Orthopedics
Jaime R. Denning
The orthopedic or musculoskeletal examination is a significant part of neonatal evaluation. Normal variations in contour, size, relationships, and range of motion of joints are influenced by genetic factors and by position in utero. These normal variations must be distinguished from congenital anomalies and traumatic lesions. The basic principle, that the earlier appropriate treatment is started, the better the correction, makes it incumbent on those caring for the neonate to make an early diagnosis and obtain appropriate consultation promptly.
In current practice, musculoskeletal abnormalities may be detected prenatally. Using ultrasound, conditions such as skeletal dysplasia, spinal malformations, limb length discrepancy, and clubfoot deformities can be detected with some accuracy (1,2,3,4). The neonatal examination is vital to the confirmation of such anomalies and to the completion of any prenatal counseling rendered for such problems.
▪ PHYSICAL EXAMINATION
The clinician examines the musculoskeletal system first by inspection, looking for abnormalities in contour, size, and position and observing the spontaneous and reflex movements of the infant, and second by palpation and manipulation to determine whether there are abnormalities of passive motion. This is followed by stimulation, where indicated, so that active motion can be noted. All observations include comparisons between opposite extremities. A routine for examining a newborn should be developed so that each examination will be complete. This routine may vary among physicians, but each part of the musculoskeletal system should be examined systematically.
Head and Neck
The neck is examined passively for rotation, lateral flexion, anterior flexion, and extension. Rotation of 80 degrees and lateral flexion of 40 degrees should be present in a full-term infant. Both these motions are normally symmetric to the right and left. Extension and flexion are difficult to measure, but in flexion, the chin should touch or nearly touch the chest wall. Extension should be at least 45 degrees from neutral. When rotation or lateral flexion is asymmetric or when motion is limited, radiographs of the neck should be made.
Upper Extremities
The clavicle and shoulder girdle, including the scapula and proximal humerus, elbow, forearm, and hand, are inspected and palpated, with any anomalies in contour, size, and postural attitudes noted. Range of motion of the shoulder girdle is evaluated. Normal flexion and abduction of the shoulder are 175 to 180 degrees. Extension, internal rotation, and external rotation of the shoulder should be at least 25 degrees, 80 degrees, and 45 degrees, respectively.
The elbow is inspected next, and its motion is evaluated. Normally, the newborn’s elbow lacks 10 to 15 degrees from going to full extension and flexes 145 degrees. The forearm should pronate and supinate at least 80 degrees. Limitation of these two motions can be missed easily. Supination and pronation are tested by holding the humerus at the side of the trunk with the elbow held flexed 90 degrees with one hand while checking supination and pronation with the other. The wrist flexes 75 to 80 degrees and extends 65 to 75 degrees. The normally clenched fist of the newborn should have full passive extension of the thumb and all fingers. Active finger extension may be elicited, if necessary, by a pinprick to the palm. Extension should be to 0 degrees at the metacarpophalangeal joint, but active extension of the interphalangeal joint usually lacks 5 to 15 degrees from going to 0.
Spine
In the newborn, congenital anomalies of the spine are not readily detectable on physical examination; however, gross anomalies frequently can be recognized by inspection of the spine. Passive flexion and extension and lateral bending of the spine should show smooth contours. Lateral flexion may be slightly asymmetric, secondary to position in utero. A hairy tuft, cutaneous vascular pattern, or lipomatous mass may signal underlying axial anomalies.
Lower Extremities
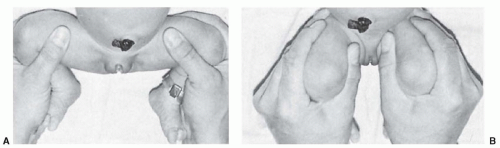
The lower extremities are observed for symmetry and variations in contour, position, and size. The hips of a newborn should flex 145 degrees and generally have flexion contractures, as shown by the Thomas test. This test is performed by fully flexing the infant’s hips and then extending the hip being tested while holding the opposite hip in flexion to lock the pelvis. The number of degrees that the extended thigh lacks from going to 0-degree extension is the degree of flexion contracture present in that hip. It is normal for the term newborn to have a 25- to 30-degree flexion contracture. The hip flexion contracture gradually diminishes during the first 12 weeks after birth but occasionally will be present longer than 3 months. When hip extension is asymmetric, the more extended hip may be unstable. The stability of the hip always must be evaluated by an Ortolani test (Fig. 48.1A) or the oppositely directed provocative Barlow test (Fig. 48.1B). When there is a difference in the extension of the hips or a positive Ortolani or Barlow test, additional evaluation of the hip by sonography is indicated. The timing of this imaging is discussed later in this chapter.
Internal and external rotation of the newborn’s hip should range between 40 and 80 degrees, abduction is between 45 and 75 degrees, and normal adduction is between 10 and 20 degrees. Any asymmetry of motion should be investigated to determine the cause.
Infants who were not in a frank breech fetal position generally will have a knee flexion contracture of 10 to 25 degrees, with additional ability to flex to 120 to 145 degrees. In those positioned in frank breech, the knees usually will hyperextend 10 to 15 degrees and have limitation of flexion.
Examination of the ankles and feet includes observation of resting positions and range of active motion, stimulated by stroking the sole and dorsal, medial, and lateral sides of the foot. The range of passive motion of the ankle in both dorsiflexion and plantar flexion varies depending on the fetal position. Dorsiflexion to above neutral should always be present. Plantar flexion of less than 10 degrees below neutral generally is abnormal. Abduction and adduction of the forefoot is at least 10 to 15 degrees, and the hindfoot has 5 to 10 degrees or more of motion in both varus and valgus.
▪ MUSCULOSKELETAL ANOMALIES
It is not within the scope of this text to discuss all the congenital and acquired abnormalities of the musculoskeletal system seen in the neonate; this chapter does, however, cover most of the more common abnormalities.
Neck
Klippel-Feil syndrome is a defect in segmentation of the cervical vertebrae (5). There is both a decrease in the number of vertebrae and a fusion of two or more vertebrae. The neck appears shorter than normal, and motion is limited in all directions. The limitation of motion depends on the number of fused segments and frequently is asymmetric in both rotation and lateral flexion. The asymmetric motion may simulate muscular torticollis, but radiographic examination of the neck can confirm the presence of the Klippel-Feil deformity. Treatment started early, done several times a day, and consisting of passive stretching of the neck to improve rotation, lateral bending, and flexion-extension may improve the range of motion of the neck. A careful search for associated anomalies should be performed as renal anomalies, hearing impairment, and cardiac defects are present in a significant number of patients with Klippel-Feil (6).
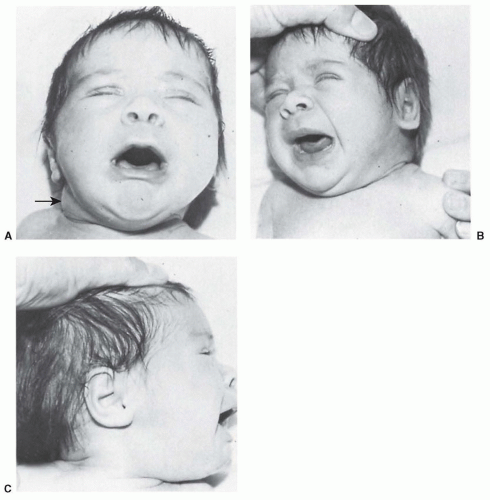
Torticollis of the neonate may be one of several types. The typical muscular torticollis (Fig. 48.2A) involves a mass from an intramuscular hematoma that appears in the sternocleidomastoideus at 2 weeks of age and gradually disappears during the next 8 to 10 weeks. This mass may go unnoticed and the torticollis unrecognized until there is facial asymmetry and limited motion of the neck. The physical findings of muscular torticollis are limited rotation of the neck toward the side of the lesion (Fig. 48.2B and C) and limited lateral flexion away from the lesion. In well-established, persistent torticollis, there is flattening of the maxillary and frontal bones on the side of the lesion and of the occiput on the opposite side. The asymmetry is not present in the newborn but may become apparent as early as 2 or 3 weeks and is progressive until the tightness is corrected. Torticollis associated with intrauterine deformation may be apparent at birth.
Initial treatment of muscular torticollis is by passive exercise and appropriate positioning of the infant in bed (7). The neck should be gently but firmly stretched four or five times each day toward the direction of limited rotation and lateral flexion. Sandbags or some similar objects may be used to position the baby’s head to prevent it from assuming the position that the tight muscle encourages.
There is a type of congenital torticollis that is associated with neither a mass in the sternocleidomastoideus nor cervical spine abnormalities. In these infants, there is a myostatic contracture of the sternocleidomastoideus, probably secondary to in utero position or compression. This type of torticollis often is associated with scoliosis and abductor contracture of one hip and adductor tightness of the opposite hip. The adducted hip may show acetabular dysplasia (Fig. 48.3). The abductor contracture may not be detectable until the normally present tightness of hip flexors has spontaneously diminished enough that the hip can be extended. Whereas this type of torticollis corrects with little or no treatment, the associated hip contractions require stretching. Rarely, the associated acetabular dysplasia progresses to dislocation. This association between torticollis and hip dysplasia should remind the clinician to look for one condition when the other is present (8).
Spine
Scoliosis
Congenital scoliosis is difficult to recognize at birth unless there is asymmetric movement, a cutaneous lesion (such as aplasia, dimple, dermal sinus tract, flat hemangioma, or hairy tuft), or a lipomatous mass. In the newborn infant, scoliosis is caused by an isolated defect in vertebral body formation or by failure of segmentation. There is little evidence that it is an inherited anomaly, except when it occurs as part of a genetically transmitted syndrome. Because of the cartilaginous nature of much of the spine at birth, only significant anomalies, such as hemivertebrae, can be diagnosed by plain x-ray. Ultrasound is a good alternative for evaluation of suspected cases when magnetic resonance imaging (MRI) is not indicated in the newborn (9,10). For the older infant with significant abnormalities, MRI evaluation is certainly indicated for determination of occult intraspinal pathology, including syringomyelia, diastematomyelia, and tethered cord (11). Spinal orthoses and casting are seldom are of long-term benefit, but these treatment modalities may be used to prolong time to surgery (12). Early referral to a spine specialist is recommended for congenital scoliosis. If a curve is progressive, spinal fusion will be needed and should be done before the curve becomes cosmetically or functionally significant (13). Fusion of a short segment, with or without excision of markedly abnormal bone segments, may be done as early as necessary. Congenital scoliosis is associated with a high incidence of cardiac and related genitourinary anomalies; therefore, the function and anatomy of the cardiovascular and genitourinary systems should be evaluated by MRI and ultrasonic techniques (14).
Myelomeningocele
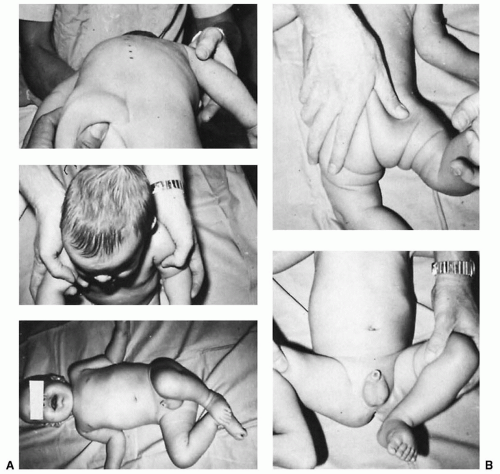
Diagnosis of a myelomeningocele generally poses little problem when there is a skin defect. Because the skin over myelomeningoceles is not always defective, any soft mass in or off the midline must be examined closely to determine its composition. Lipomata always have good skin coverage and tend to be off the midline.
The care of an infant born with myelomeningocele is complex and requires input from several specialties (see Chapter 47,
“Neurosurgery of the Newborn”). It is important to determine immediately after birth the level of involvement by inspection of the back, careful examination of the muscle function of the lower extremities, and radiographic examination before surgical closure.
“Neurosurgery of the Newborn”). It is important to determine immediately after birth the level of involvement by inspection of the back, careful examination of the muscle function of the lower extremities, and radiographic examination before surgical closure.
The most common abnormalities of the lower extremities associated with myelomeningocele are deformations of the feet, indicating lack of normal fetal muscle activity. Initial treatment of the deformed foot is with plaster cast correction, followed, if necessary, by surgical releases and transfer of muscle insertions to maintain the correction. These surgeries may be done at almost any age.
Gentle passive exercising and progressive splinting treat flexion or extension deformities of the knee. New splints need to be made frequently as the deformity improves.
Treatment of a dislocated hip in the patient with myelomeningocele is controversial. There is general agreement that in those children with intact hip musculature, the dislocated hip, as in an otherwise-normal newborn, reduces easily in flexion and abduction. For those lesions below L-2, hip abduction therapy helps in developing a more stable hip. The flexed, abducted, and externally rotated position achieved in a Pavlik harness should not be used when the lesion is above L-2 because this position may lead to development of contractures that prevent the hip from extending and adducting.
Infants with high lumbar or low thoracic myelomeningoceles have very high mortality and morbidity. The degree of disability correlates well with the level of defect, presence and degree of hydrocephalus, and presence of a bony kyphosis.
Upper Extremities
Duplication and Reduction
Supernumerary parts, absence or reduction anomalies of the extremities, and segmentation defects of the limb should offer no problem in diagnosis. These orthopedic anomalies seldom need immediate attention, but they should be seen early by the orthopedist to plan appropriate therapy and discuss prognosis with the family. This is true for anomalies of both the upper and lower extremities.
Syndactylism, or fusion of any portion of two or more digits, is a common anomaly that is transmitted through an autosomal dominant gene with varying expressivity. Surgical treatment should be within the 1st year, with timing dependent on the completeness of the syndactyly and the fingers involved. It is important to determine by radiography if there is a synostosis between fingers because this should be divided by 1 year of age. A delay in surgical separation in synostosis will result in a bowing of the longer finger due to differential growth.
Polydactyly is correctable by surgery, with timing dependent on the extent of duplication. When the duplication does not contain
bone or cartilage, it can be removed in infancy. When there is a question about function, surgical correction should be delayed until the degree of function present in each of the duplicated digits can be ascertained.
bone or cartilage, it can be removed in infancy. When there is a question about function, surgical correction should be delayed until the degree of function present in each of the duplicated digits can be ascertained.
Absence of the radius, formerly called radial clubhand, now termed congenital radial longitudinal deficiency is easily recognized (Fig. 48.4). The wrist and hand are deviated 90 degrees or more. Absence of the radius may be bilateral or unilateral, and the thumb may be present, absent, or hypoplastic. The condition is caused by damage to the apical ectoderm or deeper mesenchymal tissue of the limb bud. It is not genetically transmitted in the otherwisen-ormal child, but it is associated with several genetically transmitted syndromes and frequently is accompanied by aplastic anemia. Early treatment by corrective splints may be started, and there are many surgical approaches that should be tailored to each patient by his or her hand surgeon to improve function (17).
Congenital absence of the thumb occurs as an isolated anomaly or may be associated with a radial deficiency. When unilateral, little or no treatment is needed, but when the absence is bilateral, pollicization of the index finger of the dominant hand will improve function. When the thumb is rudimentary and nonfunctional, treatment is controversial.
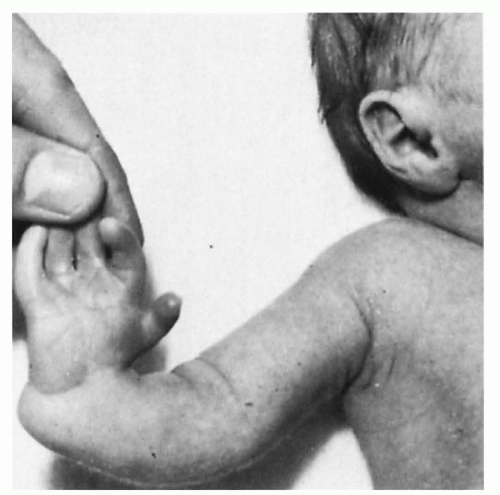
In the extremities, congenital constriction band (Streeter) syndrome is diagnosed at birth by the presence of defects in the soft tissue underlying the skin (that is usually intact). This entity, possibly more accurately called early amnion rupture sequence, has been
proposed as an etiologic factor in extremity, truncal, and facial abnormalities, including cleft lip/palate (18). In either the upper or lower extremity, a circumferential band can lead to neurovascular compromise of the distal part of the extremity (Fig. 48.5). The presentation is one of a visible constriction or, in more extreme cases, cyanosis or extreme edema in the portion of the extremity distal to the band. Surgical treatment to release the band or amputation in severely compromised extremities may be indicated at a relatively early age (19).
proposed as an etiologic factor in extremity, truncal, and facial abnormalities, including cleft lip/palate (18). In either the upper or lower extremity, a circumferential band can lead to neurovascular compromise of the distal part of the extremity (Fig. 48.5). The presentation is one of a visible constriction or, in more extreme cases, cyanosis or extreme edema in the portion of the extremity distal to the band. Surgical treatment to release the band or amputation in severely compromised extremities may be indicated at a relatively early age (19).
Shoulder Girdle
The Sprengel deformity of congenital elevated scapula is the most common congenital anomaly of the shoulder girdle. The deformity may be bilateral or unilateral, and usually it is associated with other abnormalities, such as Klippel-Feil, congenital anomalies of the upper thoracic vertebrae, or ribs. Asymmetry of the shoulders in unilateral involvement makes recognition easier. On palpation, the affected scapula is high and rotated outward so that its vertebral border lies superiorly and more horizontally than normal. Shoulder abduction and flexion usually, but not always, are limited. The early, conservative treatment is passive range of motion. Surgical correction, if necessary, generally improves appearance and function, with the overall improvement from surgery better in the younger child (20).
Two congenital malformations of the clavicle are congenital pseudoarthrosis and congenital (partial or complete) absence of the clavicle. The physical signs on palpation of congenital pseudoarthrosis are angulation of the clavicle and a painless, bulbar mass in the midclavicular area (Fig. 48.6). The shoulder girdle is hypermobile, with motion in the clavicle at the pseudoarthrosis. Early treatment is not needed before surgical grafting of the defect at 3 to 4 years of age. Because the need for any intervention is controversial, therapy should be individualized. Congenital pseudoarthrosis of the clavicle can be differentiated from perinatal fracture of the clavicle by abundant callus formation in the healing fracture within 2 to 3 weeks after birth.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree