 hours apart and no more than 7 days apart after 20 weeks of gestation. It is usually a mild form of hypertension, late in onset, often occurs close to term, and occurs intrapartum or within 24 hours of delivery. It often resolves within 10 days of the postpartum period without treatment.
Severe gestational hypertension is defined as a sustained sBP ≥160 mmHg and/or a dBP ≥110 mmHg measured at least 6 hours apart with no proteinurea. Women with severe gestational hypertension have higher maternal and perinatal morbidities that those with mild gestational hypertension. However, women with mild gestational hypertension often progress to severe gestational hypertension and pre-eclampsia if not treated.
The rate of progression from severe hypertension to pre-eclampsia is dependent on the gestational age at the time of diagnosis; the rate reaches 50% when gestational hypertension develops before 30 weeks of gestation.
Prevalence and Epidemiology
Chronic hypertension occurs in up to 22% of women of childbearing age, with the prevalence varying according to age, race, and body mass index. Chronic hypertension complicates 1–5% of pregnancies. In the United States, for example, there are at least 120 000 pregnant women with chronic hypertension (3% of 4 million pregnancies) per year, a rate expected to increase with the obesity epidemic and as age at childbearing increases in the developed world (see below). Pre-eclampsia complicates about 5% of all pregnancies, 10% of first pregnancies, and at least 20% of pregnancies in women with a history of chronic hypertension.
Race
Black women have higher rates of pre-eclampsia complicating their pregnancies compared with other racial groups, mainly because they have a greater prevalence of underlying chronic hypertension. A study in the US found that among women aged 30–39 years, chronic hypertension is present in 22.3% of Blacks, 4.6% of Whites, and 6.2% of Hispanics, who generally have BP levels that are the same as or lower than those of non-Hispanic White women.
Age
Pre-eclampsia is more common at the extremes of maternal age (<18 years or >35 years). The increased prevalence of chronic hypertension in women older than 35 years can explain the increased frequency of pre-eclampsia among older gravidas.
Etiology and Pathophysiology
Chronic hypertension may be either essential (90%) of cases or secondary to some identifable underlying disorder, such as renal disease, endocrine disorders, or vascular problems (Table 21.2).
About 20–25% of women with chronic hypertension develop pre-eclampsia during pregnancy. However, the exact cause of pre-eclampsia is unknown.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


