Monitoring Devices
IDEAL BEDSIDE NEWBORN INTENSIVE CARE UNIT MONITORING
Goals
Accuracy: Validation against gold standard measurements is needed. Accuracy of measurements must also span gestational age and birth weight differences of all patients in a newborn intensive care unit (NICU) setting. Movement of neonates should not significantly interfere with measurements. Fluctuation in temperature and humidity should also not affect monitoring.
Reliability: Application, data acquisition, and removal of monitoring devices should not be affected by differences in caregivers. Measurements should demonstrate minimal variation with respect to time of monitoring, caregiver, and infant position.
Feasibility: Devices should be minimally invasive, inexpensive, and easy to apply and remove for widespread use in a NICU setting. Minimal interference with patient care is essential, for example, with smaller-size neonatal sensors or with portable or wireless devices. Data would ideally be continuously recordable, easy to interpret, and compatible with simultaneous monitoring of other physiologic parameters. Real-time data collection would also allow personnel to respond to an event at the same time the data are being displayed.
Patient safety: Sensors, leads, or other methods of acquiring data must be safe for patient use. Considerations of skin sensitivity have led to the development of smaller-size hydrocolloid sensors. Risk of infection is typically minimized by disposable equipment or limiting duration of patient exposure to monitoring device interfaces. Signal interference between different modes of monitoring and electromagnetic radiation shielding must be considered for neonatal use of any monitoring device.
CARDIAC MONITORING
Electrocardiogram
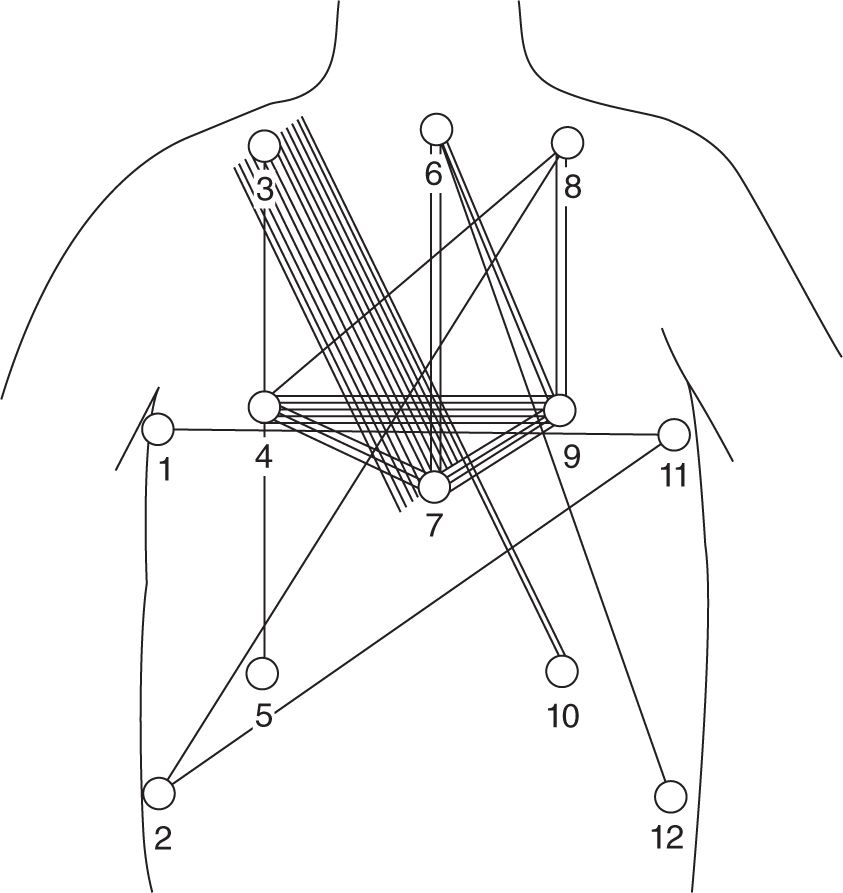
Description: An electrocardiogram (EKG or ECG) provides measurement of electrical signals generated by cardiac cell potentials by a surface electrode. The most common type of electrode for EKG monitoring is a silver-silver chloride, foil-based electrode. Instead of requiring a separate electrolyte solution to be applied to the patient, most EKG monitoring electrodes now come packaged in sets of three with an adhesive electrolyte gel backing (hydrogel) that serves as the electrolyte interface solution as well as an adhesive. An approaching excitation wave to a surface lead is recorded as a positive potential and represented on the EKG as an upward deflection. Typical lead placement and EKG module diagram are shown in Figure 5-1.
FIGURE 5-1 Optimal electrocardiogram (EKG) lead placement. (Adapted with permission from Baird TM, et al. Optimal electrode location for monitoring the ECG and breathing in neonates. Pediatr Pulmonol. 1992;12(4):247–250.)
Indications: The EKG is used for measurement of heart rate for conditions potentially leading to cardiac instability. Basic arrhythmias and abnormal waveforms may be detectable. However, for complete evaluation of arrhythmias, a 12-lead EKG is recommended rather than the typical 3-lead EKG used for continuous-monitoring purposes.
Accuracy/Reliability: Accuracy is dependent on skill level and experience of the interpreter. Computer-assisted interpretation should not be relied on for accuracy. Reliability for measuring heart rate is good, and signal is acquired more readily than pulse oximetry.
Limitations:
1. Artifacts: Computer-based cardiac monitoring systems now have more sophisticated filtering components to reduce noise and artifact. However, artifacts may still be generated by poor contact between skin and electrode or improper placement of leads. Electrical interference from other equipment may be problematic. Problems with cable connections, cables, or internal hardware or software failure of the EKG module may also contribute to artifact.
2. Skin fragility: In extremely preterm infants, removal of adhesive EKG leads has been associated with stripping of the stratum corneum, with the potential increased risk of infection1 and increased transepidermal water losses.2
3. Difficulties with lead placement: A limited flat thoracic surface, especially in a preterm infant, may cause difficulties with lead placement, resulting in more artifact generation.
4. Electrical safety: Allowable current level for flow through any patient-connected lead is established at 10 mA.3
Cardiac Output Monitoring
Impedance Electrical Cardiometry
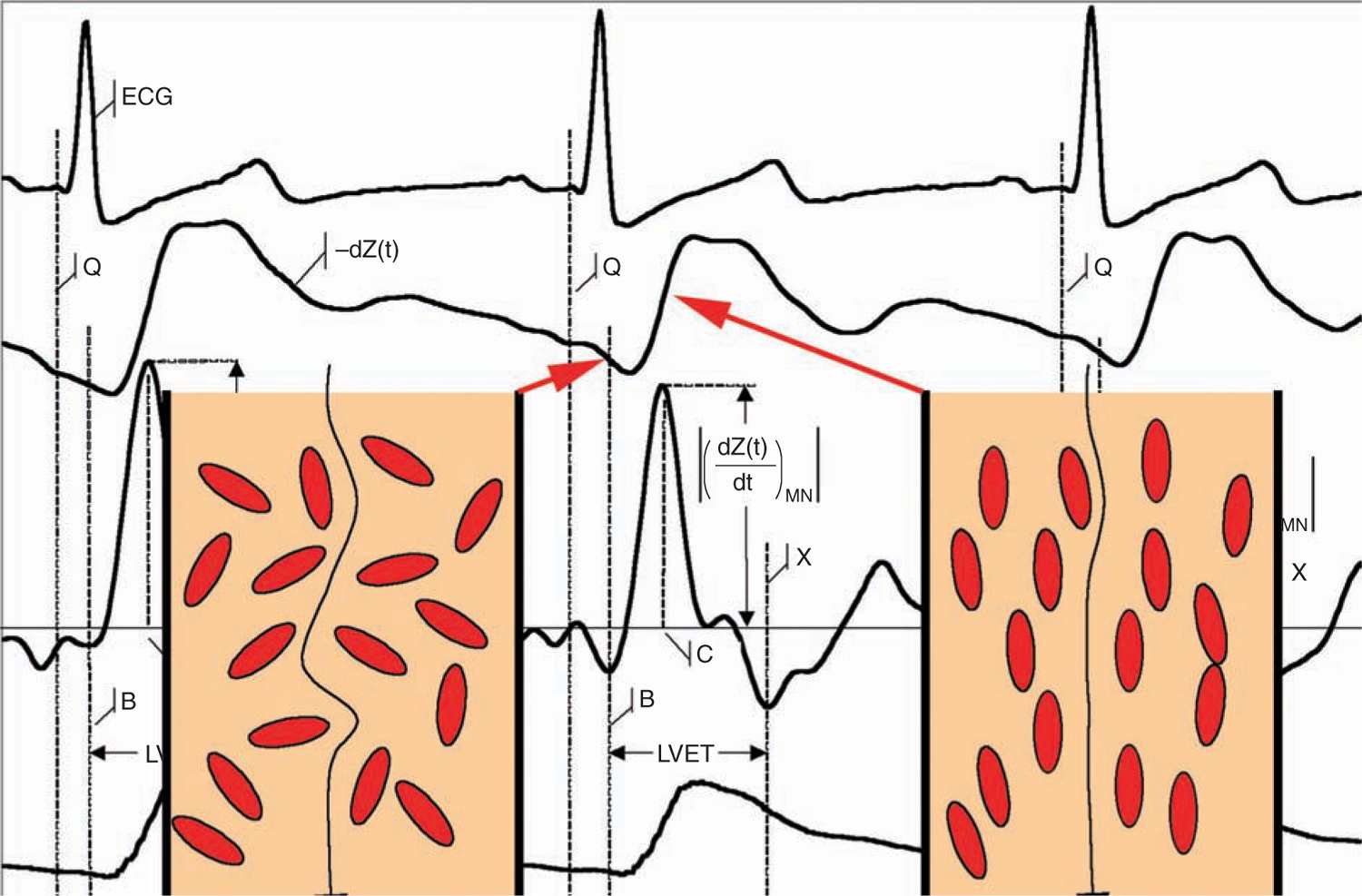
Description: Impedance electrical cardiometry is a noninvasive assessment of beat-to-beat cardiac output by measuring changes in thoracic electrical bioimpedance of aortic blood flow during the cardiac cycle with 4 adhesive skin sensors. The related concept of electrical velocimetry is based on the assumption that conductivity of blood in the aorta changes during the cardiac cycle. A random orientation of erythrocytes occurs during periods of no flow across the aortic valve (lower conductivity), followed by alignment of erythrocytes in parallel with blood flow during pulsatile flow across the aortic valve (higher conductivity). Impedance is the reciprocal of conductivity; thus, impedance waveforms are measured with this technology to calculate stroke volume and cardiac output4: SV (mL) × HR (1/min) = CO (mL/min) (Figure 5-2).
FIGURE 5-2 Parallel readings of electrocardiogram (EKG), impedance waveforms, and pulse plethysmogram. (Used with permission from Cardiotronic, Inc.)
Indications: This is potentially useful for monitoring of cardiac output in neonates with circulatory compromise. Infants with congenital heart disease, hypotension requiring pressors, infection, or other conditions contributing to hemodynamic instability may benefit from noninvasive cardiac output monitoring.
Accuracy/Reliability: This method was compared in adults to cardiac catheterization and thermodilution techniques employing the Fick principle for measurement of cardiac output as well as echocardiographic measurements of stroke volume and cardiac output.5–7 It was found that estimates of cardiac output from electrical cardiometry were highly correlated with both thermodilution techniques (precision of ± 0.46 L/min)7 and transesophageal Doppler echocardiographic measurements of cardiac output (r2 = 0.86).5 However, validation studies in the pediatric population are limited,8 and no data are currently available for the neonatal population.
Limitations: This procedure requires additional validation for use in neonatal patients. Because of varying degrees of ductal shunting in a neonate, measurements may not be accurate. Placement of sensors on the face, neck, and chest of a neonate may also not be feasible for some extremely small or preterm infants with skin sensitivity. An accurate weight must be input by the user to calculate stroke volume.
Continuous-Wave Doppler Ultrasound
Description: Compact continuous-wave Doppler ultrasound devices can be used for noninvasive serial measurements of cardiac output after acquiring a Doppler waveform of transvalvar flow.
Indications: Indications for use are conditions of hemodynamic instability or circulatory compromise as listed previously for which cardiac output measurements may be useful to assess response to treatment and time.
Accuracy/Reliability: Reliability of measurements largely is dependent on the experience of the user. Conflicting studies of preterm and term neonates using a continuous-wave Doppler ultrasound (USCOM; Coffs Harbour, NSW, Australia) found good interrater correlation (0.93)9 but poor correlation with conventional echocardiography measurements.10 When compared to the gold standard thermodilution method, a continuous-wave Doppler ultrasound device underestimated cardiac output during states of high cardiac output11 and showed poor agreement in children.12
Limitations: Currently, this technique is not ideal for continuous monitoring as the device must be held in place by the user. This requires training and experience to acquire appropriate images for accurate assessment of cardiac output. Difficulties in reliably measuring cardiac output require additional clinical research with this modality.9,10
RESPIRATORY MONITORING
Surface Monitoring
Transthoracic Impedance Pneumography
Description: Transthoracic impedance pneumography measures electrical impedance changes between two electrodes on the thorax during respiration. Change in impedance from breathing activity is separated from baseline impedance of the thorax, and then the signal is filtered by a microprocessor. Most devices utilize the same leads as used for EKG measurement.
Indications: This method is used for measurement of respiratory rate, especially during conditions associated with tachypnea, or for detection of apneic events.
Accuracy/Reliability: Measurement of breath amplitude by impedance pneumography had poor correlation with tidal volume, with higher values during supine positioning compared to prone positioning.13 This type of respiratory monitoring also frequently underestimated breath amplitude.14 Impedance monitors may also miss obstructive apneic events and misinterpret cardiac artifact as a breath.15
Limitations: Introduction of artifact is common because of improper lead placement, poor skin contact, or patient movement. Changes in impedance may also be introduced by changes in thoracic blood volume unrelated to respirations. The technique is less accurate for detection of obstructive apnea. Skin irritation from the electrodes may be a limitation, especially in preterm neonates.
Inductance Plethysmography
Description: In inductance plethysmography, a band containing an electrical wire coil is placed around the chest and abdomen of an infant. The inductance is measured and is proportional to changes in the area of the thorax and abdomen as the patient breathes.
Indications: This is another indirect monitor of respiration for infants requiring monitoring of respiratory rate or to detect apnea. Also, it is useful for estimates of lung tidal volumes because the signal is proportional to the tidal volume.
Accuracy/Reliability: Respiratory inductance plethysmography was more accurate than impedance pneumography in measuring breath amplitude in both prone and supine positions in neonates.14
Limitations: Breath activity may be underestimated because of postural changes or overestimated because of infant movement. Thoracoabdominal asynchrony may result in imprecision.16 Placement of an encircling band around the thorax and abdomen may be too cumbersome or lead to skin sensitivity in some infants.
Ventilator-Associated Devices
Pneumotachography
Description: In pneumotachography, sensors detect airflow, heat, or pressure changes when placed in series with the airway.
Indications: Mechanically ventilated patients requiring real-time monitoring of respirations, pressure waves, flow waves, and volumes to assist in adjustment of ventilation when patient lung compliance or resistance changes.
Accuracy/Reliability: Accuracy of measurements from a pneumotachograph when compared to spirometry-measured flows and volumes is largely dependent on the type of flow sensor, placement, and calibration techniques that are used.17
Limitations: This method is limited by the degree of air leakage around the endotracheal tube, which will make measurements inaccurate.
New Cardiorespiratory-Monitoring Devices
Several newer types of cardiorespiratory-monitoring devices are currently under development to eliminate the need for traditional EKG leads. One type uses a piezoelectric transducer sensor placed under an infant to detect an acoustic cardiorespiratory signal.18
BLOOD PRESSURE MONITORING
Continuous Blood Pressure
Description: Continuous blood pressure monitoring is obtained from an indwelling arterial line by a catheter pressure transducer in an umbilical arterial catheter or peripheral arterial catheter. Blood flow deflects a diaphragm, which is relayed into an electrical signal after adjustment for parameters such as viscous drag factor and stiffness of the transducer.
Indication: The need for recognition of hypotension or hypertension in critically ill or preterm infants may require continuous blood pressure monitoring. Ongoing monitoring of blood pressure changes in relation to interventions such as medication infusions or fluid boluses also would benefit from continuous reading.
Accuracy/Reliability: This method is considered gold standard for blood pressure measurements and the most reliable. However, signal dampening from malpositioned or clotted catheters may result in erroneous values.19
Limitations: An in-dwelling vascular catheter increases the risk of infection and thrombus formation. Catheter placement is also invasive and can be associated with life-threatening complications, such as necrotizing enterocolitis or pericardial effusions, if misplaced. These factors may limit duration of use. Artifacts may also be introduced by catheter movement or air bubbles in the system.
Indirect (Noninvasive) Blood Pressure Monitoring
Description: An occlusive device typically consisting of a cuff with an inflatable bladder is placed around an extremity to cause occlusion of arterial flow distal to the cuff. Measurements of systolic and diastolic pressure are obtained noninvasively during cuff deflation using the oscillometric method, which detects small pulsations in the artery through a pressure sensor (Figure 5-3). Different algorithms exist to convert these oscillatory signals into systolic and diastolic
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree