Multiple Gestations
Mary E. Revenis
The incidence of twins, triplets, and higher-order multiple gestations now accounts for approximately 3% of all pregnancies in the United States. The products of multiple gestations constitute a disproportionate number of admissions to neonatal intensive care units and suffer greater morbidity than do singletons. In 2002, 16% of all preterm deliveries in the United States were due to multifetal gestations (1). In addition to prematurity, the products of multiple gestations are susceptible to unique problems that may intensify as the numbers increase. A review of the major problems can help the clinician to anticipate the medical needs and prepare the parents for what lies ahead. Most of the issues discussed in this chapter apply to all multiple gestations.
▪ EPIDEMIOLOGY
The incidence of multiple gestations in the United States has increased dramatically during the past three decades as a result of the shift in maternal age distribution to older ages, as well as the increased use of fertility enhancement therapy. The number of births from twin deliveries and higher-order multiples rose, respectively, to 31.1 and 1.84 per 1,000 live births in 2002 (1). The actual rate of twin conceptions is much higher because early fetal loss with a vanishing twin is far more common than clinically recognized (2). In 1,000 pregnancies studied early with ultrasonography, Landy et al. (2) found a twin conception rate of 3.29%, with subsequent reduction to a single fetus in 21.2% of those pregnancies.
The incidence of naturally conceived higher-multiple births is mathematically described by the Hellin-Zeleny law, which states that if twins occur at a frequency of 1/N, triplets occur at a frequency of (1/N)2, quadruplets at (1/N)3, and so on. Because most epidemiologic studies exclude data on twins with no live-born member, they grossly underestimate the incidence of multiple gestations.
Natural monozygotic twinning reportedly occurs at a fairly constant rate of 3.5 to 4 per 1,000 live births, with limited variation among populations, but this is likely underestimated due to early losses. The occurrence of monozygosity is not affected by environment, race, physical characteristics, or fertility. The risk of monozygotic twins in assisted conception is two to four times higher than that in natural conceptions. The relatively new reproductive technologies of zona manipulation, intracytoplasmic sperm injection, and blastocyst transfer enhance artificial reproductive technology success but are also associated with a remarkable increase in monoamniotic twinning. The zona may act as a container for the dividing cell mass, disruption of which may allow for monozygotic twinning (3).
In contrast, rates for dizygotic twins vary greatly among populations, from 5 to 6 per 1,000 live births in Japan to 40 per 1,000 live births in Nigeria. Other factors that influence the incidence of dizygotic twinning include a maternally transmitted familial tendency, race, nutrition, parity, advanced maternal age, coital frequency, and seasonality. Twins are found most often in black populations and least often in Asians. Of concern during the current obesity epidemic, taller or heavier women bear twins at a rate 25% to 30% higher than short, undernourished women (3,4). Parity is an independent risk factor, with multiparous women having a greater likelihood for multiple gestations. Advanced maternal age predisposes to dizygotic twinning, with peak incidence at 37 years of age. Coital frequency has a positive affect, with a high rate of twin conceptions within the first 3 months of marriage. Another factor is the effect of the climatic seasons. In the Northern hemisphere, most dizygotic births are autumnal, reflecting more multiple ovulations during the winter and spring months. The seasonality of multiple births does not coincide with the peak months of singleton births (5).
High circulating levels of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) lead to the release of more than one ovum per menstrual cycle, making multizygotic conceptions more likely. Conception stimulants such as clomiphene citrate (Clomid, Serophene), which act by stimulating endogenous secretion of gonadotropins, raise the incidence of multiple gestations by 6.8% to 17%; exogenous gonadotropins such as menotropins (FSH and LH; Pergonal) or human chorionic gonadotropins (APL, Follutein, Pregnyl, Profasi HP) may increase the incidence as much as 18% to 53.5% (6). The women of the Nigerian Yoruba tribe, who have naturally elevated levels of FSH and LH, have a remarkably high rate of spontaneous, dizygotic twinning (1 in 20) (7). Martin et al. (8) examined another population and found that women with dizygotic twins have higher levels of FSH and estradiol than do women bearing singletons. A phenomenon likely due to increased pituitary gonadotropin release is the twofold higher incidence of twin conceptions in the 2 months after the cessation of oral contraceptives (9). High FSH and LH levels probably account for the seasonal variation in twinning observed in many countries (10).
▪ IMPACT OF REPRODUCTIVE TECHNOLOGY
The increasing use of ovulation-inducing drugs and assisted reproductive technology (ART) (in vitro fertilization [IVF], intracytoplasmic sperm injection, blastocyst transfer) has contributed to the 65% increase in multiple-gestation births in the past four decades. By 2011, 36% of twin births and 77% of triplet and higher-order births resulted from conception assisted by fertility treatments. The observed incidence of twin births increased by a factor of 1.9 from 1971 to 2009. The incidence of triplet and higher-order births increased by a factor of 6.7 from 1971 to 1998 and then decreased by 29% from 1998 to 2011. This decrease coincided with a 70% reduction in the transfer of 3 or more embryos during IVF and a 33% decrease in the proportion of triplet and higher-order births attributable to IVF (11). It is estimated that the number of non-ART fertility treatments (ovulation induction and intrauterine insemination) are comparable in number to the ART procedures and associated with even more triplet and higher-order multiple gestations. In 2000, only 18% of triplets were naturally conceived, with 40% a result of ART and estimated 40% due to ovulation induction (3,11). After adjustment for maternal age, the national rate of twin births increased by a factor of 1.6 from 1971 to 2009, and the national rate of triplet and higher births increased by a factor of 4.8 from 1971 to 1998, the year in which the highest rate was observed (3). In addition to the expected increase in dizygotic twins following assisted reproduction, monozygotic twinning with its higher incidence of complications is also more frequent in multiple gestations following assisted reproduction with an incidence of 3.2%, eight times higher than for spontaneously conceived pregnancies (3).
The multiple births resulting from ART are the major factor responsible for the increase in preterm delivery to 12.1%, up 29% from 1981. The use of ART accounts for 3.5% of low-birth-weight (LBW) infants and 4.3% of very-LBW infants in the United States because of absolute increases in multiple gestations and also because of higher rates of LBW among singleton infants conceived with this technology (12).
The number of embryos transferred during ART procedures is directly related to the risk of multiple gestations. The multiple rate increases from 33.9% with transfer of two embryos to 41.4%, 43.2%, and 46.5% with transfer of three, four, or five or more embryos,
respectively. The rate of triplets increases from 0.8% with transfer of two embryos to 7.4%, 8.4%, and 10.7% with transfer of three, four, or five or more embryos (13).
respectively. The rate of triplets increases from 0.8% with transfer of two embryos to 7.4%, 8.4%, and 10.7% with transfer of three, four, or five or more embryos (13).
Each cycle of ART is expensive and not often covered by insurance. An attempt to improve pregnancy success has encouraged transfer of multiple embryos during each procedure, especially for older women. As increasing the number of embryos transferred with ART increases the risk of multiple gestations and thus the risk of complications, the live birth rate is not always improved. For women less than age 35, the live birth rate for each embryo transferred is higher when only two embryos are transferred (42%) than when three (39.7%), four (35.4%), or five or more (33%) embryos are transferred (13,14,15).
The increase in multiple gestations due to ART and non-ART fertility procedures is associated with significant expenses due to increased need for perinatal surveillance and intervention, increased neonatal intensive care utilization, and long-term costs of care for chronic disabilities such as cerebral palsy. To reduce health care expenses, several European countries have passed regulations or guidelines addressing the number of embryos permitted to be transferred during ART procedures (16) or have agreed to pay the expense of ART cycles if a reduced number of embryos are transferred. In the United States, the progressively rising higher-order multiple birth rate finally decreased 9% from 193.5 per 100,000 live births in 1998 to 180.5 in 2000 (1), possibly indicating some moderation of the number of embryos transferred during ART procedures. There is ongoing debate as to whether regulations in the United States would be effective in reducing the numbers of multiple gestations following ART procedures and improving outcome at a lower cost (15,17).
▪ ZYGOSITY
Zygosity is determined by the number of ova fertilized. Higher-order pregnancies may be monozygotic, dizygotic, or multizygotic. In 1955, Corner (18) postulated that monozygotic twins develop by splitting of the conceptus at any time from day 2 after conception through days 15 to 17. The timing of division determines whether monozygotic twins are dichorionic, monochorionic, or conjoined. Dizygotic or multizygotic gestations result if more than one ovum has undergone fertilization at the same coitus or even at different times or with different mates.
At birth, zygosity can be determined by gender differences or by direct placental examination. Other techniques include blood typing, dermatoglyphics, and chromosome banding (19,20). The most precise technique is DNA variant restriction fragment length polymorphisms (21). Because monozygotic twins carry significantly higher risks of morbidity and mortality prenatally and postnatally, establishing the zygosity of all multiple gestations is clinically important. More effort is going into determining zygosity prenatally using ultrasonography or genetic identification techniques.
▪ PLACENTATION
The placenta from a twin gestation can be monochorionic or dichorionic; if dichorionic, it can be fused or separated, making four types of placentation possible:
Diamniotic, dichorionic separate
Diamniotic, dichorionic fused
Diamniotic, monochorionic
Monoamniotic, monochorionic
All dizygotic twins have a diamniotic, dichorionic placenta; all monochorionic twins are monozygotic. Zygosity should be determined in the case of twins of the same gender if the placenta is not monochorionic, because these siblings may be monozygotic or dizygotic. Fusion of the placenta does not differentiate zygosity. Table 24.1 lists zygosity determination based on placental examination.
TABLE 24.1 Zygosity Determination | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
Benirschke (23) described how to determine chorionicity of a fused placenta based on examination of the dividing membranes. The amnion contains no blood vessels and is more transparent than is the chorion, which contains fetal vessels and remnants of villous tissue. A monochorionic placenta is one in which the septum is composed of a thin, translucent amnion that can be easily separated and lifted from the chorionic plate. In a dichorionic placenta, the septum is thicker and more opaque. It does not separate as easily from the chorionic plate. Ultrasonography of the dividing membranes early in gestation is useful in some cases to determine the chorionicity, but it is not always technically feasible (24). Examination of the placenta and membranes should always be performed at delivery as ultrasound assessment may be erroneous (Fig. 18.3 and Fig. 24.1).
A monochorionic, monoamniotic placenta is formed by division of the embryonal disc at 7 to 13 days, which is after differentiation of the amnion. Only 1% to 2% of monozygotic twins are monoamniotic; the fetal mortality rate is as high as 50%, primarily due to twisting, knotting, or entanglement of the umbilical cords (27). Conjoined twins with their necessarily monoamniotic placenta result from the latest and incomplete splitting of the embryonic disc at days 13 to 15 of gestation. The monochorionic, diamniotic placenta with a dividing membrane consisting of two layers of amnion without an intervening chorion is formed at approximately 5 days of gestation. Dichorionic, diamniotic placentas are formed the earliest, within the first 3 days after conception.
▪ ANTEPARTUM COMPLICATIONS
Many complications of pregnancy occur more frequently in multiple gestations. Preterm labor is the most frequent complication, occurring in 20% to 50% of multiple gestations, most likely due to uterine overdistention. Pregnancy-induced hypertension, placenta previa, antenatal and intrapartum hemorrhage, hyperemesis gravidarum, and premature rupture of membranes all occur at a higher rate (28,29). Polyhydramnios, an almost expected complication of multiple gestations, is transient in pregnancies in which there are no other complications. If persistent, the polyhydramnios suggests abnormal fetal conditions, such as twin-to-twin transfusion syndrome (TTTS) or congenital anomalies (28,29).
▪ ANTENATAL MANAGEMENT
Recommendations for managing multiple gestations are controversial. The only unquestioned aspect of management is the benefit of early diagnosis, facilitating referral to an appropriate facility for high-risk infants. Antenatal management includes the following components:
Early diagnosis
Nutritional intervention
Cervical cerclage
Prophylactic tocolysis
Steroid stimulation of fetal lung maturity
Therapeutic amniocentesis
Multifetal reduction
Bed rest
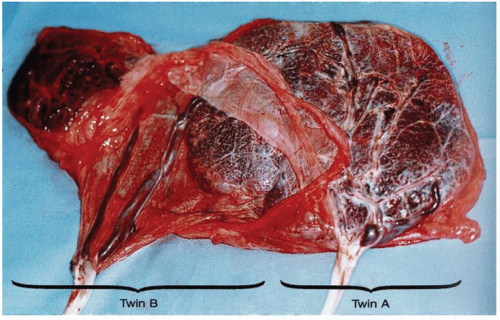 FIGURE 24.1 Marginal and velamentous insertions. This is a monochorionic diamniotic placenta in which the twin on the left (twin B) has a velamentous insertion into a bilobed placenta. Twin A has a marginal insertion. A prenatal sonogram was mistakenly interpreted as dichorionic because of the seemingly separate placentas. The occurrence of marginal and velamentous insertions increases with increasing numbers of fetuses (25). The risk for twin-to-twin transfusions is more than three times higher when a monochorionic placenta has a velamentous insertion (26). From Fletcher MA. Physical diagnosis in neonatology. Philadelphia, PA: Lippincott-Raven Publishers, 1998 (Figure 9, p. 78). |
Bed rest beginning before 28 weeks is commonly advised to decrease perinatal mortality (30). The National Institutes of Health (NIH) Collaborative Study showed no significant effect of antenatal betamethasone therapy in inducing fetal lung maturity in twins, but it is important to note that a relatively small number of twins were enrolled in the study (31). The 1994 NIH Consensus Statement on antenatal corticosteroids recommends betamethasone for all fetuses between 24 and 34 weeks of gestation, including multiple gestations (32).
There are several approaches to limiting the complications seen in higher-order multiple gestations. The first is to limit the number of embryos transferred during IVF to one or two. This results in a reduction in pre- and postnatal complications in the mother and infants but may decrease the take-home baby rates (14,15). An alternative is the use of multifetal reduction. Reduction, most often to twins, is usually performed at 9 to 12 weeks of gestation via either the transvaginal or transabdominal route (33). Reduction of quadruplets to twins improves overall outcome, but studies on the effect of reduction of triplets to twins have had conflicting results (33). In a recent review of trichorionic triplets, there was an increased rate of miscarriage (8.1% vs. 4.4%) and a decreased rate of early preterm delivery (10.5% vs. 26.7%) for pregnancies with embryo reduction compared to those expectantly managed. The ratio of reductions done to prevention of one early preterm delivery was 7:1 (34). Infants who are the products of reduced twin gestations have an increased incidence of impaired fetal growth and a lower gestational age at delivery when compared with nonreduced twins (12). Selective termination is used during the second trimester in pregnancies in which one twin is discordant for a major genetic disease or anomaly (35).
▪ LABOR AND DELIVERY
The total duration of labor in a twin gestation is similar to a singleton gestation, with some differences in the lengths of each stage such as a shorter latent phase during twin labor but a longer active phase and second stage, possibly due to dysfunctional labor in an over distended uterus.
There are many potential complications associated with delivery of multiple gestations, including malpresentation, cord prolapse, cord entanglement, vasa previa, locked twins, and fetal distress. Locked twins occur most often if the chins interlock to prevent expulsion or extraction of the first twin. Locking occurs at a rate of 1 per 817 twin gestations, and uterine hypertonicity, monoamniotic twinning, fetal demise, and decreased amniotic fluid are all contributing factors (36).
The best method of delivery depends on the number of fetuses, presentation of the first fetus, and gestational age. Table 24.2 details the frequencies of each variation of presentation. If both twins are vertex, there is no evidence that cesarean section improves outcome (36). In vertex-nonvertex twin gestations longer than 32 weeks, vaginal delivery is recommended (36). Delivery of the nonvertex second twin can be by total breech extraction or external cephalic version under ultrasound guidance and epidural anesthesia if the estimated weight is greater than 1,500 g, although the outcome is better with breech delivery of the second twin rather than manual version (36). If the first twin is nonvertex, delivery is usually by cesarean section (36).
Mode of delivery of the preterm multiple gestation depends on many factors, only one of which is the fetal presentation. If premature twins present in a vertex-vertex pattern without other complications, vaginal delivery is attempted, whereas a cesarean section is recommended for all other combinations of presentation if the gestational age is less than 34 weeks (36). When these recommendations are followed, there is no effect of mode of delivery or birth order on the incidence of intracranial hemorrhage in very-LBW
twins (37,38). Extremely-LBW twins (<1,000 g) have been shown to benefit from cesarean section, regardless of their positioning, with a reduction in postnatal mortality (39).
twins (37,38). Extremely-LBW twins (<1,000 g) have been shown to benefit from cesarean section, regardless of their positioning, with a reduction in postnatal mortality (39).
TABLE 24.2 Twin Presentation | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||
Delayed-interval delivery of multiple gestations is reported (40,41




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


