Hand
Christine J. Cheng
Department of Surgery, Division of Plastic and Reconstructive Surgery, Washington University School of Medicine, St. Louis Children’s Hospital, St. Louis, Missouri 63110.
Hand surgery is a specialized field that embodies the concept of “regional” surgery, uniquely combining orthopedic, neurosurgical, and plastic surgical techniques in the functional and sometimes aesthetic restoration of a remarkably complex organ. Care of the pediatric hand is complicated by the additional factors of growth and psychomotor and social development. Those who care for children’s hands must be equipped to deal with issues specific to their young patients, which always include counseling and support to their parents, care providers, and families.
EMBRYOLOGY AND ANATOMY
The Growing Hand
The embryonic upper extremity starts as a limb bud that develops from proximally to distally around day 26 of gestation (1). The hand first forms as a plate. The digital rays separate by apoptosis of their intervening cells by day 36. A well-differentiated hand exists by 7 weeks, which does not undergo further differentiation after about the 50th day. Early studies of chick embryos led to the discovery of growth centers that specifically govern upper extremity development, which all have counterparts in the human hand (2). Cells within the apical ectodermal ridge produce fibroblast growth factors that direct proximal-to-distal growth: sonic hedgehog protein, secreted by cells within the zone of polarizing activity, has been found to define the radioulnar axis; Wnt-7a protein is associated with establishment of the dorsal-ventral axis (1,2). The cartilaginous skeleton undergoes enchondral ossification of its primary centers between the seventh and tenth weeks of gestation. The carpus does not begin to ossify until around 1 year of age. Secondary ossification varies according to gender and race, with frequent delays in congenitally abnormal hands (3).
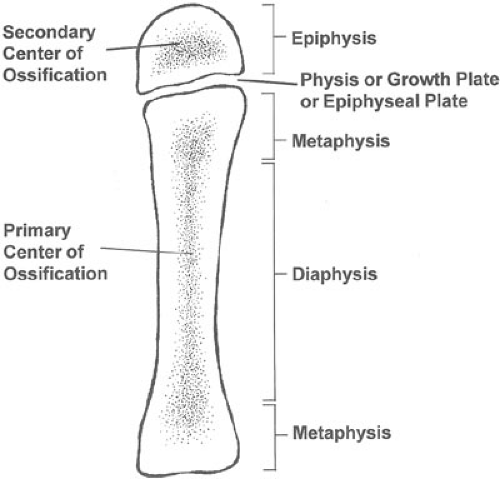
The four distinct physiologic regions of pediatric bone (Fig. 106-1)—epiphysis, physis, metaphysis, and diaphysis—are not only responsible for their growth, but also account for different patterns of injury and responses to treatment, compared with adults. The epiphyses are located at the ends of the long bones, which are covered by articular cartilage at skeletal maturity. The physis, or growth plate, produces rapid longitudinal and latitudinal growth. Vascular compromise to this region halts cell division, resulting in longitudinal deformity if the entire physis is affected, and angular deformity if only a portion is injured. The physis, which appears as a lucent line on plain X-rays, may temporarily widen in response to injury of its adjacent region. The metaphysis forms the contoured flare at either end of the bony shaft, or diaphysis. Metaphyseal bone has a thinner and more fenestrated cortex in children, making torus or buckle fractures more likely. The diaphysis comprises the major portion of each long bone, and is more vascular and less dense in younger children. As the skeleton matures, the number of Haversian systems increases and this region becomes more solid. Thus, fracture patterns change and fracture healing slows with increasing age. In children, the periosteum is thicker, with more osteogenic potential, making fractures less likely to displace, as well as keeping them more stably reduced (4).
Functional Development and Physical Examination
Functional assessment must take into account the anatomic structures and sensory capabilities of the hand, as well as the chronological and developmental age of the child. For the first month, infants tend to hold their fists tightly clenched, opening only during reflexive actions such as startling or stretching. At 3 months of age, they begin to grasp with only their fingers, usually with the wrist flexed. Grasp does not involve the thumb until 6 to 7 months of age, and true thumb use for pinch and manipulation of smaller objects does not begin until a child is
around 10 months old (3). Adequate physical examination, as well as the necessity and timing for surgical intervention, are influenced by these developmental patterns.
around 10 months old (3). Adequate physical examination, as well as the necessity and timing for surgical intervention, are influenced by these developmental patterns.
Examination begins with observing whether the child places the hand purposefully in space, inspecting the relative length of the upper extremity and the size of the hand, and checking joint motion and stability. Digital motion in utero produces finger flexion creases, so the absence of these creases at birth suggests either the lack of a functioning joint or inadequate musculotendinous structures. Similarly, abnormal progression in functional development or patterns of use can reflect abnormal neurosensory or musculoskeletal conditions. Pain may be displayed by the refusal to use an affected limb, whereas anesthesia can present as an unusual wound or even self-biting. Because younger children are incapable of following commands and verbalizing answers during physical examination, adequate assessment may require multiple visits to establish the full clinical picture. Comparison to the opposite extremity is often helpful.
CONGENITAL HAND DIFFERENCES
Classification
Systems of classification allow a common language for communication and enable comparisons to be made between groups. Unfortunately, the spectrum of congenital hand differences is vast, with a nearly infinite number of unique variations. Thus, a comprehensive system of congenital hand conditions that adequately classifies all malformations is difficult to devise. An excessively generalized system is not useful, whereas an extremely detailed one becomes unwieldy and impractical. The most commonly employed classification has been that introduced by the International Federation of Surgical Societies of the Hand (5), which avoids Greek and Latin terms, does not include eponyms, and uses simple descriptive terminology. With this system, hand malformations are classified into seven major groups:
Failure of formation of parts
Failure of differentiation of parts
Duplication
Overgrowth
Undergrowth
Congenital constriction ring syndrome
Generalized skeletal abnormalities
Shortcomings of this system are revealed when attempting to classify hands that have more than one abnormality or in which the etiology is not clearly established.
Prevalence and Etiology
Although the hand is a visible organ, some congenital differences are subtle and can be missed upon initial inspection of an infant at birth. Missed diagnoses make it difficult or even impossible to establish the true incidence of congenital hand differences. Estimates among different populations estimate the prevalence to be as high as 1 in 500 to 600 live births (1,6). In descending order of frequency, the most common major congenital upper limb malformations are syndactyly, polydactyly, congenital amputation, and radial-sided defects. Although the relative frequencies of the two most common conditions, syndactyly and polydactyly, have varied between populations, they consistently comprise 20% to 50% of all reported diagnoses.
Increased understanding of the molecular biology of limb development has already identified the genetic basis for many congenital hand conditions (1). Some of these involve single gene mutations, such as in Apert syndactyly, whereas others are associated with chromosomal abnormalities (e.g., trisomy 13). At the cellular level, a variety of mechanistic pathways are involved, including transcription factors, cell signaling pathways, and growth factors. Teratogen exposure and in utero events such as limb constriction by fetal membranes have also been implicated as causative factors, although more recent theories suggest that interruption of fetal vascular circulation may be the underlying mechanism common to these (7).
In the developing fetus, hand formation coincides temporally with development of the cardiac and renal systems, so careful evaluation of these organ systems is indicated
in an infant born with a congenital hand abnormality. Involvement of multiple limbs and multiple organ systems can suggest a congenital syndrome, with potentially serious consequences. For example, radial club hand is associated with Fanconi anemia and thrombocytopenia-absent radius syndrome, both of which involve life-threatening hematologic defects. Ulnar polydactyly, which is commonly an isolated genetic trait in African Americans, is more likely to be part of a syndrome in Caucasians (8). When a syndrome is suspected, referral to a geneticist is recommended for parental counseling on heritability, including the likelihood of subsequent offspring and the patient’s children having the same condition.
in an infant born with a congenital hand abnormality. Involvement of multiple limbs and multiple organ systems can suggest a congenital syndrome, with potentially serious consequences. For example, radial club hand is associated with Fanconi anemia and thrombocytopenia-absent radius syndrome, both of which involve life-threatening hematologic defects. Ulnar polydactyly, which is commonly an isolated genetic trait in African Americans, is more likely to be part of a syndrome in Caucasians (8). When a syndrome is suspected, referral to a geneticist is recommended for parental counseling on heritability, including the likelihood of subsequent offspring and the patient’s children having the same condition.
Treatment Indications and Timing
The functional goals of treatment are to provide a hand that can be properly positioned, has good sensation, and is able to achieve both power grasp and precision pinch. A normal-appearing hand is optimal, but cannot always be attained. Surgical correction of congenital hand differences can usually be postponed until conditions for general anesthesia, such as age, weight, and hemoglobin levels, are optimized. Most congenital hand differences should be corrected by or shortly after 1 year of age, when the child truly begins to use the hand as an instrument for exploring his or her environment, self-feeding, and nonverbal communication. Conditions that cause joint contracture, or angulation or rotational deformity due to tethering of adjacent digits, such as in acrosyndactyly where the fingertips are fused or syndactyly of the border digits (thumb-index, ring-small) should be corrected as early as 6 months of age to avoid permanent skeletal changes. Of course, emergent correction is warranted when the circulation to a digit or limb is at risk, such as with severe constriction rings. The decision of when to operate involves a balance between minimizing anesthetic risk, preventing the disturbance of psychomotor development, and reducing surgical complications because neurovascular structures in an older child are larger and easier to handle.
Syndactyly
Syndactyly, or fused digits, is one of the most common congenital hand defects, occurring in about 1 of every 2,000 births. It is twice as common in males, ten times more common in Caucasians, and involves one or both hands with equal frequency. Ten to 40% of cases have a positive family history, with the condition always inherited as an autosomal dominant trait, although penetrance and expressivity can vary (3). Long-ring finger syndactyly is the most common. Fusion of the thumb and index fingers is the most rare. The mechanism is believed to be a failure of the normal digital separation in the embryonic hand and can involve only the soft tissues (simple syndactyly) or can include the phalanges and nails (complex syndactyly). The webbing is further classified as complete when it extends the entire length of the digits and incomplete when it does not. Syndactyly is commonly associated with congenital syndromes, such as Poland syndrome, which can include chest hypoplasia, and Apert syndrome, which has associated characteristic craniofacial features.
Surgical correction of syndactyly is recommended in all cases to restore independent motion and normal span of the fingers, allowing the proper use of instruments and equipment such as gloves. Separation of border digits (thumb-index, ring-small) is recommended as early as 6 months of age to avoid permanent skeletal deformity due to unequal length between the fused fingers. Syndactyly of the central fingers (index-long, long-ring) can be postponed, although most surgeons recommend correction prior to school age, to save the child from social stigmatization.
The variously described techniques for syndactyly separation all incorporate a few basic principles. A local skin flap, usually dorsal, is used to form the new web, alternating volar and dorsal flaps resurface the fingers, skin grafts cover any remaining defects, and only one side of any digit is released at a time (3). Correction of a web that reaches up to and beyond the proximal interphalangeal (PIP) joint will require skin grafting (Fig. 106-2). Grafts are taken from future non–hair-bearing areas such as the lateral inguinal area, with full-thickness skin grafts less likely to contract than split-thickness ones. Unfortunately, skin grafts tend to become darker than the surrounding skin, especially in dark-skinned individuals. Limiting dissection to only one side of each digit at a time avoids the chance of neurovascular compromise, especially if there is abnormal vascular anatomy. Thus, multiply fused digits require staged correction. Incomplete syndactyly may be corrected with local transposition flaps alone, if the web is shallow. In complex syndactyly, the bony elements and nails are also separated, with joint abnormalities being more common in complicated cases such as seen with Apert syndrome. Long-term follow-up is important, as recurrent webbing or “web creep” with growth can occur, which usually requires minor local flap revision.
Polydactyly
Polydactyly, or extra digits, is the other most frequently occurring congenital hand abnormality. Its incidence is estimated to be at least 1 in 1,000 live births (9). The real incidence may be higher because cases treated with suture ligation in the newborn nursery may not be reported and families of infants with milder forms may not seek treatment (8). The thumb is most commonly duplicated in Caucasians and Asians, occurring in 1 out of every 3,000 live births, whereas African Americans are more likely to have duplication of the small finger, with an incidence of
10 per 1,000 (9). Polydactyly is described as radial, central, or ulnar according to the location of the duplicated digit. This is preferred over the old terminology of preaxial and postaxial because controversy exists over where the true axis of the hand lies (9). In addition to the position of the extra digit, its degree of development is further classified. For ulnar polydactyly, Stelling (10) and Turek (11) describe three types: type I is a functionless cutaneous appendage, type II is partial duplication, and type III is complete duplication. Based on a study of pedigrees, Tentamy and McKusick (12) divided them into two types: Type A is a well-formed digit that articulates with the adjacent metacarpal, and Type B is small and poorly developed. Wassel’s classification of thumb polydactyly describes the level and completeness of duplication (13). Although the precise mechanism is unknown, ectodermal overgrowth has been observed in experimental animal models and human embryos that developed radial polydactyly (14,15). Thumb polydactyly is rarely associated with a syndrome. Ulnar polydactyly is frequently an autosomal-dominant trait in African Americans, but in Caucasians it is more likely to be associated with one of more than 40 syndromes (8).
10 per 1,000 (9). Polydactyly is described as radial, central, or ulnar according to the location of the duplicated digit. This is preferred over the old terminology of preaxial and postaxial because controversy exists over where the true axis of the hand lies (9). In addition to the position of the extra digit, its degree of development is further classified. For ulnar polydactyly, Stelling (10) and Turek (11) describe three types: type I is a functionless cutaneous appendage, type II is partial duplication, and type III is complete duplication. Based on a study of pedigrees, Tentamy and McKusick (12) divided them into two types: Type A is a well-formed digit that articulates with the adjacent metacarpal, and Type B is small and poorly developed. Wassel’s classification of thumb polydactyly describes the level and completeness of duplication (13). Although the precise mechanism is unknown, ectodermal overgrowth has been observed in experimental animal models and human embryos that developed radial polydactyly (14,15). Thumb polydactyly is rarely associated with a syndrome. Ulnar polydactyly is frequently an autosomal-dominant trait in African Americans, but in Caucasians it is more likely to be associated with one of more than 40 syndromes (8).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree