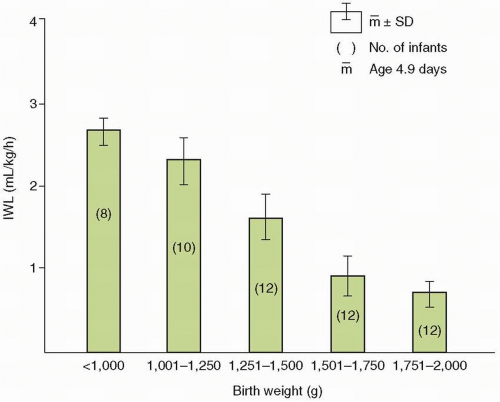
The loss of water by evaporation from the skin and respiratory tract is known as IWL. About 30% of IWL normally occurs through the respiratory tract as moisture in expired gas (
31,
32,
33), with the remaining 70% lost through the skin. IWL depends more on surface area (m
2) than weight, but it is commonly expressed per kilogram (kg) because weight is more easily determined than is area.
IWL is a function of energy expenditure, though a number of additional factors are known to influence IWL in a predictable manner (
Table 19.2) (
31,
32,
33,
34,
35,
36,
37,
38,
39,
40,
41,
42,
43,
44,
45,
46,
47,
48,
49,
50,
51,
52,
53,
54,
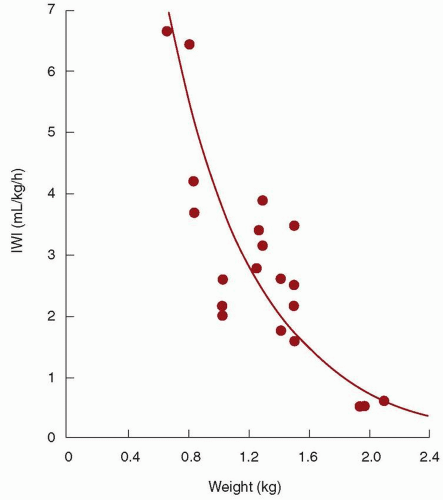
55). When expressed per kilogram of body weight, IWL is inversely proportional to birth weight and gestation age (
Figs. 19.4 and 19.5) (
51,
54). In other words, smaller, more immature infants have larger IWL per kilogram (
Table 19.3). The same is true if IWL is expressed per square meter of body surface (
43). Therefore, although the greater IWL of smaller premature infants is partly due to the increased ratio of surface area (skin and respiratory tract) to body weight, it also is thought to be related to their thinner skin, greater skin blood flow, larger body water per kilogram of body weight, and higher respiratory rate. Because skin permeability to water varies inversely with gestational age, the degree of immaturity is an important determinant of cutaneous IWL independent of birth weight.
Factors That Increase Insensible Water Loss
An increase in minute ventilation, as may occur with cardiac disease, pulmonary dysfunction, or metabolic acidosis, increases the respiratory IWL (
44), as long as the water vapor pressure is less in the inspired than in the expired gas. Preterm infants receiving mechanical ventilation breathing gas mixtures that have been warmed (31.5°C) and humidified (100%) have about a 30% decrease in respiratory IWL compared to nonintubated infants (
32). Environmental temperature above the neutral thermal zone increases IWL in proportion to the increment in temperature (
31,
36,
52). This effect can occur even without a rise in body temperature. In contrast, a subneutral environmental temperature is not associated with reduced IWL, although metabolic heat production is increased (
36). Increased body temperature, whether caused by fever or environmental overheating, elevates IWL (
31,
52).
Skin breakdown or injury disrupts the barrier against cutaneous evaporation and raises IWL. Skin trauma from thermal, chemical, or mechanical injury is common among critically ill, small premature infants. Such injury may result from removal of tape and adherent monitoring devices or from prolonged skin exposure to disinfectant solutions. IWL also is increased in conjunction with the skin manifestations of essential fatty acid deficiency, a potential problem in infants receiving fat-free parenteral nutrition. Congenital skin defects, such as those seen in gastroschisis, omphalocele, and neural tube defects, are associated with increased IWL until surgically corrected.
Use of nonionizing radiant energy, in the form of either a radiant warmer or phototherapy, has been shown to increase IWL by about 50% (
37,
38,
40,
42,
45,
50,
54). For infants in incubators with controlled air temperature, the increase in IWL with overhead phototherapy is most likely a result of increased body temperature because of the warmer incubator walls (
50). For infants in incubators operated to control skin temperature, the rise in IWL with phototherapy can be explained by the lower absolute humidity resulting from the reduced air temperature that accompanies the warming of the incubator walls by the phototherapy. The impact on IWL of phototherapy delivered by fiberoptic blankets or pads is not known but is probably negligible unless the blanket produces a warmer or moister microenvironment around the infant. Investigators using direct measurements of transepidermal and respiratory water loss have obtained conflicting results regarding the effect of overhead phototherapy on IWL. One group (
42) found an increase in transepidermal water loss with phototherapy, but another did not (
56,
57). In contrast to conventional phototherapy, light-emitting diode (LED) phototherapy does not result in changes in transepidermal IWL (
58).
If an infant’s IWL is measured at the same skin temperature under a radiant warmer and in an incubator, the IWL is higher (by about 50%) under the radiant warmer. IWL is higher because absolute humidity (water vapor pressure) is lower under the radiant warmer than in the incubator (
38). This may be true even though relative humidity is higher under the radiant warmer (
37,
38), because the lower air temperature with the radiant warmer means that the saturation pressure of water vapor is considerably lower than in the incubator (
Table 19.4). This finding has been confirmed
using direct measurements of transepidermal water loss (
45). It is now understood that the higher IWL with radiant warmers arises from the lower ambient water vapor pressure and not from higher air velocity or a direct effect of nonionizing radiation on the skin. The same phenomenon explains the effect of phototherapy on IWL of infants in incubators operated by skin temperature servocontrol. The effects on IWL of radiant warmers and phototherapy are additive; the IWL with the combination is approximately twice as large as in an incubator without phototherapy (
37,
40).
Increased motor activity and crying increase IWL by up to 70% (
31,
39,
55). This effect may be partly due to elevated minute ventilation.
Factors That Reduce Insensible Water Loss
Increasing the humidity or water vapor pressure of inspired gas reduces respiratory IWL. The inspired humidity is raised by humidifying the air-oxygen mixture delivered to a head hood or directly to the infant’s upper airway (e.g., via nasal cannula, face mask, or
endotracheal tube) if respiratory support is required. If the temperature and water content of the inspired and expired gas are the same, the respiratory IWL will be entirely eliminated. Increasing ambient humidity, for example in an incubator, reduces total IWL, but respiratory IWL is decreased more than is cutaneous IWL (
31); a threefold increase in ambient water vapor pressure, from an average of 7 to 25 mm Hg, resulted in a 30% reduction in total IWL. Increasing ambient humidity is facilitated by the design of certain recent models of incubators. The use of incubator humidification systems should not be overlooked as a way of reducing IWL and total fluid requirements (
59). Modern incubators allow adjustment of the ambient humidity, which, in turn, affects IWL and water requirement.
Plexiglas heat shields are effective in reducing the IWL of small premature infants in incubators (
38), especially if the ends are at least partially enclosed to decrease air movement near the skin. Plexiglas heat shields are not effective for infants under radiant warmers (
35,
38), because Plexiglas is opaque to the infrared energy produced by the radiant heaters. Thin barriers of saran and other materials reduce IWL of infants under radiant warmers while allowing the infrared heat to reach the skin (
35). These heat shields presumably reduce IWL by limiting air movement and raising water vapor pressure near the infant’s body surface.
Thin plastic blankets have been found to reduce IWL by 30% to 70% for infants under radiant warmers and in incubators (
34,
35,
48). Chambers made of thin plastic material also reduce IWL by a similar amount (
34,
41). Semipermeable membranes (
46,
47) and water-proof topical agents (
49) reduce IWL from the covered areas by an average of approximately 50%.
Knowledge of these factors that affect IWL is essential for estimating the water intake required by newborn infants and for
making appropriate adjustments in water intake with changes in care. Of all infants, premature and critically ill infants are the ones whose IWL is most profoundly influenced by these factors. This is especially true for the extremely premature infant. However, these are exactly the infants for whom precise maintenance of fluid and electrolyte balance is most important and for whom the margin for error is smallest.