Laceration Repair with Sutures, Staples, and Wound Closure Tapes
Robert McNamara
Michael DeAngelis
Introduction
A laceration is a traumatic tear or opening in the skin surface. The goal of laceration repair is to reduce the risk of wound infection by restoring the skin’s protective barrier and ultimately to achieve a functional and cosmetically pleasing scar.
Over one third of injuries in children involve a laceration, making it the most common specific injury for which care is sought in a pediatric emergency department (1,2). In addition, a significant number of these patients seek treatment in primary care clinics (3). Laceration repair accounts for half of all procedures performed on injured children (4).
The incidence of lacerations in children is strongly correlated with the developmental level of the child. The initial rise in incidence occurs with the ability to ambulate. Lacerations peak at 2 years of age, when the child has attained greatest mobility but lacks equivalent motor coordination. Half of childhood lacerations occur in children under 5 years of age, and these lacerations frequently involve falls on broken glass bottles, wooden furniture, asphalt, or concrete (2,4). Lacerations resulting from assaults or altercations are more common in adolescents.
Animal bites also are a frequent source of lacerations in children. This is especially true in the preschool and early school years, when inadvertent provocation can result in an attack by the animal.
Common sites of lacerations in children are the head (60%), the upper extremities (23%), and the lower extremities (15%) (5). Lacerations of the head or face are proportionately greater in children under 2 years of age, as older children are more likely to break a fall by extending an arm or leg.
The majority of childhood lacerations can be treated without subspecialty assistance (4). The need for consultation depends on a number of factors, including the level of skill and experience of the clinician, the complexity of the laceration and involvement of underlying structures, the location of the laceration, and the ability of the child to cooperate.
Considering the frequency of lacerations during childhood, the importance of early repair, and the straightforward methods required for the majority of these injuries, every clinician treating acute injuries in children should be capable of repairing lacerations
Anatomy and Physiology
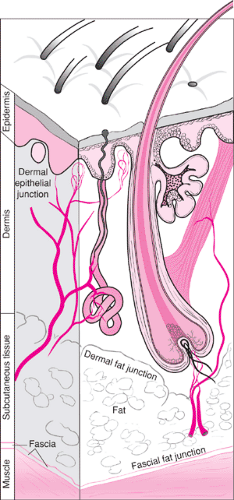
Knowledge of the anatomy and regenerative properties of the skin is crucial to performing an optimal laceration repair. The layers of the skin are depicted in Figure 108.1. The epidermis is the outermost layer and is composed of epithelial cells, whose function is to protect deeper tissues from infection and desiccation. Immediately beneath the epidermis is the dermis, which contains blood vessels, nerve endings, collagen, and fibroblasts. Below the dermis is the subcutaneous layer, which is composed primarily of fat cells. Hair follicles, nerve fibers, and blood vessels are also located in this layer. The subcutaneous layer is bounded below by a sheet of connective tissue called the fascia, which protects the underlying muscle and helps prevent superficial infection from spreading to deeper tissues.
The depth of the wound and the particular layers that have been disrupted are important factors in determining the best type of closure. Early contraction at the deeper levels
following injury frequently results in an inaccurate estimate of wound depth. The wound must be explored thoroughly for this reason. Certain layers retain sutures best: the fascial-fat junction, the dermal-fat junction, and the level just below the dermal-epidermal junction (Fig. 108.1). Adequate support of the affected tissue is a prerequisite for optimal closure and requires approximation of each involved layer. Improper alignment of the skin layers results in an uneven surface, which may cause shadowing and more obvious scarring.
following injury frequently results in an inaccurate estimate of wound depth. The wound must be explored thoroughly for this reason. Certain layers retain sutures best: the fascial-fat junction, the dermal-fat junction, and the level just below the dermal-epidermal junction (Fig. 108.1). Adequate support of the affected tissue is a prerequisite for optimal closure and requires approximation of each involved layer. Improper alignment of the skin layers results in an uneven surface, which may cause shadowing and more obvious scarring.
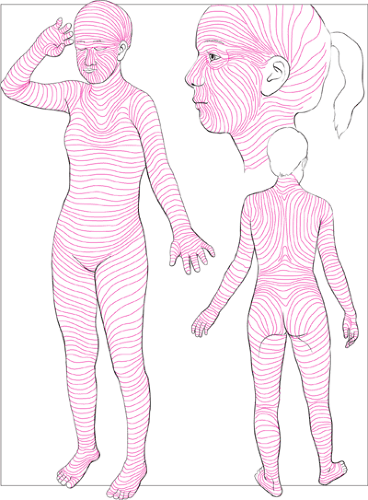
Intact skin is under constant tension. This tension has both a static component and a dynamic component. The skin in a particular location of the body possesses an intrinsic amount of tension that is determined partly by the underlying muscles and joints. Relaxed skin tension lines (RSTLs) lie perpendicular to the underlying muscle and are accentuated by contraction of the muscle (Figure 108.2) (6,7,8). They are best identified by gently pinching the skin and observing the furrows and ridges that are formed. Tension adjacent to these lines determines the initial extent of separation that occurs along a laceration and the ultimate width of the scar. Sutures provide temporary support until the skin can regenerate tissue capable of overcoming this tension and maintaining closure of the wound (2). Lacerations running perpendicular to these lines tend to gape more and require stronger sutures over a longer period to provide adequate support. Consequently, these lacerations are at increased risk for scarring. Lacerations that run parallel to these lines can be expected to heal more rapidly and with better cosmetic results.
The normal healing process of skin occurs over a prolonged period and involves multiple, sometimes overlapping, stages. The healing process is typically divided into coagulation, inflammation, epithelialization, angiogenesis, collagen formation, and wound contraction (9,10).
Coagulation occurs within the first hours following injury and involves vasospasm, platelet aggregation, and fibrous clot formation. Platelets also release factors that help trigger the response of inflammatory cells.
The inflammatory phase, which peaks at 24 hours after the injury, is marked by increased capillary permeability, which allows leukocytes to migrate into the wound. Neutrophils and macrophages act as scavengers to rid the wound of debris and bacteria. Macrophages also release chemotactic substances that stimulate fibroblast replication.
Epithelialization occurs as new epithelial cells grow and migrate across the wound edges. In a sutured laceration, complete bridging of the wound occurs within 48 hours (10). The placement of sutures creates a new wound through the epithelium, and the new epithelial cells will migrate along the track of the suture. These cells frequently disappear once the suture is removed; however, when sutures are left in place for prolonged periods of time or are placed under excessive tension, these epithelial cells are more likely to remain and form punctate scars along the edge of the wound.
Angiogenesis is the process of new blood vessel formation. The various stages of wound healing depend on the delivery of substrates, including nutrients, oxygen, and inflammatory cells, to the site of injury. Angiogenesis is crucial for providing the means of delivery for these substrates.
Collagen, the principal structural protein of most tissues in the body, is essential for restoring the tensile strength of the skin. Fibroblast deposition of collagen components begins within 48 hours after the injury (2). Various enzymatic processes result in the formation of fibrils. Subsequent cross-linking of these fibrils gives the collagen its maximal strength. Although the process of collagen synthesis reaches a peak in
the first week, remodeling continues for up to 12 months. A new scar will reach only one quarter of its ultimate strength by 3 weeks and less than two thirds by 4 months (10).
the first week, remodeling continues for up to 12 months. A new scar will reach only one quarter of its ultimate strength by 3 weeks and less than two thirds by 4 months (10).
Wound contraction is a poorly understood process in which the full wound thickness moves toward the center of the wound. This occurs 3 to 4 days following the injury and appears to be independent of epithelialization and collagen formation. This process is considered an important part of wound healing and should not be confused with the contracture that results from scar shortening.
Various factors, both internal and external, will inhibit the normal process of healing. Underlying immune deficiencies or prolonged steroid use can affect the inflammatory stage. The presence of crushed tissue or debris surrounding the laceration, as frequently occurs with blunt trauma, will significantly impede epithelial cell growth. Epithelialization is, therefore, optimized by meticulous attention to wound cleansing, débridement, and foreign body removal (Chapters 107 and 111). Collagen synthesis is a complex process that depends on the presence of a number of trace minerals, vitamins, and plasma proteins as well as an adequate supply of oxygen. Poor nutrition, underlying illness, or vascular disease will adversely affect this process.
As the microscopic process of healing proceeds, the appearance of the wound also undergoes predictable stages of evolution and remodeling. What may initially appear to be a cosmetically appealing result following suture removal often will go through a stage in which it becomes increasingly thickened, reddened, and elevated. This occurs during the active period of fibrous tissue production and remodeling, which lasts approximately 3 months. Over the next 3 months, the scar can be expected to fade and recede as capillaries collapse and the cellular content is replaced by connective tissue. The look of the scar 6 months following the initial laceration is essentially its final appearance (2).
Hypertrophic scarring and keloid formation are the result of abnormal healing, which can occur despite proper wound management and closure (11). Hypertrophic scars are composed of red, raised, pruritic tissue, which is the result of excessive collagen deposition occurring within the original boundaries of the wound. Keloids are nodular masses of scar tissue that also contain increased amounts of immature collagen and migrate beyond the original extent of the wound. Keloids occur with greater incidence in dark-skinned individuals and have a higher propensity for certain areas of the body, such as the sternum, deltoid, and mandible.
Children appear to have advantages in healing ability over adults. Studies suggest that in adults the stages of healing begin later, occur at a slower rate, and do not reach the same level as in children. With increasing age, collagen biosynthesis and cross-linking are decreased (12), the rate of epithelialization is reduced (13), and the proliferative capacity and contractility of fibroblasts are diminished (14). The underlying reason for these changes is difficult to determine due to the presence of multiple confounding factors. It is unclear whether these changes in wound healing are the result of prolonged environmental exposure or underlying disease or are simply part of the natural process of aging.
Indications
The basic goals of wound repair are to restore the integrity of injured tissue and to achieve a functional and aesthetically pleasing scar. These goals are best achieved by reducing tissue contamination, débriding devitalized tissue, restoring perfusion, and establishing a well-approximated skin closure (15).
Minor soft-tissue wounds are a common, unavoidable part of pediatric emergency care. Anxiety of the patient and family surrounding the repair of these injuries can be a source of much stress for the clinician. For these reasons, the ability to approach this situation in a clearly planned and confident manner is essential to the clinician’s long-term survival in pediatric emergency care. Skilled minor wound care can be a source of great patient and personal satisfaction and should receive major consideration in the education of emergency care providers.
Reasons to Seek Consultation
Not every wound should be repaired by the emergency physician. Consultation should be considered for the following kinds of wounds (16):
Wounds involving an open fracture or joint space disruption
Wounds involving tendons, nerves, or blood vessels
Wounds involving specialized structures (e.g., parotid duct, lacrimal duct, tarsal plate)
Wounds that would be better treated under general anesthesia due to their extent or location
Wounds that the emergency physician considers beyond his or her own level of expertise
The consulting service will vary with the injury and can range from general surgery for a wound complicated only by its extent to plastic surgery, otolaryngology, oral surgery, or orthopaedics for more specialized circumstances. If the initial receiving hospital does not have the appropriate specialist available, transfer may be necessary.
A difficult situation arises when the family insists on a plastic surgeon for a relatively minor wound that is well within the capacity of the emergency physician. To readily consult plastic surgery in all such cases is a poor strategy. Often a simple closure yields a wholly acceptable result, and the expense of a plastic surgeon and the time delay caused by such consultation is inappropriate for the situation (17). The clinician should reason with and inform the family that he or she is capable of handling the wound. The clinician also should inform the family that revision is unlikely to be needed but, if required, can be performed without difficulty at a later date under more favorable conditions.
With complicated wounds, immediate repair even by an experienced plastic surgeon may not always be the best strategy (18). A complicated repair in the acute phase is considered less desirable by some authorities for the following reasons: (a) a higher risk of infection may necessitate suture removal and undermine the initial effort; (b) it is more difficult to make the proper cuts for Z-plasty, etc., in damaged tissue as opposed to the firm scar base that will be present at a later date; (c) less time is available to study the natural tendencies of the wound; and (d) the patient has no basis of comparison with which to judge the outcome of plastic surgery (18).
Some emergency physicians will feel comfortable with extensor tendon repair; however, the requirement for close follow-up and patient compliance, coupled with the potential for significant disability, make referral a strong consideration in these cases. The emergency physician also must be aware that delayed repair of certain injuries, including nerve and tendon transection and complicated facial lacerations, is an acceptable response on the part of a contacted consultant (17).
Infectious Considerations
The risk of infection in a wound depends on the interaction of patient factors, the wound environment, and the care provided by the physician (6,9,19,20,21,22). When wound evaluation indicates that primary closure would be associated with a high risk of infection, it is recommended to leave the wound open for delayed primary closure or to allow healing by secondary intention (6,9,21). Loosely closing a wound should never be considered. The infectious risk with this method is generally the same as with primary closure (9).
Because the rate of wound infection in children is quite low, delayed primary closure is rarely used in the management of pediatric wounds. Studies examining all types of pediatric lacerations repaired with primary closure report infection rates as low as 1% to 2%. Bites, complex or long lacerations (greater than 3 cm), and wounds of the lower extremities seem to be at higher risk for infection (23,24,25). It is important to realize that if primary repair fails due to wound infection, the subsequent management is similar to delayed primary closure (22).
Patient Factors
Patient factors associated with an increased rate of infection include the presence of diabetes, renal failure, liver failure, immunosuppression, connective tissue disorders, obesity, and malnutrition (16,26). Wound infection rates for pediatric patients with these conditions are generally unknown, as wound studies typically exclude such patients. The presence of an underlying illness should not be the sole reason for avoiding wound closure, and the majority of wounds in these patients are amenable to primary repair. It is important, however, to pay close attention to wounds in such patients and to ensure adequate follow-up.
Local Factors
Local factors associated with the wound itself are the main source of wound problems in the ED (9,19). The clinician should always consider the following factors before wound closure.
Time Delay
Time is a variable factor in the closure of wounds, as some, such as a highly contaminated puncture wound, should never be closed, and others may be safely closed at almost any time after the injury (22). The “golden period” of wound repair is frequently mentioned, but this period is dependent on the characteristics of each individual wound. Although there is a strong relationship between the timing of wound closure and the risk of subsequent infection, the length of the “golden period” is highly variable (16,25,27).
Several studies have demonstrated that if a wound contains greater than 105 bacteria per gram of tissue, the probability of infection will be high (28,29,30). The mean time to achieve this level of contamination in one study was 5.17 hours, leading some authorities to consider the “golden period” to be quite short (29). Actual clinical studies, however, have produced results that support individual evaluation of wounds to determine if the time delay for closure is acceptable. No difference was found in infection rates for pediatric wounds sutured more than 6 hours after injury as compared with those repaired earlier (25). A study of wounds in a Third World setting found that it was safe to close general wounds for a period up to 19 hours, whereas scalp and facial wounds could be closed at any time (27). In one study evaluating hand wounds, time was not a factor in infection for a period up to 18 hours (30).
The primary determinant of a patient’s ability to resist wound infection is most likely the local circulation to the wound site (31). For that reason, injuries to well-vascularized areas such as the scalp, face, and tongue may be comfortably repaired many hours after presentation (19,31). In the previously mentioned Third World study, 97% of scalp wounds that were closed after 19 hours healed without complications (27).
Wound Contamination and Crush Injury
The degree of contamination is an important determinant of wound infection (6,28,29,30). Any foreign matter in the wound decreases resistance to infection. Soil components damage host defenses and raise the infective potential of bacteria. Saliva and feces are composed of concentrations of bacteria that greatly exceed the numbers needed to produce infection (6,9). The presence of devitalized tissue alone in a wound is considered a major risk factor for wound infection (6,31,32). Experimentally, inserting devitalized fat, muscle, or skin into a wound increases the infection rate (32). This occurs through inhibition of leukocyte function, creation of an anaerobic
environment, and the support of bacterial growth by the “culture medium” nature of the devitalized tissue (32).
environment, and the support of bacterial growth by the “culture medium” nature of the devitalized tissue (32).
Crush injuries are generally considered to be at higher risk for infection due to the presence of devitalized tissue and, more importantly, disturbances of local blood flow (33). Although this makes intuitive sense, clinical series supporting this hypothesis are limited. Separate studies on hand injuries demonstrated conflicting results when comparing infection rates in crush versus laceration-type injuries (29,34). In areas where the vascular supply is good, such as the scalp, the overall infection rate will be low regardless of the mechanism of injury (27,35).
The ability to sharply débride devitalized or heavily contaminated tissue will have a major impact on the decision to close a wound primarily (15,19,21). Débridement can convert a crushed, dirty wound into a clean, sharply incised laceration suitable for primary repair. Similarly, adequate wound irrigation can be expected to reduce the bacterial contamination of a wound and decrease the rate of subsequent infection (Chapter 107).
Wound Location
Although the wound location itself will usually not preclude primary repair, some general issues are pertinent to remember in evaluating wounds. Most studies demonstrate an increased rate of wound infection in injuries to the lower extremities (24,25,35). This is thought to be due to the relatively poor blood supply to the lower extremities (24,31). The foot may be at a particularly high risk (6). Upper extremity wounds also are considered to be at higher risk for infection, particularly hand wounds, for reasons similar to those that apply to the lower extremities (31,35).
Areas with significant exposure to endogenous bacteria such as the mouth, vagina, and perianal area are theoretically at high risk for infection (6). These same areas, however, also have an excellent vascular supply, counterbalancing the increased bacterial exposure (31). Closure of wounds in the mouth is generally considered acceptable if no major time delay has occurred (36,37). The low rate of infection of episiotomy incisions indicates some margin of safety for primary wound repair in the perineum. If in doubt about closure in one of these areas, consultation should be considered.
Location of a wound also may influence where the repair is best undertaken. Lacerations of the perineum may require closure in the operating room for the best result in terms of patient fear and anxiety. Wounds in inaccessible areas of the oral cavity also may require such management.
Bite Wounds
Mammalian bites account for approximately 5% of all traumatic wounds evaluated in the ED and up to 1% of all ED visits (38,39,40). Considerable controversy exists surrounding the proper management of both human and animal bite wounds. The clinician’s decision regarding closure in the case of a bite wound must weigh the various factors related to wound infection together with the supposition that the wound is contaminated with bacteria (19). The important considerations then become the vascular supply to the area and the ability of the clinician to adequately clean the wound and decrease the bacterial contamination present (16,23,41).
In all types of bite wounds, the hand is at an especially high risk for infection (42,43,44,45,46,47,48). The hand contains many poorly vascularized structures that do not resist infection well. Also, because the fascial spaces and tendon sheaths closely communicate, infection can spread quickly through the entire hand (41). In contrast, wounds of the head and neck have a much lower risk of infection. The location of the wound should also be assessed for cosmetic and functional significance. Although the hand is important functionally, wounds should generally be managed without primary closure. For cosmetic reasons, facial wounds are typically repaired immediately (16,23).
Dog Bites
Dog bites account for approximately 0.4% of all ED visits and 60% to 90% of all bite injuries treated in the ED (49). Children and young adults are the most frequent victims of dog bites, and most of their injuries occur on the head, neck, and upper extremities (40,49). Because the larger teeth of dogs facilitate the tearing of tissue, dog bites are more likely to result in lacerations than puncture wounds (50). Consequently, most of the bite wounds considered for suturing in the ED are caused by dogs. These wounds are assumed to be contaminated, although it has been stated that meal-eating (as opposed to meat-eating) dogs do not have sufficient oral bacteria to create an inoculum at the level of 105 bacteria per gram of tissue (19). As with human bites, dog bites to the hand are at higher risk for infection regardless of the use of antibiotics (45,46).
Although dog bite wounds are generally considered contaminated, recent investigations support primary closure of selected injuries (38,50,51,52,53). In one randomized clinical trial, the infection rate in 169 dog bite lacerations was the same for those sutured as for those left to heal by secondary intention (7.7%) (51). This was true even for dog bites of the hand. Other observational studies have also demonstrated equivalent infection rates for sutured and nonsutured dog bite lacerations (38,52). In one series of 91 patients with primary closure of dog bites lacerations, investigators reported an infection rate of only 4.4% (52). Another study reported an infection rate of 5.7% in 88 dog bite lacerations repaired primarily. The infection rates in this study did not differ between patients discharged with and without prophylactic antibiotics (38).
In general, dog bite lacerations of the face should be repaired primarily. If coupled with excellent wound care and meticulous closing technique, suturing of facial dog bite wounds can safely be accomplished with minimal risk of infection. In 145 pediatric facial dog bite wounds repaired after pressure irrigation and wound edge excision, an infection rate of only 1.4% was reported even though no antibiotics were administered (53).
Cat Bites
Cat bites account for approximately 5% to 18% of all animal bites treated in the ED (48,54). Because of a cat’s thin, sharp teeth, most bites result in puncture wounds (57% to 86%). Lacerations are much less common (5% to 17%) (48,54). The majority of these bites occur on the hand (48). Cat bites have a much greater risk of infection than dog bites. Their teeth are more likely to penetrate tendons, joints, and bone, resulting in deeper inoculation of bacteria. Also, the wound is difficult to explore and irrigate. The reported incidence of infection is as high as 30% to 50% (41,48,54).
Data are limited regarding the treatment of cat bite wounds with primary closure. Lacerations on the face may be considered for suturing, but in general sutures should be avoided in other locations. In one small study of cat bite lacerations on the face repaired with primary closure, there were no reported infections (48). Another study that included cat bite wounds located primarily on the head, neck, and upper extremities found an infection rate of only 4.4% after primary closure (38).
Human Bites
Human bites are the third most common mammalian bite in the United States, with the hand being involved in 60% to 75% of the cases (16). The notorious reputation of human bites is primarily based on one specific injury to the hand, the closed fist injury, or “fight bite.” This injury occurs when the closed fist strikes the teeth of another person, most commonly during a fight (16). The forces involved to create the skin break are generally sufficient to inoculate the tendon and its coverings, which lie just under the skin in this area. Frequently, deeper injury occurs to the bone, cartilage, and joint space. When the hand is subsequently extended, the bacteria are carried into areas not accessible to routine cleansing in the ED (42). In the pediatric age group, these wounds are usually infected by the time of presentation (44,45). Admission to the hospital and intravenous antibiotic therapy are generally indicated for an infected closed fist injury (16,41,42,45).
All patients presenting with a wound over the metacarpal head should be considered to have a human bite wound until proven otherwise. It is prudent to treat each wound in this location as a bite wound regardless of the history provided by the patient. If the wound is not infected at presentation, it should be thoroughly evaluated by wound exploration and radiographic study to detect any underlying injury that would prompt hospitalization. Patients scheduled for outpatient treatment must have their wounds thoroughly cleansed, left open, and elevated. These patients are routinely treated with antibiotics and must be capable of early follow-up (42).
In children, human bites usually occur with fighting (62%) or playing (26%). Most of these bites result in superficial abrasions (75%), which do not generally get infected (41,44). The literature on suturing human bite lacerations in children is limited. One small series suggested that the placement of deep sutures was associated with an increased rate of infection (44). However, primary closure of wounds in well-vascularized areas that can be adequately cleansed should not present a problem (23,38,55). The typical small forehead laceration that is caused by a playmate’s tooth is one example of a bite wound that should not be closed unless the wound is surgically extended for proper cleansing (44).
Other Animal Bites
Rodent bites account for up to 7% of all animal bites treated in the ED (54,56). Most of these bites result in small puncture wounds with a very low risk of wound infection. Lacerations caused by monkeys have a notorious reputation based on anecdotal reports, whereas those caused by large herbivores such as horses will be associated with significant crush injury (57). Recommendations on primary closure of these wounds are lacking given their relative infrequency.
Foreign Bodies and Wound Closure
The presence of a nonirritant foreign body such as a small piece of metal or glass is not a contraindication to primary wound closure (58). Such wounds can be closed and managed expectantly if the foreign body is difficult to remove, is not in a critical area (e.g., a joint space or near a vital structure), and is not positioned so that it would be a likely source of ongoing irritation for the patient. Certainly, the patient and family should be informed of the presence of a foreign body and the rationale for the planned course of action.
Irritant foreign bodies such as wooden splinters or thorns should be removed at the time of presentation to avoid infectious complications (Chapter 111) (58). The presence of even minute amounts of soil in a wound invites infection, and thus wounds with suspected remaining soil should not be closed primarily (6,9).
Gunshot and Stab Wounds
Low-velocity gunshot wounds that do not damage underlying structures can be managed on an outpatient basis. The traditional care of these wounds includes open treatment (no sutures) and basic wound care without using antibiotics (59,60). These wounds generally heal well without antibiotic therapy despite retained metallic fragments in the wound (59,60).
Stab wounds must be evaluated for depth and involvement or penetration of underlying structures before closure. This frequently necessitates surgical consultation. These wounds may be categorized as puncture wounds or simple, sharply incised lacerations. In the latter slashing-type injuries, the wounds may be closed like any other. Deeper puncture-type injuries are traditionally managed in an open fashion (Chapters 107,110).
Dead Space
Eliminating any pocket or “dead space” in the depths of a wound that could collect blood or serum and thereby potentiate infection is often accepted as an essential step in wound management. This must be distinguished from the technique of a layered closure to decrease tension on the wound edge, which has cosmetic advantages (6,61). Although theoretically
useful, the suture closure of dead space to decrease infection has not been clearly shown to be beneficial and may actually be detrimental (62,63,64,65,66). Animal studies suggest that deep sutures increase the risk of infection in contaminated wounds (63,65,66). In clean, noncontaminated wounds, however, this was not shown to be the case (65,66). Sutures through the adipose layer should be avoided. These sutures do not help to relieve tension, and they increase the rate of infection (61,62,64).
useful, the suture closure of dead space to decrease infection has not been clearly shown to be beneficial and may actually be detrimental (62,63,64,65,66). Animal studies suggest that deep sutures increase the risk of infection in contaminated wounds (63,65,66). In clean, noncontaminated wounds, however, this was not shown to be the case (65,66). Sutures through the adipose layer should be avoided. These sutures do not help to relieve tension, and they increase the rate of infection (61,62,64).
Equipment
Basic surgical tool requirements useful for wound repair are listed below.
Needle holder. The size of the needle holder should match the size of the needle selected for suturing. An excessively large needle holder will flatten a small needle after only a few uses (67).
Tissue forceps. Tissue should be manipulated gently with forceps to avoid any crushing effects. An alternative to forceps is a single- or double-pronged skin hook (67).
Tissue scissors. A sharp, tightly cutting pair is essential for débridement (68).
Hemostats. These may be useful in situations when bleeding vessels will require ligation (68).
Scalpel. A No. 10 or 15 blade may be necessary for sharp débridement (68).
Sterile drapes. An adequate amount of drapes should be used to keep the wound area sterile. In the repair of facial wounds, the hole in the drape should not be so small as to obscure useful landmarks (36,67). Drapes over the face can be forgone if they cause excess anxiety in a child.
Sterile gauze. A ready and sufficient supply of gauze pads is frequently overlooked in setting up for laceration repair.
Sterile gloves. Although the use of sterile gloves (as opposed to clean, nonsterile gloves) has never been proven to reduce the rate of wound infection, this practice is still generally recommended. Of note, a recent multicenter, randomized clinical trial reported no difference in wound infection rates when clean, nonsterile gloves were used instead of sterile gloves for wound closure (69).
Mask. A mask is important for reducing contamination of the wound and protecting the clinician from mucous membrane exposure (6,68). One study, however, did not find any significant difference in wound infection rates when comparing lacerations repaired by clinicians with and without masks (70).
Light. An adequate light source is essential and should preferably be directed into the wound unobstructed from above.
Bed. The patient and bed should be positioned in such a way as to maximize the comfort of both the patient and the clinician during the procedure. Using arm extensions and pillows should be considered, and the height of the bed should be raised to a workable level.
Suture material (6,15,67,71,72,73,74,75,76). Sutures are divided into two general classes, absorbable and nonabsorbable, based on their rate of degradation. Sutures that undergo rapid degradation, losing their tensile strength within 60 days, are considered “absorbable.” Sutures that maintain their tensile strength for greater than 60 days are considered “nonabsorbable.”
Several types of nonabsorbable sutures are available for percutaneous suturing; however, the general choice for emergency physicians will be a synthetic monofilament type such as nylon (Dermalon, Ethilon) or polypropylene (Prolene). The monofilament sutures are preferred over braided or multifilament sutures, which are thought to increase the risk of wound infection by providing interstices for bacteria to be shielded from leukocytes. Most synthetic sutures possess a low coefficient of friction that allows the them to pass smoothly through tissue. This same property, however, lessens the stability of the knot, and therefore the clinician should use at least four throws when tying knots with synthetic material. Silk is more reactive than synthetic suture material, which limits its usefulness for general wound repair. The relatively soft feel of silk and its workability make it a consideration for repairs of the eyelid or mouth. In these areas, silk sutures are usually removed in a few days, thus lessening the reactivity problem.
Absorbable sutures are typically used to approximate the dermal area in deeper lacerations. Synthetic absorbable sutures are generally less reactive and have greater tensile strength than sutures from natural sources, such as catgut. Two commonly used synthetic absorbable sutures are polyglycolic acid (Dexon) and polyglactin (Vicryl). The use of absorbable sutures for skin closure has traditionally been discouraged because of the material’s greater tissue reactivity and potential for increased scar formation. Recent studies, however, suggest that cosmesis is equivalent for wounds closed with absorbable and nonabsorbable sutures (74,75,76). One study, comparing the use of plain gut and nylon sutures in the repair of 95 uncomplicated pediatric lacerations, found no difference in cosmesis at 4 months (75). Another study comparing the use of rapid (“fast”) absorbing gut versus nylon sutures in 84 patients with facial lacerations found no significant difference in cosmesis at 9 months (76). The primary advantage offered by the use of absorbable sutures for skin closure is that a return visit for suture removal is not required.
The size (diameter) of the suture material is a measure of its tensile strength. The appropriate suture size chosen for a repair depends on the tensile strength of the tissue being approximated. The clinician should select the smallest size suture that will adequately hold the tissues in place and thus minimize the amount of foreign material in the wound. In decreasing order of size and tensile strength, the sutures commonly used in the ED run from 3-0 to 6-0. In general, 3-0 and 4-0 absorbable and nonabsorbable sutures are used for fascial closure, 4-0 and 5-0 absorbable sutures for dermal closure,
and 4-0 to 6-0 nonabsorbable sutures for skin closure. 6-0 sutures are used for the repair of facial wounds, whereas the use of 3-0 sutures is usually limited to the repair of wounds of the scalp or other areas of significant tension (e.g. wounds overlying joint surfaces).
and 4-0 to 6-0 nonabsorbable sutures for skin closure. 6-0 sutures are used for the repair of facial wounds, whereas the use of 3-0 sutures is usually limited to the repair of wounds of the scalp or other areas of significant tension (e.g. wounds overlying joint surfaces).
Needles. The reverse cutting needle is the best choice for general wound repair in the ED. This needle has its cutting edge situated on the outside of the curve of the needle so that the cut is made away from the wound edge, which prevents the suture material from further cutting into the tissue along the path of the needle cut.
Procedure
Wound Preparation
General wound preparation and cleansing is critical for optimal wound repair, and this topic is detailed in Chapter 107. The repair of lacerations is perhaps the most common indication for using procedural sedation in the young child, and this technique is detailed in Chapter 33.
Anesthesia
Adequate anesthesia is essential for proper wound evaluation and closure (16,31). The application of local and regional anesthesia is detailed in Chapter 35. A few additional comments are herein emphasized. Complete anesthesia of the affected area must be accomplished before wound manipulation. It is the fault of the clinician and not the patient if the anesthesia is not satisfactory. If the anesthesia is inadequate, the clinician must retreat and start over to ensure a wound repair that is least distressing for both the patient and family.
The most common form of anesthesia used for laceration repair remains local infiltration. Although this method is the most reliable, local infiltration is painful and subjects the clinician to the risk of an inadvertent needle stick. Many strategies have been suggested to reduce the pain associated with infiltration. These include using small-gauge needles, buffered solutions, warmed solutions, a slow rate of injection, injection through the wound edges, subcutaneous rather than intradermal injection, and pretreatment with topical anesthetics (16,23,77,78,79,80,81,82,83,84,85).
An alternative method for the administration of local anesthesia is topical application of local anesthetics. Several such anesthetics have been used, including a combination of lidocaine, epinephrine, and tetracaine (LET). The major advantage of these agents is painless application and reduced patient anxiety (86,87,88,89,90,91). Although the onset of anesthesia is more delayed than with local infiltration, the application of topical anesthetics has been shown to significantly reduce the total treatment time in children with simple lacerations (92).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree