Hernias and Umbilicus
Frederick J. Rescorla
Indiana University School of Medicine, Indianapolis, JW Riley Hospital for Children, Indianapolis, Indiana 46202.
INGUINAL HERNIA
Embryology
Most inguinal hernias in infants and children are indirect inguinal hernias due to a patent processus vaginalis. The pertinent embryology of the inguinal region relates to the development and descent of the testes and their relation to the processus vaginalis.
The gonads develop near the kidney as a result of migration of primitive germ cells from the yolk sac to the genital ridge, which is completed by 6 weeks’ gestation. Differentiation into testes or ovaries occurs by 7 or 8 weeks’ gestation under hormonal influences. The gubernaculum forms from the caudal end of the mesonephros and is attached to the lower pole of the testes. The lower portion of the gubernaculum has several thin, cordlike structures that appear to guide the testes into the scrotum. These occasionally pass to ectopic locations (perineum or femoral region) outside the line of normal scrotal descent. Downward retroperitoneal migration of the gonads starts at about 3 months’ gestation. The ovary reaches the pelvic brim at about 12 weeks’ gestation and remains at this level. The remnant of the gubernaculum in girls forms the ovarian and uterine ligaments. The testes continue to descend, reaching the level of the internal ring by 7 months’ gestation.
The peritoneum bulges into the inguinal canal as the processus vaginalis during the third month prior to testicular descent. The gubernaculum precedes the testes and begins to shorten as it approaches the bottom of the scrotal sac. The testes descends from the internal inguinal ring during the seventh month of gestation and passes through the inguinal canal in a few days, but takes about 4 weeks to migrate from the external ring to the lower scrotum. As the testis evaginates the abdominal wall, the layers of the spermatic cord are formed from the layers of the abdominal wall. The internal spermatic fascia forms from the transversalis fascia, the cremasteric fascia from the internal oblique and transversus abdominis muscle, and the external spermatic fascia from the fascia of the external oblique.
The processus vaginalis normally closes during the last few weeks of term gestation after the completion of testicular descent. It obliterates initially both at the level of the internal inguinal ring and just above the testes. The portion adjacent to the testes becomes the tunica vaginalis. In girls, the canal of Nuck corresponds to the processus vaginalis, opens into the labium majus, and usually obliterates earlier than the male processus vaginalis.
Failure of the processus vaginalis to close accounts for nearly all inguinoscrotal abnormalities seen in infancy and childhood. Although reason for failure of closure is unknown, it is more common in cases of testicular nondescent and prematurity. In addition, persistent patency is twice as common on the right side, which is probably related to later descent of the right testis.
Pathology
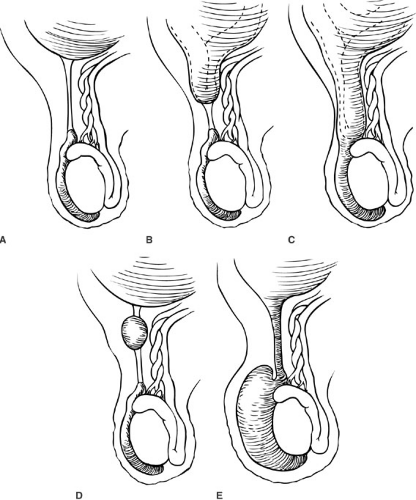
An indirect inguinal hernia occurs when intestinal contents enter the inguinal region through a patent processus vaginalis. Depending on the degree of patency of the distal processus, the hernia may be confined to the inguinal region or pass down into the scrotum (Fig. 68-1). A communicating hydrocele occurs when the opening is narrow, allowing fluid but not intestinal structures to pass into the inguinoscrotal region. A scrotal hydrocele occurs when the proximal portion of the processus vaginalis obliterates and the tunica vaginalis fills with fluid. A hydrocele can also occur along the cord because the processus may obliterate proximal and distal to an isolated cystic dilation. In little girls, the processus (canal of Nuck) may remain patent and may fill with fluid, or allow the ovary and fallopian tube to enter the inguinal region.
Clinical Presentation and Initial Management
Presenting Symptoms
A hernia is generally identified as a bulge in the area of the lower abdominal crease, with varying degrees of extension from the area of the internal inguinal ring down along the path of the cord structures to the hemiscrotum. The differential diagnosis includes a communicating hydrocele, which usually has a history of size fluctuation, transilluminates on examination, and is usually not reducible on physical examination. Other, less common abnormalities include torsion of the testes and inguinal lymphadenopathy. In addition, a retractile testis frequently is felt as a mass just below the external ring. In girls, an asymptomatic labial mass is frequently identified. If not repaired, this can lead to torsion and strangulation of the ovary and fallopian tube. In most patients, the hernia reduces either spontaneously or with gentle pressure by the parent or physician.
Conditions associated with an increased occurrence of inguinal hernias include prematurity, undescended testes, epispadias, bladder exstrophy, ambiguous genitalia, and a family history. Inguinal hernias are more common in children with increased intraabdominal pressure secondary to abdominal wall defects and in children in whom ventriculoperitoneal shunts or peritoneal dialysis is used.
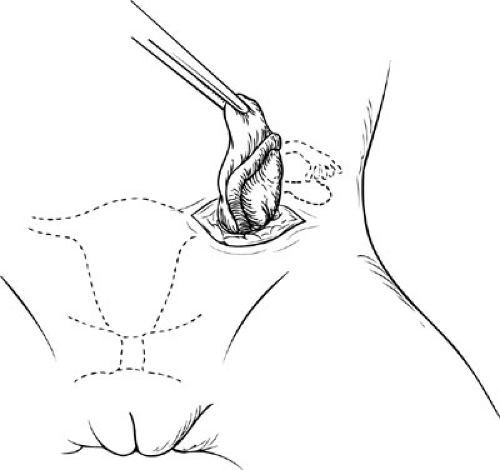
At initial examination, an attempt should be made to reduce the hernia. This can be facilitated with one hand applying gentle pressure on the lowest aspect of the hernia and the other hand forming an inverted V at the level of the internal inguinal ring to force the hernia contents back through and not superficial to the external inguinal ring (Fig. 68-2). If reduction is not possible, the hernia is incarcerated.
Incarceration
Incarceration represents the most common complication associated with inguinal hernias. Incarceration is reported in 6% to 18% of patients in several large series (1,2,3), and several researchers have reported rates of about 30% for infants less than 2 months of age (1,4). Contained structures can include small bowel, appendix, omentum, colon, or, rarely, Meckel diverticulum. In girls, the ovary, fallopian tube, or both are usually incarcerated. Rarely, the uterus is drawn into the sac along with the fallopian tube.
It is essential at the time of the initial evaluation to attempt reduction of an incarcerated hernia. The only exception to this is a long-standing incarceration with evidence of peritoneal irritation. Reduction can be attempted in the presence of uncomplicated clinical and radiographic bowel obstruction. An attempt by the surgeon with several minutes of gentle pressure is usually successful. If unsuccessful, sedation administered intramuscularly or intravenously may allow adequate relaxation to allow reduction.
Indications for Surgery
Due to the high rate of complications associated with inguinal hernias, repair is generally recommended shortly after the diagnosis is established. In an otherwise healthy child with an easily reducible hernia, outpatient surgery is scheduled within a few weeks at the convenience of the parents and surgeon. If reduction is moderately difficult, repair should be performed within a few days and the parents advised to return if incarceration occurs. If reduction is difficult or requires sedation, most surgeons admit the child for close observation and perform the procedure within the next 24 hours. The child with one episode of incarceration may have another and should be observed closely. An irreducible hernia requires immediate exploration.
In girls, hernias frequently appear as asymptomatic labial masses that can be difficult to reduce. The ovary is usually not strangulated, and the question arises as to the urgency of repair of an irreducible structure that is not compromised and that may have been incarcerated for days or weeks. The occurrence of strangulation of ovaries in this location is well documented so same day or next day repair is probably the most prudent.
Premature infants diagnosed with hernias while hospitalized in the neonatal units can be safely repaired before discharge. The neonatal staff can observe these patients, and as long as reduction is easy, repair can be delayed. Premature infants with inguinal hernias diagnosed after discharge may have surgery delayed to allow a general anesthetic on an outpatient basis if the hernia is easily reducible. Because the natural history of communicating and noncommunicating hydrocele can result in spontaneous closure and resolution, a period of observation until 1 year of age is generally warranted.
Contralateral Side
Few topics in pediatric surgery have drawn as much attention or generated more controversy than the management of the contralateral side in children presenting with a unilateral hernia. The only purpose of a contralateral exploration is to avoid the occurrence of a hernia on that side at a later date. The advantages of routine contralateral exploration are related to avoiding the issues associated with the development of a contralateral hernia, including parental anxiety, cost, anesthesia, and risk of contralateral incarceration. The disadvantages include potential injury to the vas deferens and testes, increased operative time, and the fact that in many infants it is an unnecessary procedure. The relevant issues in the debate revolve around the frequency of occurrence of contralateral hernias and the relation of this to age, gender, and side of the clinically apparent hernia. A more recent survey by Levitt et al. (5) found that 51% of surgeons routinely explore the contralateral side in prematures, 40% do so in boys younger than 2 years and 13% in boys ages 2 to 5 years. Routine contralateral exploration in girls younger than 5 years was performed by 39% of surgeons.
Rothenberg and Barnett (6) in 1955 reported that the contralateral processus vaginalis was patent in all the
infants in their study who were younger than 1 year and in 65% of those older than 1 year. Kiesewetter and Parenzan (7) attempted to determine the role of contralateral exploration in children younger than 2 years. They performed contralateral exploration in 100 infants with clinical unilateral hernias and identified a contralateral patent processus vaginalis in 61% of cases. A second group of 237 infants underwent unilateral repair only, and 31% went on to have contralateral hernias. In view of these data, Kiesewetter and Parenzan recommended bilateral repairs for children younger than 2 years.
infants in their study who were younger than 1 year and in 65% of those older than 1 year. Kiesewetter and Parenzan (7) attempted to determine the role of contralateral exploration in children younger than 2 years. They performed contralateral exploration in 100 infants with clinical unilateral hernias and identified a contralateral patent processus vaginalis in 61% of cases. A second group of 237 infants underwent unilateral repair only, and 31% went on to have contralateral hernias. In view of these data, Kiesewetter and Parenzan recommended bilateral repairs for children younger than 2 years.
A similar study by Sparkman (8) in 1962, involving 918 infants and children, identified a contralateral patent processus vaginalis (CPPV) in 57%. A second group of 1,944 children underwent unilateral repair only, and 15.8% had subsequent contralateral hernias. In a review of 2,764 patients undergoing routine contralateral exploration, Rowe and colleagues (9) reported a decreasing patency rate with advancing age. Patent processus vaginalis was seen in 63% of infants younger than 2 months, gradually decreasing to an incidence of about 40% after 2 years of age.
Two more recent reports of unilateral repairs at all ages observed a somewhat lower incidence of contralateral hernias, but also focused on the side of recurrence. A 20-year follow-up study reported an overall contralateral hernia occurrence rate of 22%, with a 41% occurrence rate of a right hernia after an initial left hernia repair and a 14% occurrence rate of a left hernia after an initial right repair (10). In a review of 904 unilateral repairs, Given and Rubin (11) reported a contralateral occurrence rate of 6.8%, with subsequent occurrence of a right hernia in 9.6% of patients and left hernia in 5.4%. This study may be somewhat flawed in that the mean delay between hernia repairs was 26.8 months and the follow-up period of the study patients was only 9 to 32 months.
Several series of unilateral repairs have also reported low rates of development of contralateral hernias, although the accuracy of follow-up is questionable. The occurrence rates of a contralateral hernia were 5.8% in Kobe, Japan, (12) 3.7% in Jakarta, Indonesia, (13) and 2% in Karachi, Pakistan (14). These investigators found no significant prediction for occurrence based on the original side or gender.
In an attempt to focus on infants, Surana and Puri (15) reviewed infants between 1 week and 6 months of age (excluding premature infants who underwent bilateral exploration) undergoing unilateral repair. Ten percent of those with long-term follow-up (5 to 17 years) had contralateral hernias. Of those with initial right hernias, left hernias developed in 8.7%; of those with initial left hernias, right hernias developed in 16.6%. Only 1 of 12 girls had a contralateral hernia.
The case for premature infants is less clear, with several of the previously mentioned series including routine bilateral explorations for premature infants younger than 6 months. In a review of 222 very-low-birthweight (less than 1,500 g) neonates with hernias, 61% had bilateral presentation (16). Many researchers reporting on premature infants have observed bilateral rates exceeding 80%, but many consider a patent processus vaginalis equivalent to a hernia (4,17,18). Misra and associates, (19) in a follow-up study of 251 infants younger than 6 months who underwent unilateral repair, observed that contralateral hernias developed in 8%. Only 13% of the premature infants in this group experienced contralateral hernias. In general, these studies appear to draw into question the routine bilateral management of premature and young infants.
The issue of young girls with hernias is also controversial. In one study of 117 girls with hernias, the rates of significant contralateral sacs (more than 1 cm) was 60% for patients younger than 1 year, 28% for patients 1 to 7 years of age, and 33% for patients older than 7 years (20). Although these rates are similar to those for boys, the rate of contralateral hernia occurrence is unknown in girls compared with boys or with advancing age among girls. Several studies have reported a similar 2:1 ratio for right-sided and left-sided hernias, but a more even distribution of hernias in older girls than in older boys (20,21). In addition, if unilateral repairs are performed, the contralateral hernia rate is between 8% and 25% and appears unrelated to age or the original side of repair (20,21).
The basic question remains: How many infants and children have a CPPV, and what percentage of these have a subsequent hernia? The initial data by Rowe and colleagues (9) of contralateral patency rates of 63% in infants younger than 2 months decreasing to 40% after 2 years of age appear secure, with subsequent hernias developing in about 25% to 50% of these patients, although this latter point is perhaps the area of most controversy. Another factor rarely discussed is the actual size of the CPPV and the relationship of this size to the risk of subsequent development of a hernia. Schier et al. (22), in a laparoscopic (three-port) approach, identified wide open CPPV in 26% of boys and 11% of girls presenting with initial right hernia and wide open CPPV in 30% of boys and 38% of girls presenting with left hernias. In all four groups, small (undefined size or depth) CPPV were noted in 15% to 20%. This later group of small CPPVs may be recorded as true CPPV in many open and laparoscopic series.
The pediatric surgeon is then left with three options: (1) never exploring the contralateral side, (2) exploring up to a certain age (e.g., premature infants, 6 months, 1 or 2 years), or (3) attempting to determine contralateral patency and thus avoid negative explorations. If the other side is to be explored, it may be more reasonable to operate on the clinically uninvolved right sides more often or to an older age than the uninvolved left sides owing to the 2:1 ratio for occurrences of contralateral right hernias compared with left hernias. If a reliable and safe method were available to
determine patency, negative contralateral explorations could be eliminated; however, even with this approach, at least two contralateral repairs would be performed to prevent one clinical hernia. Many authors therefore recommend avoiding contralateral exploration (23). A relatively recent prospective study followed 656 infants, children, and adolescents with unilateral inguinal hernias after unilateral repair only, without consideration of age, gestational age, or gender (24). At a mean follow-up of 25.5 months, they noted development of metachronous contralateral hernias in 8.8 months at a median interval of 6 months (range 4 days to 7 years) with the rate of 12.4% in infants less than 6 months of age, 14.8% in premature infants, 10.6% in infants less than 2 years of age, and 27.6% in children with an incarcerated hernia.
determine patency, negative contralateral explorations could be eliminated; however, even with this approach, at least two contralateral repairs would be performed to prevent one clinical hernia. Many authors therefore recommend avoiding contralateral exploration (23). A relatively recent prospective study followed 656 infants, children, and adolescents with unilateral inguinal hernias after unilateral repair only, without consideration of age, gestational age, or gender (24). At a mean follow-up of 25.5 months, they noted development of metachronous contralateral hernias in 8.8 months at a median interval of 6 months (range 4 days to 7 years) with the rate of 12.4% in infants less than 6 months of age, 14.8% in premature infants, 10.6% in infants less than 2 years of age, and 27.6% in children with an incarcerated hernia.
Several methods have been used in an attempt to avoid negative contralateral explorations. The use of a Bakes dilator through the hernia sac to evaluate the contralateral side has been advocated (25), but has been difficult and unreliable in other reports (26). Herniography has also been used, but has disadvantages, including pain with injection, radiation, and time and cost of a radiologist. As a result, this technique has not been widely accepted. Pneumoperitoneum has also been used. In a series of 64 children, only 5 (8%) had CPPV, although one later developed a contralateral hernia (27). This technique was shown to be unreliable for determining patency of the processus vaginalis in a study using pneumoperitoneum followed by laparoscopy (28). The use of ultrasound to detect a CPPV was reported to have an accuracy of 91% in one early report (29). Chen et al. (30) more recently noted an accuracy of 97.9% using a measurement of 4 mm at the internal ring as the upper limit of normal.
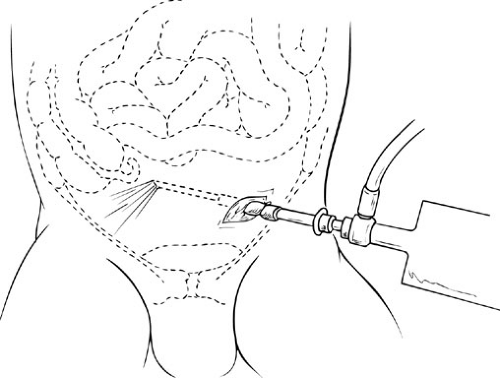 FIGURE 68-3. Nonpuncture laparoscopy. A 70-degree oblique, 4-mm diameter telescope through a 5-mm nondisposable cannula is used to visualize the contralateral internal inguinal ring. |
The introduction of laparoscopy into pediatric surgery has allowed diagnostic visualization of the opposite side. Several reports have documented initial diagnostic laparoscopy in children presenting with unilateral hernias (28,31,32). The incidence of CPPV detected by this method ranges from 30% to 53%, again consistent with previous reports on intraoperative patency determinations. Of interest, several reports have noted that the incidence of patent processus vaginalis does not decrease with advancing age during the first 5 years of life (28,31). Another approach that is currently widely used is to evaluate the other side by passing a 30- or 70-degree oblique scope through the open hernia sac. A meta-analysis of 964 laparoscopic evaluations identified a sensitivity of 99.4% and specificity of 99.5% (33). In these reports, the average additional time was 6 minutes. This technique appears attractive in that it may avoid negative contralateral exploration in cases in which it would be routinely performed by the surgeon. It appears to have little advantage in older children who would normally undergo unilateral repair only. If performed in the latter setting, laparoscopy may actually lead to an increased rate of contralateral exploration, although it should reliably eliminate the occurrence of any subsequent indirect inguinal hernias.
From the preceding discussion, it is clear that this topic remains controversial. My preferred method in boys younger than 2 years old and girls younger than 5 or 6 years old who present with unilateral hernias is to examine the contralateral side by passing a 70-degree angled scope through the open hernia sac (Fig. 68-3). To minimize cost, this should be performed with nondisposable materials. The bladder is emptied with a Crede’s maneuver before the procedure. A 5-mm reusable trocar is passed under
direct vision through the open hernia sac into the peritoneal cavity. A silk tie is passed around the sac and trocar above the level of the internal ring and secured to maintain the pneumoperitoneum. After low-pressure insufflation, the 70-degree angled telescope is passed through the trocar and the contralateral side examined (Fig. 68-4). If a CPPV is identified, contralateral exploration is performed. Because of the angle of approach, it is not always possible to determine the length of the patent processus vaginalis. In cases that are inconclusive due to inability to determine the depth of a small defect or to rule out a veil of peritoneum obscuring a patent processus, a probe may be passed through a 14-gauge angiocatheter to directly measure the length (34).
direct vision through the open hernia sac into the peritoneal cavity. A silk tie is passed around the sac and trocar above the level of the internal ring and secured to maintain the pneumoperitoneum. After low-pressure insufflation, the 70-degree angled telescope is passed through the trocar and the contralateral side examined (Fig. 68-4). If a CPPV is identified, contralateral exploration is performed. Because of the angle of approach, it is not always possible to determine the length of the patent processus vaginalis. In cases that are inconclusive due to inability to determine the depth of a small defect or to rule out a veil of peritoneum obscuring a patent processus, a probe may be passed through a 14-gauge angiocatheter to directly measure the length (34).
Operative Management
The operative procedure for repair of an indirect inguinal hernia involves high ligation of the hernia sac at the level of the internal ring. A transverse incision is placed in the lowest inguinal crease. Scarpa fascia is incised and the external oblique fascia identified. Dissection is continued laterally just above the external oblique to the inguinal ligament, which is then followed inferiorly to expose the external inguinal ring. The external oblique fascia is opened in the direction of its fibers, taking care to avoid injury to the ilioinguinal nerve. Some surgeons prefer to perform the repair in young infants without opening the external oblique (Mitchell-Banks technique) (35). The rationale for this modification is based on the proximity of the external and internal inguinal rings in neonates. The cremaster muscle fibers are gently dissected in a direction perpendicular to the axis of the cord structures. This exposes the hernia sac on the anteromedial surface of the cord. The sac is gently elevated, and the spermatic vessels and vas deferens are separated from the sac. When the sac is free, it is divided between clamps. The proximal sac is gently elevated and the cord structures dissected free to the level of the internal ring where the sac is ligated. The distal sac is examined and, if short, may be left in place. If the sac extends into the scrotum, the anterior aspect can be excised. Levitt et al. (5) found that 78% of pediatric surgeons leave the distal sac alone, other than to drain fluid. If a hydrocele is present, it should also be excised, taking care to avoid injury to the testes and epididymis. In addition, the testes should not be separated from the scrotal attachments. If the testis is undescended or retractile and will not remain in the scrotum, an orchiopexy is performed. The external oblique is then closed. Local anesthetic can be placed in the area of the ilioinguinal nerve and in the subcutaneous tissue to provide postoperative pain relief. The remaining layers are closed, and a collodion topical dressing is placed over the wound in infants. A standard dressing is used for older children.
This procedure is adequate for nearly all indirect inguinal hernias. Occasionally, particularly in neonates with large hernias, the internal ring appears excessively dilated. In these cases, the internal ring can be closed along its medial aspect, below the cord structures. Another approach in the neonate with a difficult hernia is to use a technique of direct closure of the hernia sac through the open sac at the level of the internal ring (36). The suture includes
peritoneum and, where available, muscle surrounding the internal ring taking care to avoid injury to the vas deferens and cord vessels.
peritoneum and, where available, muscle surrounding the internal ring taking care to avoid injury to the vas deferens and cord vessels.
In girls, the initial exposure is identical. The hernia sac and round ligament are dissected free, and the distal attachments are divided. The sac is then mobilized to the level of the internal ring. The fallopian tube is frequently within the wall of the hernia sac as a sliding hernia (Fig. 68-5). This can occasionally be identified by looking through the sac to ensure the ligature is placed distal to the fallopian tube. I prefer to open the sac, gently pull on the round ligament until the fallopian tube is identified, and if a slider is not present, simply ligate the sac. The internal ring is closed, and the remainder of the closure is identical to that in boys. A survey of pediatric surgeons noted that 41% of surgeons tighten the internal ring in girls (5). If a slider of the fallopian tube is present, the sac can be ligated distal to the fallopian tube, divided, and invaginated into the peritoneal cavity, with closure of the internal ring. Another method, described by Goldstein and Potts (21), involves incising the sac along the borders of the fallopian tube to the level of the internal ring. A pursestring suture is then placed in the remainder of the sac at the level of the internal ring. The tube with the attached portion of the sac is then placed into the peritoneal cavity, the suture is tied, and the internal ring is closed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree