Practical Approach to Arrhythmias
INTRODUCTION
Tachycardias and bradyarrhythmias are important problems in the neonate. Clear understanding and recognition of these arrhythmias are important for optimal management.
TACHYCARDIA
Tachycardia can be either supraventricular (SVT) or ventricular (VT) in origin.
Atrioventricular Reentrant Tachycardia Including Wolff-Parkinson-White Syndrome
Pathophysiology
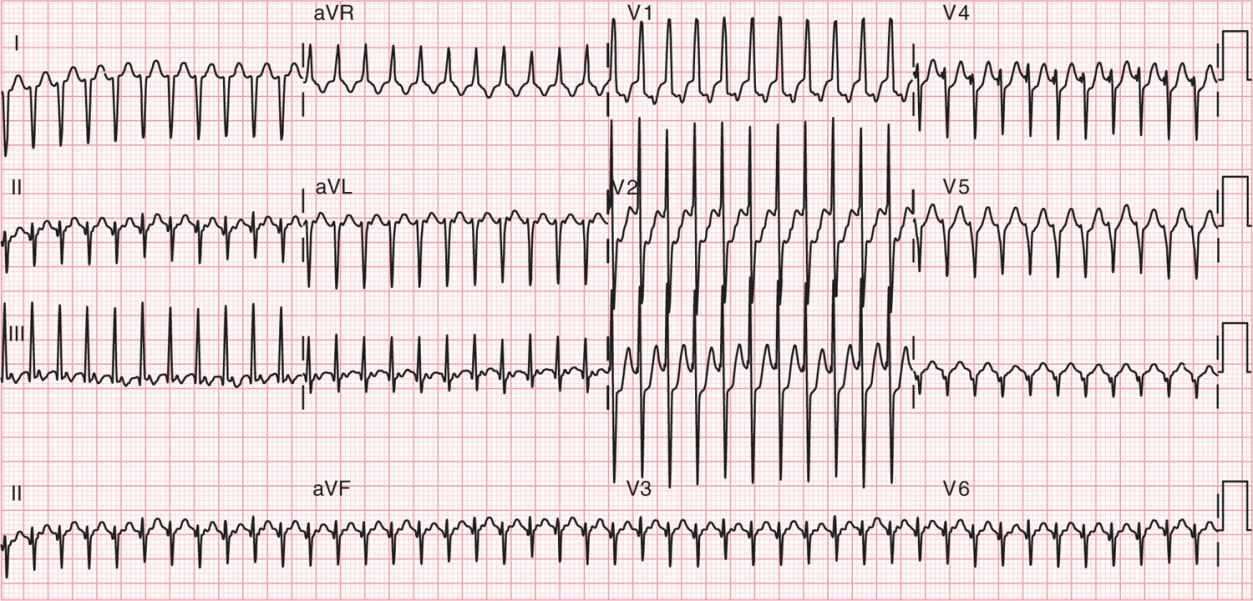
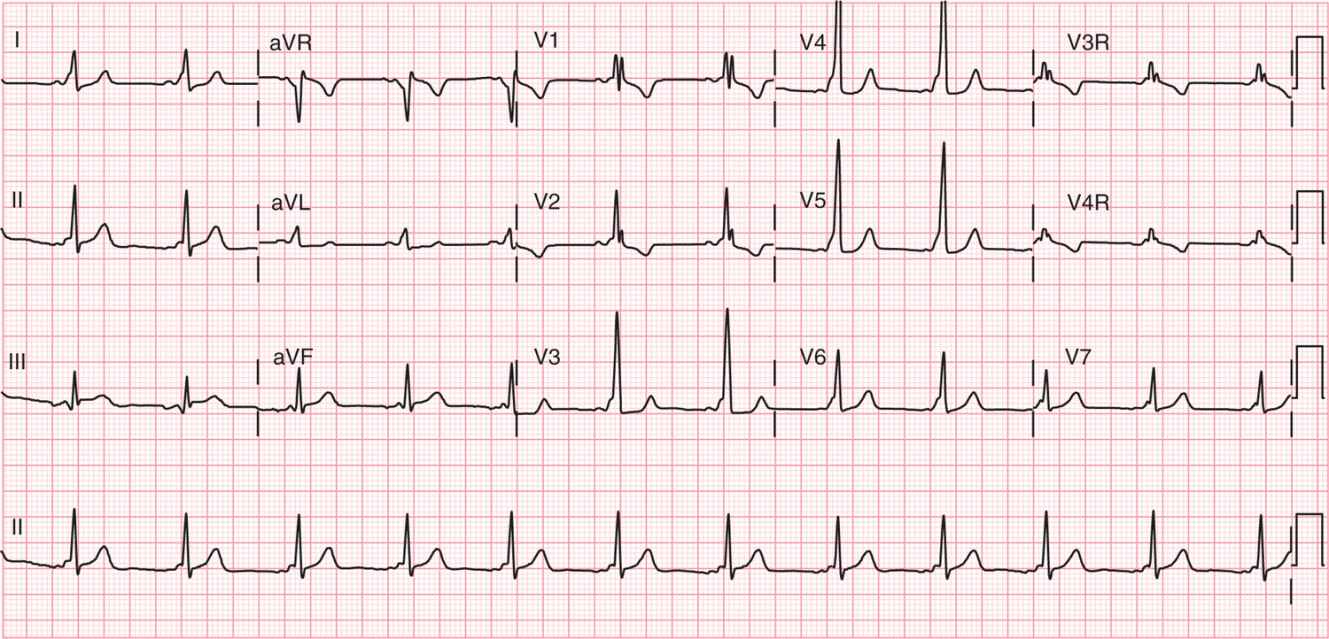
Atrioventricular reentrant tachycardia (AVRT) is the most common arrhythmia seen in the neonate. This reentry rhythm utilizes both the atrium and the ventricle and involves normal antegrade conduction across the atrioventricular (AV) node and retrograde conduction via an accessory pathway. This results in a narrow complex SVT, with retrograde p waves usually seen in leads II, III, and aVF and rates of 230–260 bpm (Figure 84-1). About one-third of accessory pathways are able to conduct antegrade as well and give the appearance of preexcitation or Wolff-Parkinson-White (WPW) syndrome on the baseline electrocardiogram (ECG) (Figure 84-2).
FIGURE 84-1 Electrocardiogram (ECG) of atrioventricular reentrant tachycardia in a 2-day-old. The ECG shows a narrow complex tachycardia at a rate of 280 bpm. Retrograde p waves are visible in leads II, III, and aVF.
FIGURE 84-2 Electrocardiogram showing Wolff-Parkinson-White syndrome. The patient is in sinus rhythm with a short PR interval and clear delta wave.
Presentation
The infant with neonatal SVT often presents with heart failure symptoms: poor perfusion, hepatosplenomegaly, poor feeding, and tachypnea. The differential for SVT must include infection with a sinus tachycardia.
Diagnosis
The 12-lead ECG will allow for accurate measurement of the heart rate and confirmation of the diagnosis.
Therapy
Acute management of SVT may include vagal maneuvers (ice to the face, rectal stimulation), intravenous adenosine (100–200 μg/kg as a rapid intravenous push), or synchronized cardioversion. Medical therapy consisting of β-blockers (propranolol 2–4 mg/kg/d orally divided four times a day) or digoxin (10 μg/kg/d divided twice daily) is used for chronic management; however, digoxin should not be used if the patient has WPW syndrome.
Follow-up
Neonatal SVT self-resolves in approximately 50% of children during the first year of life. If SVT does not resolve, ablation therapy is a curative procedure that can electively be performed when a child weighs more than 15–20 kg.
Atrial Flutter
Pathophysiology
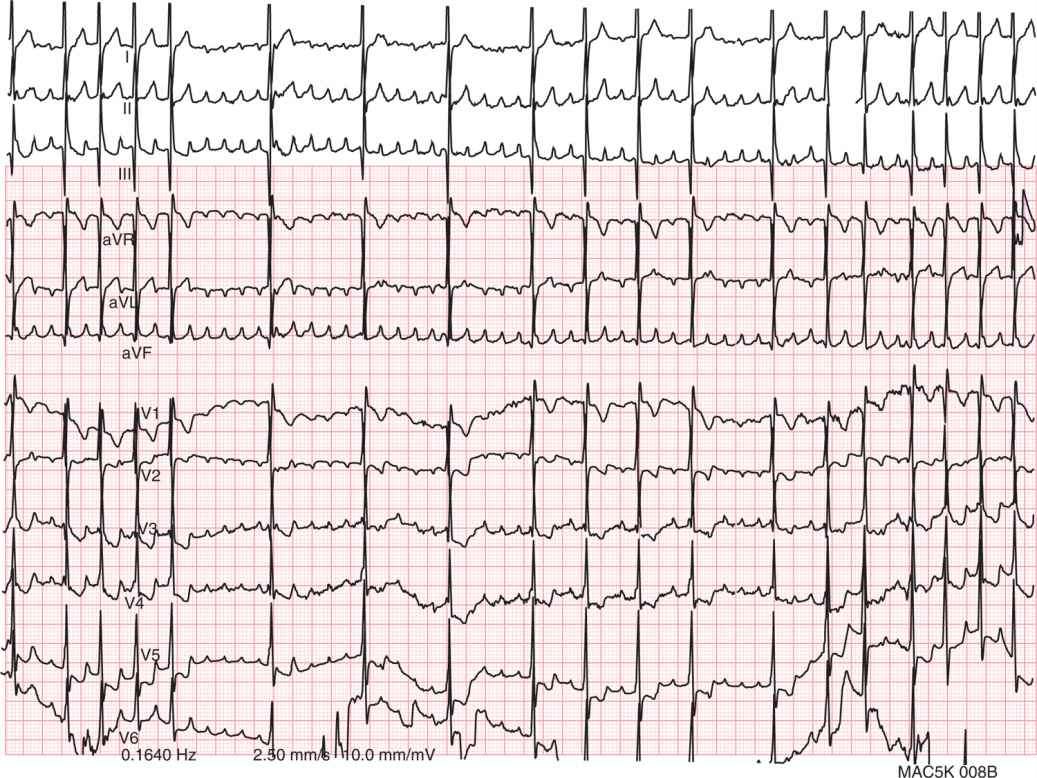
Atrial flutter is commonly seen in the newborn period. It is caused by a reentry rhythm within the atria. The ECG reveals a sawtooth pattern in the atria, best seen in leads II, III, and aVF, with an atrial rate between 300 and 500 bpm and 2:1 ventricular conduction (Figure 84-3).
FIGURE 84-3 Electrocardiogram of an infant in atrial flutter who has just received a dose of adenosine. The adenosine blocks conduction throughout the atrioventricular node (AVN), which allows for better visualization of the sawtooth pattern p waves and thus can be a useful aid for diagnosis of the rhythm.
Presentation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree