Operative Hysteroscopy
Mindy S. Christianson
Kyle J. Tobler
Howard A. Zacur
DEFINITIONS
Hysteroscopy—Direct visual inspection of the cervical canal and uterine cavity through a rigid or flexible hysteroscope.
Index of refraction—The bending of light caused by the ratio of its velocity in room air to its velocity within an optical fiber.
Resectoscope—A specialized electrosurgical endoscope that consists of an inner and outer sheath equipped with a 30-degree telescope. The inner sheath has a common channel for the telescope fluid medium and electrode.
Uterine synechiae—Adhesions that form between the anterior and posterior walls of the uterus as a result of trauma or infection in a milieu of estrogen deprivation.
INTRODUCTION
Hysteroscopy is a term derived from the Greek words hystera, which means uterus, and skopeo, which means “to view.” In 1869, Pantaleoni successfully performed this procedure in a living human subject. He used a tube with an external light source to detect “vegetations within the uterine cavity.” No attempt was made at this time to distend the uterine cavity. During the past 145 years, developments in optics, fiberoptics, instruments, and distending media have resulted in new equipment and techniques that allow the gynecologic surgeon to diagnose and treat many intrauterine cavity disorders. Hysteroscopy is a standard part of the gynecologic surgeon’s armamentarium and the preferred minimally invasive choice for treatment of intrauterine pathology.
Abnormal vaginal bleeding may occur as the result of many different intrauterine cavity disorders. Dilating the endocervical canal and then blindly probing or curetting the uterine cavity to diagnose and treat these disorders would seem far less effective than performing a diagnostic and/or operative hysteroscopy. Critics have cautioned, however, about the risk of disseminating endometrial cells into the peritoneal cavity from the pressure of either gaseous or liquid distending medium during hysteroscopy. In 2000, reports by Zerbe and colleagues and Obermair and colleagues demonstrated that endometrial cancer cells could be found in peritoneal fluid following hysteroscopy with saline as distending medium in women with endometrial cancer. Whether to use hysteroscopy in evaluating abnormal bleeding in women at risk for endometrial cancer was questioned by the authors of these reports. A retrospective cohort analysis by Soucie and associates in 2012 linked a registry of women diagnosed with endometrial cancer with performance of hysteroscopy, staging of endometrial cancer, and death rates. This study concluded that hysteroscopy in women with endometrial cancer was not associated with causing a higher stage of disease. The authors concluded that hysteroscopy should continue to be used as a safe diagnostic tool for abnormal uterine bleeding.
With the emergence of minimally invasive gynecology surgery as a recognized advantage to patients, operative hysteroscopy has earned a special niche in this area. The advantages
of hysteroscopy as an accurate diagnostic technique are that it not only allows direct visual observation and accurate localization of pathology but also provides a means to sample the site most likely to yield positive results. Hysteroscopy generally is a low-risk technique that uses the endocervical canal, the natural passageway of the body, to gain entry into the intrauterine environment. Commonly performed procedures utilizing hysteroscopy include diagnostic hysteroscopy, tubal sterilization, polypectomy, myomectomy, and excision of uterine septa. Nonhysteroscopic techniques to treat intrauterine septa and adhesions are obsolete. Ablation or resection of the endometrium is considered an acceptable alternative to hysterectomy for the management of abnormal uterine bleeding. Submucous myomas no longer require hysterectomy because they can be satisfactorily managed conservatively by operative hysteroscopy. Cornual obstruction and interstitial tubal obstruction also are now managed hysteroscopically. Teaching operative hysteroscopy techniques is a key aspect of residency training curriculums and postgraduate seminars. However, as operative hysteroscopy case numbers have increased, the number of complications has also risen. Most of these complications are caused by operator error and inexperience.
of hysteroscopy as an accurate diagnostic technique are that it not only allows direct visual observation and accurate localization of pathology but also provides a means to sample the site most likely to yield positive results. Hysteroscopy generally is a low-risk technique that uses the endocervical canal, the natural passageway of the body, to gain entry into the intrauterine environment. Commonly performed procedures utilizing hysteroscopy include diagnostic hysteroscopy, tubal sterilization, polypectomy, myomectomy, and excision of uterine septa. Nonhysteroscopic techniques to treat intrauterine septa and adhesions are obsolete. Ablation or resection of the endometrium is considered an acceptable alternative to hysterectomy for the management of abnormal uterine bleeding. Submucous myomas no longer require hysterectomy because they can be satisfactorily managed conservatively by operative hysteroscopy. Cornual obstruction and interstitial tubal obstruction also are now managed hysteroscopically. Teaching operative hysteroscopy techniques is a key aspect of residency training curriculums and postgraduate seminars. However, as operative hysteroscopy case numbers have increased, the number of complications has also risen. Most of these complications are caused by operator error and inexperience.
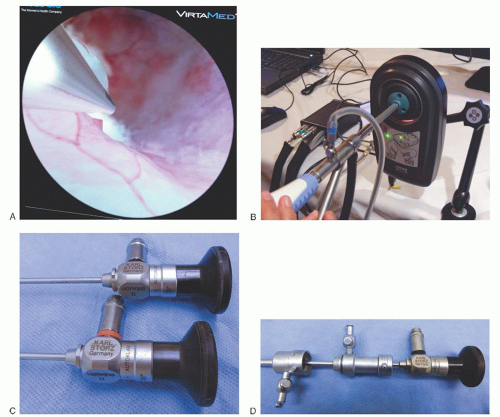
Learning how to perform an adequate hysteroscopy and then becoming competent to do hysteroscopic surgery are practice, skill-related techniques. Older methods of acquiring endoscopic skills focused on course attendance, preceptorship, and practice. During the late 1990s and continuing to the present, simulators have been developed to facilitate hand-eye coordination exercises. Several of the computer-based models with advanced interactive graphics provide sophisticated models for the student to shave myomas, ablate endometrium, and pass cannulas into tubal ostia (Fig. 18.1A, B).
However, the most basic skill levels a hysteroscopist must attain are the ability to insert the scope safely into the uterine cavity followed by satisfactory distension of the cavity to obtain clear visualization of that cavity. The preceding is not taught by simulation and must be learned in vivo. Without this skill set, hysteroscopy cannot be successfully performed.
However, the most basic skill levels a hysteroscopist must attain are the ability to insert the scope safely into the uterine cavity followed by satisfactory distension of the cavity to obtain clear visualization of that cavity. The preceding is not taught by simulation and must be learned in vivo. Without this skill set, hysteroscopy cannot be successfully performed.
INSTRUMENTATION
Hysteroscopes may be classified as rigid or flexible and possessing fixed or variable focus and be designated for either diagnostic or operative use. Scope diameter, lens offset, sheath diameter, ability to be used with a variety of distending media,
and ability to use either bipolar or monopolar cautery are key characteristics of the instrumentation.
and ability to use either bipolar or monopolar cautery are key characteristics of the instrumentation.
Viewing through the hysteroscopic telescope may still be done by using the naked eye, but is now almost always done by using a camera and video screen. As might be expected, the images obtained by the hysteroscope may vary depending upon the type of camera and video screen used with highdefinition systems providing the sharpest images (Fig. 18.2).
Telescopes
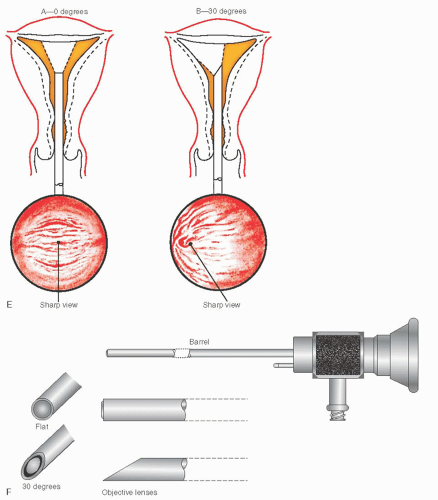
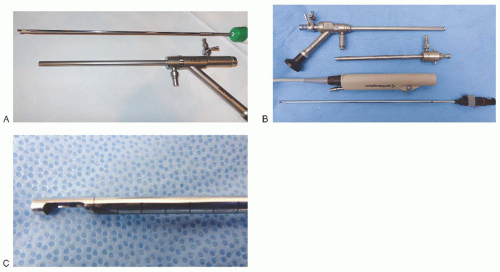
The telescope has three parts: the eyepiece, the barrel, and the objective lens (Fig. 18.1F). The 4-mm telescope (lens) gives the sharpest, clearest image in addition to a small outside diameter (Fig. 18.1C). The most desirable optics provide a large field that subtends an angle of approximately 105 degrees. However, 3-mm diameter telescopes, which have greatly improved optics, provide comparable views. These contemporary 3-mm diameter telescopes coupled to endoscopic video systems with zoom lenses are highly satisfactory for office hysteroscopy as well as for operative hysteroscopy. Telescopes are available in a variety of viewing angles with the 0-degree straight-on or a 30-degree fore-oblique view being the most common (Fig. 18.1E). Other viewing angles available include 12 degrees, 15 degrees, and 70 degrees. The major advantage of the 0-degree lens is that it allows the operator to see operative devices as a relatively distant panorama, whereas this view is lost when 30-degree lens is used. Surrounding the optics are numerous small-diameter incoherent fiberoptic bundles that provide intense cold illumination to the operative field.
Light Generators
The quality and power of light delivered to the telescope depend on the wattage and characteristics of the remote light generator and the type and structural integrity of the connecting fiberoptic light cable. Three general types of light generators are available: tungsten, metal halide, and xenon. The xenon white light is a powerful generator that provides high-quality color and intensity and is the most commonly used today.
Fiberoptic light cables must be intact to convey the optimal light from the generator to the telescope. Broken fibers can be easily identified by viewing the stretched-out cable against a dark background and looking for light emitting through the sides of the cable. The liquid cable conducts light effectively and provides superior light when combined with a xenon generator.
Diagnostic and Operative Sheaths
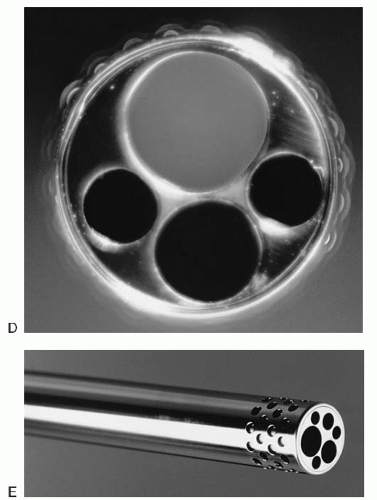
A diagnostic sheath is required to deliver the distending medium into the uterine cavity. The telescope fits into the sheath and is secured by means of a watertight seal that locks into place. The sheath is 4 to 5 mm in diameter, depending on the outer diameter of the telescope, with a 1-mm clearance between the inner wall and the telescope, through which either carbon dioxide (CO2) or liquid distending medium is transmitted (Fig. 18.1D). Medium instillation into the sheath is controlled by means of an external stopcock. Even the 5-mm instrument allows easy access through the narrow endocervical canal past the point of maximal constriction, the internal os. Therefore, diagnostic hysteroscopy usually can be performed without cervical canal dilatation. If the hysteroscope is inserted into the canal under direct vision, and if the axis of the cervical and uterine canal is carefully followed until the corpus is reached, there should be no risk of creating a false passage or perforation. Imprecise or loose coupling between the telescope and sheath will result in leakage of the medium at that interface.
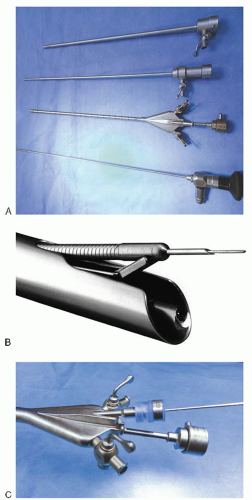
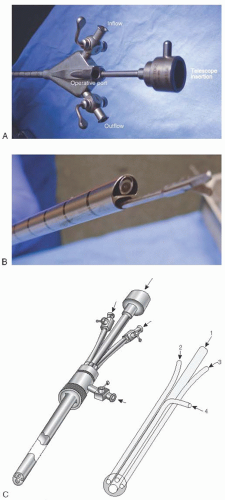
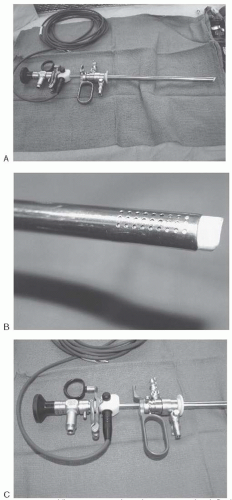
Operative sheaths have a larger diameter than do diagnostic sheaths, ranging in size from 7 to 10 mm and average 8 mm in diameter (Fig. 18.3). The operative sheath allows space for instillation of the medium, for the 3- to 4-mm telescope, and for the insertion of operating devices. The operating channel is sealed with a rubber nipple or gasket to prevent leakage of the distending medium (Fig. 18.3C). The standard operating sheath consists of a single common cavity shared by the medium, telescope, and operating tools. Disadvantages of this type of sheath are inability to flush the uterine cavity with the distending medium and difficulty manipulating the operative tools within the cavity. Hysteroscopes with isolated channels overcome the problems inherent to the common cavity sheath (Fig. 18.4). The dual operating channels permit flushing of the cavity and precise placement of operating accessories. A popular model today is the isolated-channel sheath consisting of a double-flushing sheath (Fig. 18.4D, E) that permits media instillation by way of the inner sheath and media return by way of the perforated outer sheath. The constant flow of the fluid medium in and out of the cavity creates a very clear operative field. The single isolated operating channel has a diameter sufficiently large (3 mm) to permit an entirely new generation of larger, sturdier operating tools to be used (Fig. 18.4). The new sheath combines the advantages of the resectoscope with the facility of the operating hysteroscope.
The resectoscope is a specialized electrosurgical (monopolar or bipolar) endoscope that consists of an inner sheath and outer sheath (Fig. 18.5A). The outer sheath is for fluid return as described above. The inner sheath has a common channel for the telescope, fluid medium, and electrode (Fig. 18.5B). The double-armed electrode is fitted to a trigger device that pushes the electrode out beyond the sheath and then pulls it back within the sheath (Fig. 18.5C). The operating tools consist of four basic electrodes: a cutting loop, ball, button, and angulated needle (Fig. 18.5D-G). Most resectoscopes are equipped with a 30-degree telescope. The lens is angled toward the electrode to permit a clear view of the near operative field. Vision of the electrode is lost when the electrode is fully extended outward. Most operating sheaths measure 8 mm or more in outer diameter, so dilatation is usually required for insertion. Contemporary small-diameter resectoscopes use a 3-mm telescope and a 7- to 7.5-mm sheath.
CAMERA
In most cases today, hysteroscopy employs the endoscopic microchip camera coupled directly to the telescope, with digital cameras and digital recorders. Endoscopic video camera lenses range in focal length from 25 to 38 mm. A 28- to 30-mm lens provides satisfactory magnification. The view with the coupled camera provides magnification comparable to that obtained during microsurgery. If a video recorder is available, a permanent record of the procedure can be recorded. A xenon light generator provides the best illumination for video techniques, although less expensive light sources may be satisfactory when coupled to newer cameras, which are highly light sensitive.
ACCESSORY INSTRUMENTS
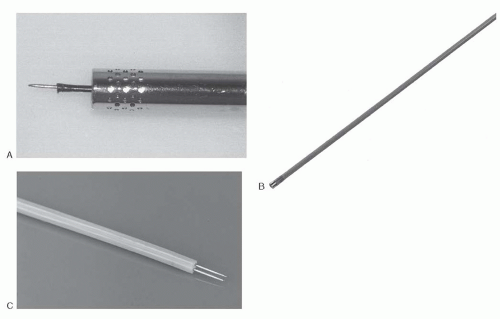
The standard accessories are the 7-F (i.e., 2.3-mm) alligator grasping forceps, biopsy forceps, and scissors. The small size of these semirigid instruments makes them particularly fragile, as excessive torque at the junction of the shaft and handle frequently leads to breakage. Flexible devices are less likely to fracture and are equally as facile compared with the semirigid variety. Development of the large isolatedchannel sheath has made the use of totally flexible 3-mm operating instruments feasible. The scissors and graspers are substantially heavier and much less prone to breakage (Fig. 18.6A-D).
A variety of monopolar and bipolar electrodes are also now available for operative hysteroscopy. Monopolar balls, needles, shaving loops (3 mm), and ridged (vaporizing) loops can be inserted through the large operating channel. Bipolar needles for myolysis, as well as bipolar ball and cutting loop electrodes, have been manufactured (Fig. 18.7), together with bipolar scissors and needles. The hysteroscopic sheath has an advantage over the resectoscopic sheath, allowing insertion of an aspirating cannula (2.3 or 3 mm), which permits the operator to selectively clear the field of bubbles and debris that cannot be removed by the way of the return second sheath. Nevertheless, the resectoscope is generally easier to use for the average gynecologist.
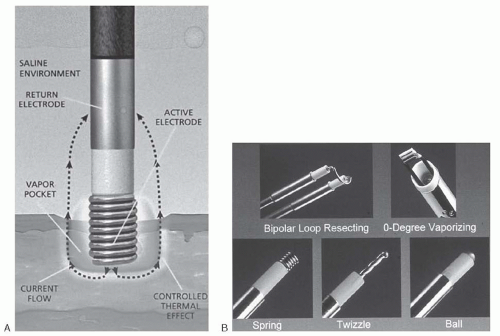
A complete bipolar system marketed under the trade name of Versapoint (Gynecare, Ethicon, Somerville, NJ) permits cutting and ablation via operative hysteroscopes or via a dedicated bipolar resectoscope. The mechanism for the bipolar current flow through the electrode is illustrated in Figure 18.8A. The electrodes measure 5-F diameter (i.e., 2 mm) and therefore can be accommodated by standard and isolated hysteroscopic channels (Fig. 18.8B). The biggest advantage of this bipolar technology is that saline may be used as the distending medium for the operative hysteroscopy. This obviates the risk of hyponatremia (see sections on media and complications). Hysteroscopic morcellators have also been developed as an alternative to the resectoscope in removing uterine submucosal myomas. Two such systems are TRUCLEAR hysteroscopic morcellator (Smith & Nephew, Andover, MA) and the MyoSure tissue removal system (Hologic, Bedford, MA) (Fig. 18.9A, B). Both systems use suction-based, mechanical energy, rotating tubular cutter systems rather than the highfrequency electrical energy used by resectoscopes. The benefits of these systems include the ability to use isotonic distension media such as normal saline and an improved visual field as resected “fibroid chips” are removed.
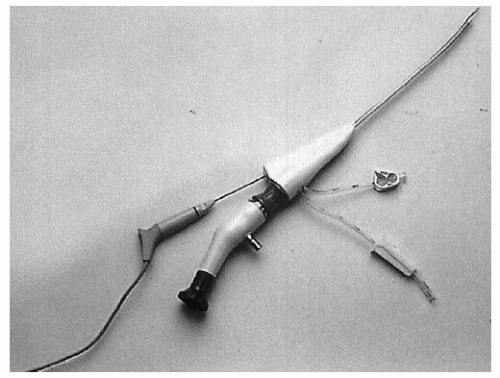
The Flexible Hysteroscope
The 4.8-mm-diameter fiberoptic hysteroscope consists of three sections: a soft flexible front section, a rigid rotating middle section, and a semirigid rear section. In 1990, Lin
and colleagues reported their experiences with this instrument in 153 procedures, including transcervical tubocornual recanalization, chorionic villus sampling, and retrieval of lost intrauterine devices (IUDs). The flexible hysteroscope has particular advantage in its ease of aligning the catheter for tubal canalization. Several manufacturers now produce fiberoptic (flexible hysteroscopes) (Fig. 18.10). Contemporary fiberoptic hysteroscopes are available with single-use, sterile sheaths that eliminate need to sterilize equipment between cases.
and colleagues reported their experiences with this instrument in 153 procedures, including transcervical tubocornual recanalization, chorionic villus sampling, and retrieval of lost intrauterine devices (IUDs). The flexible hysteroscope has particular advantage in its ease of aligning the catheter for tubal canalization. Several manufacturers now produce fiberoptic (flexible hysteroscopes) (Fig. 18.10). Contemporary fiberoptic hysteroscopes are available with single-use, sterile sheaths that eliminate need to sterilize equipment between cases.
DISTENDING MEDIA
Under normal circumstances, the uterine cavity is a potential space, with the anterior and posterior walls in close apposition. To achieve a panoramic view within the uterus, the walls must be separated. The thick muscle of the uterine wall requires a minimum pressure of 40 mm Hg to distend the cavity sufficiently to see with a hysteroscope. Because the endometrium is richly endowed with blood vessels, touching it with the sheath of the hysteroscope often produces bleeding. Although a variety of distending media can be used to attain the desired degree of distention, it usually requires pressures approximating 70 mm Hg, which at the same time propels the medium through the oviducts into the peritoneal cavity. Overdilatation of the cervix with a loosely applied hysteroscopic sheath results in leakage of the medium, suboptimal pressure, and poor expansion of the uterine cavity. In contrast, a tight application of the sheath maintains the medium within the cavity, keeps intrauterine pressure above mean arterial pressure, and maintains a clear operative field.
Media can be conveniently divided into gaseous or liquid. The latter may be further subdivided into high-viscosity and low-viscosity fluids.
GASEOUS MEDIA
Carbon Dioxide
CO2 is a colorless gas that is highly soluble when mixed with blood. It can be used to safely distend the uterus when instilled with a proper insufflation apparatus. CO2 is ideal for diagnostic hysteroscopy. The hysteroscopic insufflator (Fig. 18.11) delivers CO2 into the uterus at a flow rate measured in cubic centimeters per minute, in contrast to the laparoscopic insufflator, which allows CO2 to flow in at a rate of liters per minute. The laparoscopic insufflator is both unsuitable and unsafe for hysteroscopic insufflation. The rate of flow of CO2 into the uterus should never exceed 100 mL per minute, and pressure should be adjusted below 150 mm Hg. Before CO2 is infused, the hysteroscopic tubing and the hysteroscope must be purged of air. Additionally, the Trendelenburg position should be avoided.
When CO2 flow is excessive, bubbles appear and obscure the field. CO2 tends to flatten the endometrium, and this artifact can obscure pathology. When CO2 is improperly instilled, emboli form and can produce severe derangements in cardiovascular physiology. Advantages of CO2 as a distention medium include its neatness. It does not foul instruments, it does not mess up the office or operating room, and it allows entry evaluation of the endocervical canal. CO2 is therefore an excellent diagnostic medium. The disadvantage of CO2 is that it cannot be used for operative hysteroscopy due to risk of CO2 embolism.
LIQUID MEDIA
High Viscosity
Hyskon (32% dextran 70 in dextrose) is a colorless, viscid solution that is rarely used today for diagnostic and operative hysteroscopy. An advantage of Hyskon is its immiscibility with blood, which permits excellent visualization, even during active bleeding. A disadvantage of Hyskon is that dried residue tends to harden and clog hysteroscopic sheath channels. Two types of severe patient reactions unique to Hyskon have been reported: a syncratic anaphylactoid reaction and a bleeding diathesis. The hematologic reaction is caused by excessive vascular uptake of dextran, which allows a more general manifestation of its physiologic actions, including fibrinoplastic action, stearic exclusion, alteration of platelet adhesiveness, and interference with von Willebrand factor (factor VIIIR). Hyskon also places a patient at risk for fluid overload. The osmotic activity of dextran is such that for each gram of Hyskon instilled into the vascular space, 20 mL of interstitial water will be pulled into the circulation; 100 mL of Hyskon (32% dextran) will expand the plasma volume by 32 g × 20 mL, or a total of 640 mL. As the volume of intravascular Hyskon increases, a critical level is reached, and pulmonary edema occurs. Finally, dextran 70 (Hyskon) is a mixture of macromolecules ranging from 25 to 125 kd. Although the lower-weight molecules are rapidly excreted, the larger molecules can interfere with glomerular filtration and will remain in the bloodstream for 4 to 6 weeks.
Low Viscosity
Low-viscosity fluids must be continuously flushed through the uterine cavity if a clear view is to be obtained. Delivered fluid must be continuously circulated out of the cavity and clean fluid constantly added to make up for the deficit and maintain uterine distension. A standard diagnostic sheath does not allow for flushing. Therefore, if a low-viscosity fluid is used for distension, the view may be suboptimal because blood can mix with the distending fluid, creating a colored fluid through which the operator will see the field. The safest distending medium will be isoosmolar—that is, the electrolyte content will amount to 300 mOsm. Additionally, the sodium content of the fluid should approximate 140 mEq/L. The ideal lowviscosity fluid medium is 0.9% sodium chloride.
Regardless of the type of medium infused, the surgeon is responsible for monitoring the infused volume and reconciling that volume with the collected volume. Positive infusion differences require that the procedure be stopped when deficits range from 500 mL (for hypoosmolar fluids) to 1,000 mL (isoosmolar fluids). The surgeon and anesthesiologist must communicate, because fluid overload scenarios will usually necessitate the anesthesiologist helping to manage the ensuing pathophysiology. Additionally, intravenous fluids infused by the anesthesia team will add to the increased circulatory volume. Finally, any fluid including physiologic salt solutions can produce pulmonary edema when excessive volumes are administered via the hysteroscope, because the pressure gradient to maintain uterine distension is 60 to 70 mm Hg and subendometrial venous pressure is 4 mm Hg. Inevitably, fluids will diffuse into the venous circulation.
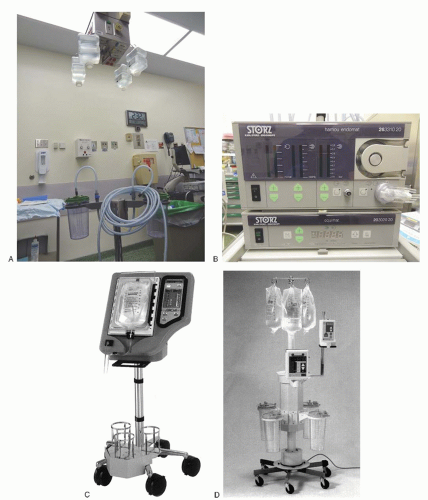
Low-viscosity distention media may be delivered by hanging a 2- to 3-L bag or bottle of fluid 6 to 8 feet above the operating table, permitting the fluid to infuse by gravity feed (Fig. 18.12A). An alternative is instilling low-viscosity fluid by rotary pump (Fig. 18.12B). The newest pumps weigh the fluid in real time and give the surgeon a constant readout of flow rate and total volume of fluid infused (Fig. 18.12C, D). Use of an automated fluid pump and monitoring system is advocated by both the American Congress of Obstetricians and Gynecologists and the American Association of Gynecologic Laparoscopists to most accurately monitor inflow and outflow and prevent complications associated with fluid overload.
Normal Saline, Ringer Lactate
Normal (physiologic) saline (0.9% sodium chloride) is perhaps the safest of any hysteroscopic media. Complications of excessive vascular absorption include fluid overload and pulmonary edema, which are managed by diuresis and support. The medium is readily available in 3-L sterile bags that can be mounted on an intravenous pole or given via an infusion pump. Garry and colleagues (1992) reported excellent safety results and precise maintenance of uterine pressure by using a pump delivery system, which was combined with one of the operating channels of the dual-channel operating sheath to provide an outflow tract and thus a constant flow rate through the uterine cavity.
Unfortunately, because saline is an efficient conductor of electrons, it does not permit a current density that is high enough for tissue action when using a monopolar system. Saline is therefore not suitable for monopolar electrosurgery, although it is effective when the Nd:YAG laser, the KTP/532 laser, bipolar electrode, and mechanical devices such as scissors are the hysteroscopic accessories of choice.
The optimal drape for the operating room is the urologic pouch (tucked under the buttocks) with a plastic reservoir pocket into which the outflow fluid may be collected and quantified to determine the fluid deficit (the difference between instilled fluid and returned fluid). The surgeon should be given a running account by a nurse or surgical assistant of the volume of fluid instilled, which is calculated as the liters of fluid hung minus volume of return fluid. Whenever any significant fluid deficit is calculated, usually considered 2.5 L for isotonic saline, the procedure should be discontinued and scheduled for completion at a later date.
Glycine 1.5% and Sorbitol 3%
Glycine (1.5%) and sorbitol (3%) solutions were first used in urologic surgery, principally for male patients. They were adopted later by gynecologists for use with monopolar electrosurgical devices such as the resectoscope. Both glycine and sorbitol are used for hysteroscopic distension, but both have disadvantages inherent to their composition. Since these solutions are hypoosmolar (sorbitol, 178 mOsm/L; glycine, 200 mOsm/L), the principal hazard relates to their vascular absorption and the creation of an acute hyponatremic, hypoosmolar state. A fluid deficit equal to or greater than 750 mL should alert the surgeon to a likelihood of hyponatremia and hypoosmolality. Two reports have presented data concerning significant complications secondary to hyponatremia. In one series of four women, two died (50% mortality); in the other, one of four women died (25% mortality). Absorption of hypoosmolar solutions produces a gradient between the circulating blood and the brain cells. The brain cells respond by pumping cation out to diminish the positive infusion of water into the brain. Unfortunately, the cation pumping mechanism of the brain is deficient in women, secondary probably to the actions of progesterone, and women are at significantly greater risk for the development of life-threatening cerebral edema when a hypoosmolar state exists. At a minimum, intraoperative and 4-hour postoperative serum sodium levels should be requested on a stat basis if concern for a fluid deficit using a hypoosmolar medium exists. A unique disadvantage of glycine is that it can be metabolized to ammonia and cause neurologic damage.
5% Mannitol and 2.2% Glycine
Mannitol (5%) and glycine (2.2%) may be used with electrosurgical devices and are approximately isoosmolar. Mannitol has an osmolality of 285 mOsm and is an osmotic diuretic. Its optical characteristics are equivalent to glycine and sorbitol; however, it is a safer medium. In a study of 181 hysteroscopic examinations using isotonic 2.2% glycine, although there was a mean decrease in sodium of 9 mmol/L in patients absorbing 1,000 mL, the serum osmolality remained normal with no significant adverse sequelae.
DIAGNOSTIC HYSTEROSCOPY TECHNIQUES
Diagnostic hysteroscopy can be performed in an office setting under local anesthesia. The injection of lidocaine 1%, 10 to 15 mL, directly into the cervix produces adequate anesthesia. Discomfort for the patient can be further diminished by ibuprofen (Motrin), 600 to 800 mg, administered 30 minutes before the procedure. Patients who require cardiac prophylaxis (e.g., artificial heart valves) should be covered by appropriate antibiotics. Informed consent clearly reviewing the risks, benefits, and alternatives should be obtained.
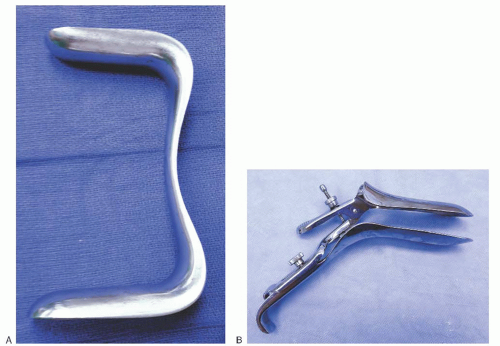
Accurate knowledge of the position of the uterus is critical to safely facilitate the procedure. The optimal view of the uterus is obtained during the proliferative phase of the menstrual cycle. After placing the patient in the dorsal lithotomy position, the perineum and vagina are gently swabbed with Betadine or another suitable antiseptic solution. A Sims retractor or breakaway speculum is inserted to allow visualization of the cervix (Fig. 18.13). The edge of the cervix at the 12 o’clock position is grasped with a single-toothed tenaculum. A suitable




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree