General Wound Management
James M. Callahan
M. Douglas Baker
Introduction
Traumatic injuries are commonly encountered in pediatric patients. Ten million patients present to emergency departments (EDs) in the United States each year for treatment of traumatic wounds (1). A significant percentage of these patients are children. The goals of therapy in dealing with cutaneous wounds include restoration of function and structural integrity, prevention of infection, and production of cosmetically acceptable healing. These goals are interrelated, and adherence to sound principles of general wound management will lead to achieving them.
Effective wound management can be initiated by either emergency medical services (EMS) personnel or parents at the scene of an injury and is continued by nursing and medical personnel in the ED. The aim of therapy is to prevent secondary tissue damage or the development of infection so that the wound can heal primarily. Adequate preparation of equipment and a well-established treatment plan are among the keys to success.
General surgical principles, including adherence to standard aseptic techniques (Chapter 7), apply to all traumatic wounds. Appropriate restraint (Chapter 3) and anesthesia, sedation, and pain control (Chapters 33 to 35) will lead to improved outcomes. Preparation of the wound is an important prelude to actual wound closure, which is discussed in Chapters 108 and 109.
Anatomy and Physiology
A working knowledge of both skin biomechanics and the mechanisms of soft-tissue trauma is necessary to manage wounds effectively. In addition, many factors can modify the overall effect and outcome of a particular injury in a given patient. Knowledge of these factors also is important.
The skin is remarkably resistant to traumatic forces (2) and is highly elastic due to its high content of elastin fibers. It also has a large number of collagen fibers, which give it added strength (2). A significant amount of force is required to cause tissue disruption.
The skin is constantly under static and dynamic tension. Static tension is caused by the force exerted on the skin by the underlying tissues at rest and the natural tension of the skin itself (3). Dynamic tension is caused by joint movement, muscle contraction, and gravity (3). Wounds under a large amount of tension tend to heal with wide, unattractive scars (3). Wound edges that retract more than 5 mm are thought to be under strong static tension (4). Wounds under low tension (edge retraction less than 5 mm) tend to heal with minimal scars. Wounds that cross joints or are perpendicular to wrinkle lines often lead to unattractive scars regardless of the repairer’s skill (4). Patients and their families should be warned about these issues before repairs are made.
The skin is inhabited by micro-organisms, which can be a source of endogenous infection when trauma causes tissue
disruption. Most of the bacteria in the skin reside in the horny layer of dead skin cells, which are in the process of being sloughed off. The stratum corneum below this layer is composed of tightly packed, viable cells that act as a barrier to bacteria (1). Exogenous sources of bacteria also can lead to wound infections.
disruption. Most of the bacteria in the skin reside in the horny layer of dead skin cells, which are in the process of being sloughed off. The stratum corneum below this layer is composed of tightly packed, viable cells that act as a barrier to bacteria (1). Exogenous sources of bacteria also can lead to wound infections.
The amount of bacteria present on the skin varies by anatomic location. Three distinct zones are characterized by the density of residing microorganisms (1). Moist areas (i.e., axillae, perineum, web spaces, and intertriginous areas) have extremely high bacterial concentrations and therefore are prone to infection when disrupted traumatically. Dry areas (i.e., back, chest, abdomen, arms, and legs) have low bacterial concentrations. Exposed areas (i.e., face, head, hands, and feet) have high bacterial concentrations, with the exception of the palms and dorsal surfaces of the hand where concentrations are low (1). Lacerations caused by contact with the oral cavity, especially the teeth (i.e., bite wounds), are highly contaminated and particularly prone to infection. Wounds that contact vaginal secretions or feces also will usually become infected.
It is important to consider the mechanism of injury in the management of soft-tissue trauma. Wounds are caused by mechanical or thermal forces (Chapter 113). Mechanical forces are of three types: shearing, tension, and compression (2).
Shearing occurs when forces of equal magnitude are applied to the skin in opposite directions along parallel planes (Fig. 107.1A) (2). A cut caused by an object with a sharp edge (e.g., a knife or glass) is an example of a shearing force. Little energy is transmitted to surrounding tissues, and therefore little devitalization of adjacent areas is seen. These wounds have a low potential for infection. Low-velocity missiles (e.g., .22-caliber rimfire bullets and bullets from handguns other than the .44 magnum pistol) usually cause a shear and compression injury that is confined to the actual missile tract (1). Direct injuries to internal organs or major vessels account for the morbidity and mortality associated with these wounds.
High-velocity missiles (including rifled slugs from a shotgun at a range of less than 45 meters) cause not only a shearing injury along the wound tract but also devitalization of adjacent tissues secondary to compression and the entrainment of large amounts of skin bacteria and debris. These wounds are highly prone to infection. They should be managed by extensive and repeated débridement of the wound in the operating room to remove devitalized tissue (1).
Tension injuries occur when the skin is struck with a blunt or semiblunt object at an angle of less than 90 degrees (Fig. 107.1B). Avulsion injuries and flap lacerations are common (2). Usually these injuries are associated with a larger force applied to the skin than is seen with shearing injuries. Devitalized tissue is more often seen adjacent to the wound. In addition, the vascular supply to a flap may be compromised, leading to necrosis. Tension wounds are more difficult to repair and more prone to infection.
Compression injuries, usually caused by blunt trauma directed at an angle of 90 degrees against skin that often overlies bones, cause the most tissue disruption (Fig. 107.1C) (2). Stellate lacerations with adjacent hematomas and abrasions are commonly seen. Large areas of devitalized tissue can result, and infection rates 100 times higher than those seen with shearing injuries have been reported (1).
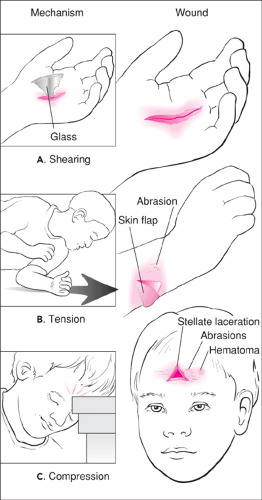 Figure 107.1 Common mechanisms of injury and resulting wounds. A. Shearing injury. B. Tension injury. C. Compression injury. |
Tissue damage caused by an object is directly related to the amount of kinetic energy the object transmits to the tissues involved. The kinetic energy of an object is described by the equation
KE = 1/2 mv
where m equals the mass of the object and v equals the object’s velocity. Increasing the velocity, therefore, has a greater
impact on the amount of tissue damage caused than increasing the mass of the object. Whether the material reacts with the biologic tissue or is relatively inert will determine if it will potentiate the development of infection. The configuration or shape of the object also will determine the nature of the wound it causes (2).
impact on the amount of tissue damage caused than increasing the mass of the object. Whether the material reacts with the biologic tissue or is relatively inert will determine if it will potentiate the development of infection. The configuration or shape of the object also will determine the nature of the wound it causes (2).
The environment in which the wounding event occurs will greatly modify the nature of the wound. Swamps, marshes, and other wet environments tend to have high bacterial loads. Wounds occurring on farms may be contaminated by animal feces. Further, soil and dirt have been shown to inhibit the infection-fighting capabilities of both the cellular and humoral immune systems (1). Organic components and inorganic clay components of soil inhibit white blood cell phagocytic and killing mechanisms and the bactericidal nature of human serum (1,5,6,7). These same elements also inactivate many antibiotics (8). Soil from swamps and similar areas have a high proportion of organic materials. Sand, a large-grained, inert component of soil, and the black dirt found on the surface of highways do not seem to have the same inhibitory effects (1).
Finally, characteristics of the patient will influence both the type of wound caused by a particular insult and the healing process. Patient age, general health, and intercurrent illnesses or medication can affect skin integrity and the processes involved in wound healing. Malnutrition, shock states, severe anemia, and uremia lead to delayed healing and increased infection rates (2). Chronic use of steroids can cause thinning of the skin analogous to the aging process, leading to large, shallow avulsions or flap injuries (2). These drugs can also impair healing mechanisms and increase infection rates.
The mechanism of injury, the characteristics of the wounding object, the environment in which the wound was sustained, and the health status of the patient are important to consider in the approach to general wound management. Developing an appropriate treatment plan based on the characteristics of the wound and the patient will improve the outcome. Characteristics that lead to increased areas of devitalization, delayed healing, or increased infection rates require specialized approaches to wound management.
Indications
All wounds will benefit from some management. The clinician must determine the level of care necessary for the particular injury. Local cleansing and irrigation is important in almost all wounds, whereas additional interventions must be considered frequently but are only indicated in specific situations. Absolute contraindications to wound closure are few in number and include the presence of signs and symptoms of secondary bacterial infection, evidence of primary healing, and lack of cosmetic or functional need for closure.
Certain situations indicate the need for the removal of a foreign body within a wound (Chapter 111). In general, objects that are easily seen and grasped, objects likely to cause intense inflammation, objects in close proximity to vital structures, and objects detected due to the development of a soft-tissue infection should be removed (9). Relatively inert foreign bodies that cause little tissue reaction and are not threatening because of their position or potential for migration may be left in place, especially if exploration would lead to further tissue damage (2,10). Other foreign bodies, especially those that are organic in nature, cause an intense tissue reaction and inflammation, which impairs the wound’s ability to resist infection. These types of foreign bodies (e.g., wood, thorns, cactus spines, fabrics, devitalized skin, rooster spurs) must be diligently sought and removed or devastating infections may result (9,11,12). Metals vary in the amount of tissue reaction and inflammation they cause, which depends on their ability to be oxidized. Sometimes elusive foreign bodies may be more easily located and removed once they are encapsulated by scar tissue.
In grossly contaminated wounds and wounds with a large amount of devitalized tissue, débridement can decrease wound infections and complications by removing bacteria, debris, and devitalized tissue (see also discussion in Chapter 108). Devitalized tissue has been shown to impair the wound’s ability to resist infection by acting as a culture medium that promotes bacterial growth, by inhibiting phagocytosis by leukocytes, and by limiting other leukocyte functions through the development of an anaerobic environment (13). Devitalized skin, fat, and muscle have been shown to cause comparable amounts of infection.
It is important to use débridement only when it is necessary, so as to not “make the wound your wound.” Jagged-edged, uneven wounds have a much longer wound edge than straight lacerations. Jagged-edged wounds, if closed carefully, have a decreased amount of tension per unit length of wound edge and lead to better wound edge approximation (1). Converting such wounds to straight-edged wounds by débridement of skin and underlying tissue increases the amount of tension required to keep the wound edges approximated and therefore the width of the scar (1). Débridement of facial fat should be avoided, as unsightly depressions may result at the site of repair.
Fluid in a wound cavity, whether blood, pus, or serous fluid, will damage the defense mechanisms of the wound and lead to an increased risk of infection. Drains can be used to evacuate these fluids and improve healing. Drains should not be used prophylactically, however, as they actually may increase infection rates by damaging wound resistance to infection and permitting retrograde contamination of the wound by surface bacteria (14).
Wounds particularly prone to infection should be considered for delayed closure, as detailed in Chapter 108. These include markedly contaminated wounds, wounds with purulent material already present, wounds more than 12 to 19 hours old, missile wounds, wounds secondary to severe crush injury, wounds caused by human or animal bites, and wounds that have come into contact with feces, saliva (bites), or vaginal fluids. Such wounds, if cleaned appropriately and managed in an open fashion for 4 to 5 days, will develop a marked resistance
to infection and can undergo delayed closure at that time (15,16). It is important to keep in mind that clinical signs and symptoms of secondary bacterial infection are not clinically evident until at least 12 hours following contamination with pathogens (17).
to infection and can undergo delayed closure at that time (15,16). It is important to keep in mind that clinical signs and symptoms of secondary bacterial infection are not clinically evident until at least 12 hours following contamination with pathogens (17).
TABLE 107.1 Tetanus-Prone Wounds | |
|---|---|
|
All wounds carry the risk of tetanus as a potential complication. Contaminated wounds (especially involving soil or feces), wounds with devitalized tissue, and deep puncture wounds are particularly prone to contamination with Clostridium tetani (18). Patients who have not received at least three previous doses of tetanus toxoid or whose primary immunization status is unknown should receive 250 IU of tetanus immune globulin (TIG) intramuscularly if the wound is tetanus prone (Table 107.1). Recommendations for using TIG and tetanus toxoid based on the number of previous doses of toxoid, the type of wound, and the length of time since the last toxoid are provided in Table 107.2.
Increasing numbers of rabies cases have been reported among wild animals in recent years (19,20). Skunks, foxes, raccoons, and bats have a significant prevalence of rabies depending on their geographic location. Transmission of infection to stray and domestic dogs and cats, cattle, and even people has been reported. Bites by known, healthy, provoked domestic pets (dogs and cats) are unlikely to transmit rabies. Bites by unknown or unavailable animals or by skunks, foxes, raccoons, and bats should be treated as if the animal was rabid. Animals that can be observed and remain healthy for 10 days after biting a person could not have transmitted the virus. The virus has been transmitted in an aerosolized fashion in caves inhabited by bats (19,20) and in enclosed rooms within dwellings in which bats have been found. Wounds for which rabies prophylaxis is indicated are listed in Table 107.3.
TABLE 107.2 Tetanus Prophylaxis | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||
TABLE 107.3 Indications for Rabies Prophylaxis | ||
|---|---|---|
|
Wound repair that will require the open reduction of fractures, reanastomosis of vascular structures, or nerve or tendon repair should be taken to the operating room, where more controlled conditions allow for better wound healing (1). Extremely large wounds or wounds requiring extensive repairs in sensitive areas (e.g., wounds in the perineum, wounds in the medial canthus of the eye, extensive intraoral wounds) also should be considered for management in the operating room.
Equipment
Sterile gloves and mask
Manual sphygmomanometer to aid hemostasis
Hair clippers or scissors for scalp wounds
Iodophor- or chlorhexidine-based solution for skin cleansing
Sterile saline solution for irrigation
Syringe, 35 mL for irrigation
Splashshield device for irrigation (may use 19-gauge needle or Angiocath)
High-porosity sponge
Sterile drapes
Gauze sponges
Antibiotic ointment, water-based
Microporous polypropylene dressings
Microporous tape
Cotton-tipped applicators
Needle driver
Scissors and/or scalpel
Forceps and/or skin hooks (may be made from 25-gauge needle and applicators)
Wound closure and anesthetic materials as needed (Chapters 35 and 108)
It is important, especially with pediatric patients, to have all of the equipment ready at the outset. Delays caused by the need to get equipment will only heighten the anxiety of the
child as he or she waits for the procedure to begin. Instruments that may look threatening should be prepared out of the child’s sight. The equipment should be appropriate for the degree of involvement and complexity of the procedure.
child as he or she waits for the procedure to begin. Instruments that may look threatening should be prepared out of the child’s sight. The equipment should be appropriate for the degree of involvement and complexity of the procedure.
Protective equipment for health care personnel is extremely important (Chapter 8). Universal precautions should be followed by all personnel in dealing with wounds. Wound irrigation, hemostasis, and wound closure present opportunities for potentially contaminated blood to come into contact with the skin or mucous membranes of personnel involved in the procedure. A study in an adult ED population showed that 4% of patients who had blood drawn had unrecognized human immunodeficiency virus (HIV) infection. Patients with penetrating trauma had an increased seroprevalence rate independent of other known risk factors (21). Although the seroprevalence rate in children would be expected to be lower, it could approach 4%, depending on the age of the child (adolescents have increased rates) and the local incidence.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


