● INTRODUCTION
Over the past decade, the widespread adoption of first-trimester risk assessment with nuchal translucency (NT) and other first-trimester ultrasound markers increased interest in early anomaly scan in general and in fetal echocardiography in particular. NT screening allowed for the detection of fetuses with chromosomal abnormalities in the first trimester with associated cardiac defects (1). Furthermore, an enlarged NT is a risk factor for cardiac malformations (1–4).
In the early 1990s, experts reported on the possibility of detection of cardiac anomalies in the late first and early second trimesters of pregnancy (5–9), but this approach was limited to few centers with significant expertise in fetal imaging. The ability to image the fetal heart in early gestation with sufficient clarity to make a diagnosis of a cardiac malformation was made possible by the advent of high-resolution transvaginal and transabdominal transducers (Figs. 16.1 to 16.5). Discrepancy currently exists in the scientific community with regard to the gestational age window, which warrants the term early cardiac examination. Some authors consider a targeted cardiac examination prior to 16 weeks’ gestation as early echocardiography (6, 10), whereas others have established the NT gestational age window of 11+0 to 13+6 weeks for early echocardiography (2, 9, 11). Nevertheless, most practitioners consider a targeted cardiac examination performed in the first and early second trimesters window (11–16 weeks) as early cardiac scan (12).
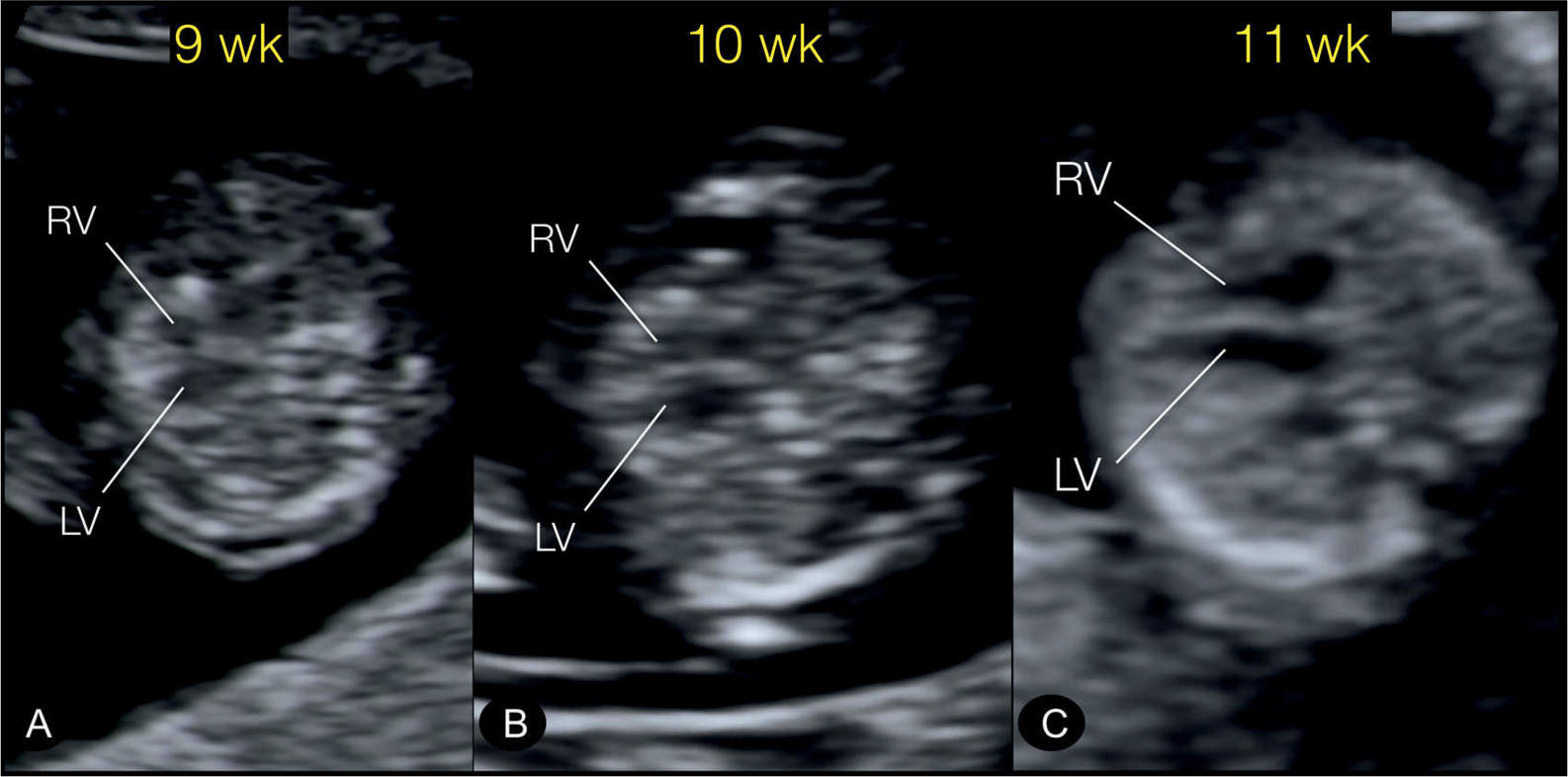
Figure 16.1: Transverse four-chamber views in three normal fetuses at 9+4 (A), 10+3 (B), and 11+2 (C) weeks’ gestation as demonstrated by transvaginal ultrasound. The lumen of right (RV) and left (LV) ventricles separated by the interventricular septum can be clearly identified by the lateral insonation. From 11 weeks’ gestation and beyond (C), the image quality under optimum conditions becomes of such clarity that reliable diagnoses can be expected.
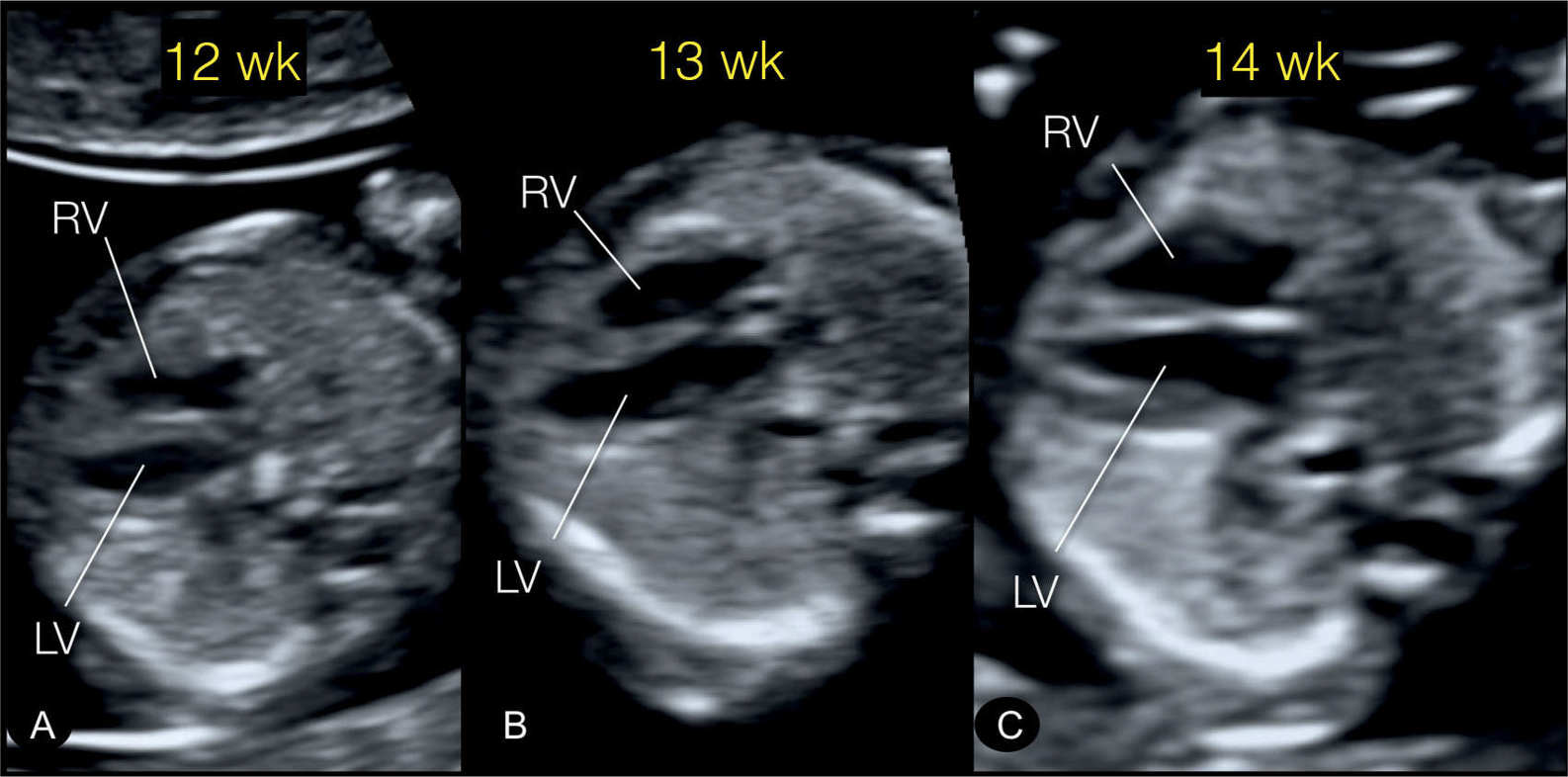
Figure 16.2: Transverse four-chamber views in three normal fetuses at 12+4 (A), 13 (B), and 14+4 (C) weeks’ gestation. Fetus at 12 (A) weeks’ gestation was examined transvaginally, while both fetuses at 13 (B) and 14 (C) weeks’ gestation were examined by high-resolution transabdominal probe (4–8 MHz). The switch from a transvaginal to a transabdominal approach can be achieved between 12 and 13 weeks’ gestation in most cases. LV, left ventricle; RV, right ventricle.
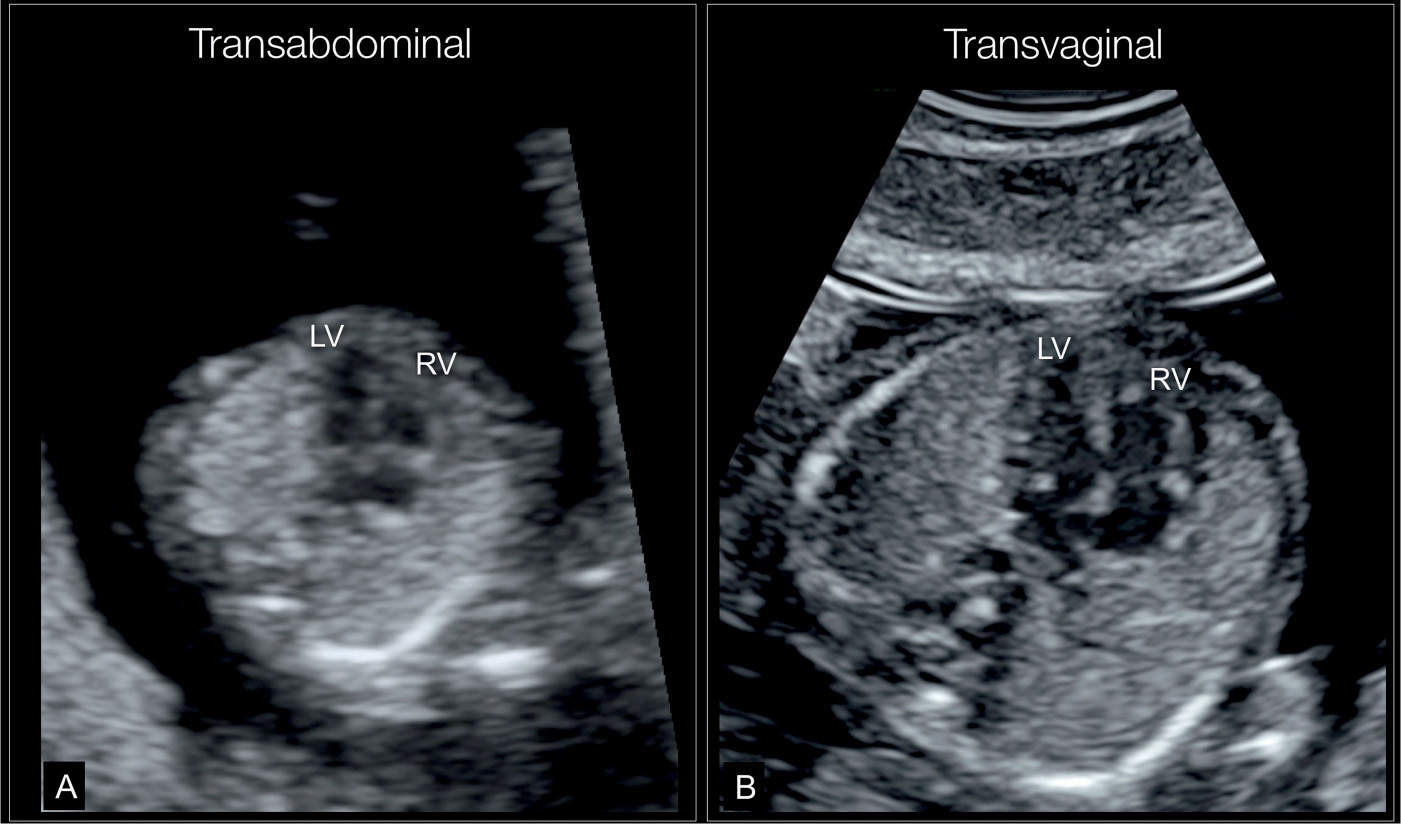
Figure 16.3: Apical four-chamber view at 13 weeks’ gestation in two normal fetuses imaged transabdominally (A) and transvaginally (B). Note the higher resolution in B in comparison to A. LV, left ventricle; RV, right ventricle.
Sufficient data on the efficacy of early fetal echocardiography have been mounting, and this examination is now considered an integral part of fetal cardiology in several centers with expertise in this area. In this book, we have integrated in each cardiac malformation chapter a section on the detection of the abnormality in early gestation. In this chapter, we discuss basic and technical aspects related to the early fetal cardiac examination in addition to common indications and potential benefits and limitations of this approach.
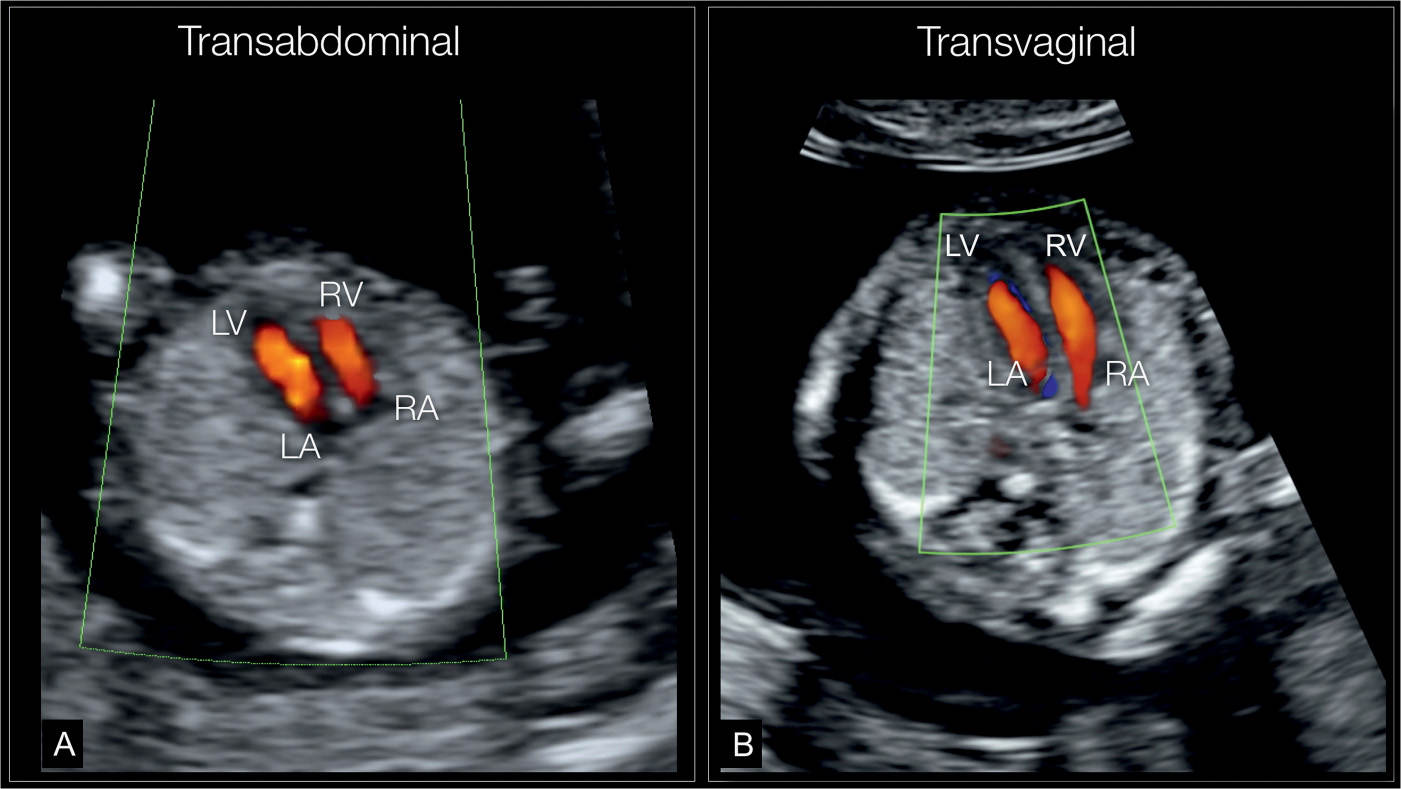
Figure 16.4: Color Doppler of an apical four-chamber view at 12 weeks’ gestation by transabdominal (A) and transvaginal (B) ultrasound examination, demonstrating diastolic flow from both right (RA) and left (LA) atria into right (RV) and left (LV) ventricles, respectively. Note that the information provided by color Doppler is very similar in both A and B. B shows a slight superior resolution by the transvaginal approach. When a cardiac anomaly is suspected, additional details may be provided by the transvaginal approach.
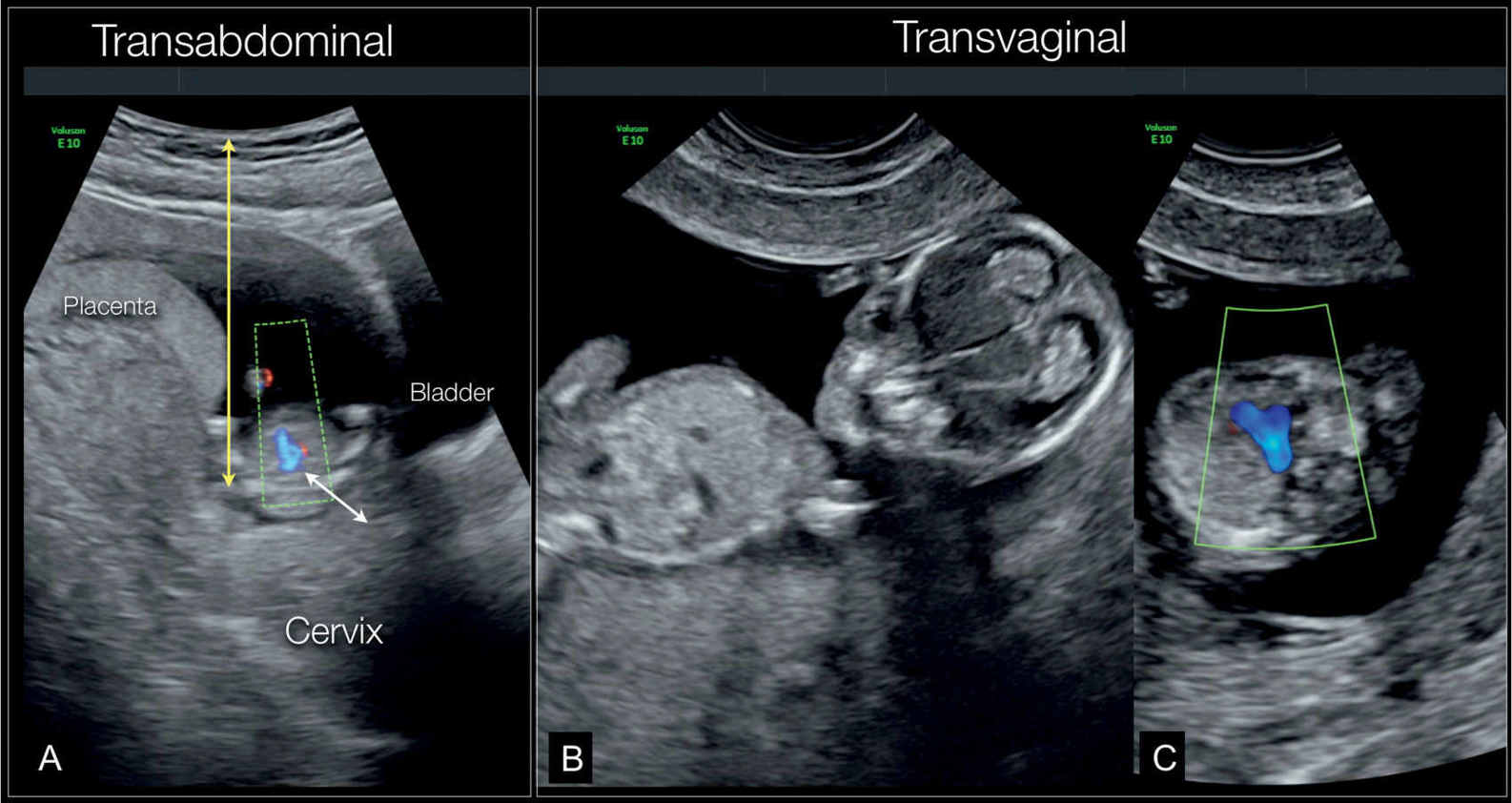
Figure 16.5: A shows a fetus at 12 weeks’ gestation scanned transabdominally with color Doppler at the three-vessel-trachea view. Note that the image displays decreased resolution, primarily due to the long distance between the transducer and the region of interest; upper fetal chest in this case (yellow arrow). Note in A the location of the fetal chest near the cervix (white arrow). B shows that the fetus is in a transverse lie, and deep in the pelvis. This represents an ideal fetal position for a transvaginal ultrasound examination. C is a transvaginal ultrasound in color Doppler at the three-vessel-trachea view, showing improved resolution over the transabdominal approach in A.
● TECHNICAL ASPECTS OF THE EARLY CARDIAC SCAN
The examination of the fetal heart in early gestation requires a modified approach from that of the second-trimester ultrasound examination. On one hand, it is a real challenge to the examiner to accurately manipulate the ultrasound equipment and get the most optimum high-resolution image on gray scale and color Doppler. On the other hand, scanning conditions are often limited by the fetal position, which often necessitates switching between the transabdominal and transvaginal route and/or the gentle manipulation of the uterus to bring the fetus in a proper position. Technical aspects of the early fetal cardiac examination are discussed in the following sections and summarized in Tables 16.1 to 16.3.
Fetus in dorsoposterior position (NT position) Magnify image Narrow sector width Fetal thorax to occupy one-third of ultrasound screen Use high-contrast image setting Use mid-to-high-resolution transducer Insonate from apical to right lateral of fetal heart |
Optimization of Color Doppler Examination in Early Cardiac Scan |
Start with grayscale optimization before activating color Doppler Use a narrow color Doppler box Use mid velocity color Doppler range Use mid filter levels Use mid-to-high persistence Use low color Doppler gain Use low power output Use bidirectional Doppler if available |
Abnormal Ultrasound Findings and Suspected Anomalies in Early Gestation Cardiac Scanning |
Four-chamber view in gray scale and color Doppler | Abnormal cardiac axis/dextrocardia Severe tricuspid insufficiency Single ventricle Large AVSD Ventricle disproportion HLHS Mitral or tricuspid atresia |
Three-vessel-trachea view | Discrepant vessel size Reverse flow in narrow PA or aorta Large aorta (CAT or DORV) One vessel (in TGA or DORV) To and fro flow in PA or aorta Interrupted vessel Aortic arch right sided to the trachea |
AVSD, atrioventricular septal defect; HLHS, hypoplastic left heart syndrome; PA, pulmonary atresia; CAT, common arterial trunk; DORV, double outlet right ventricle; TGA, transposition of the great arteries.
Transvaginal versus Transabdominal Route
It is widely accepted that the transvaginal ultrasound (TVUS) examination of the fetus is superior to the transabdominal approach in early gestation as the former provides enhanced image resolution and quality (Figs. 16.1 to 16.5). Disadvantages of the TVUS cardiac examination include the additional time, the inconvenience involved in the preparation of the vaginal probe and its sterilization after the examination is completed, and the added skills required by the operator (12). The tilting range of the probe is limited in TVUS, and the operator should be familiar with manipulating the probe in one hand and the uterus in the other hand in order to optimize the approach to the fetal chest if needed. The most optimum fetal position is the low transverse position, which provides the closest distance from the transvaginal probe to the fetal chest and explains why the best TVUS examination is achieved before 13 weeks’ gestation (crown-rump length, <70 mm), when the uterine size is still small and the fetus often lies in a transverse position (Fig. 16.5). Beyond 13 weeks, the fetus commonly assumes a longitudinal position, and the reduced depth of the high-resolution transvaginal probe limits the approach to the heart. In our experience, fetal cardiac imaging performed by the TVUS approach is achievable and reliable in most cases between 12 and 13 weeks (crown-rump length, 60–70 mm). After 13 weeks and with the latest transducers, the transabdominal route provides excellent image quality, assuming the fetus is examined in a dorsoposterior position. We encourage the reader to use, where available, linear transabdominal transducers in early fetal cardiac assessment, as they were shown to provide an enhanced image quality of the fetal heart (13, 14) (Fig. 16.6) (see also Chapter 12).
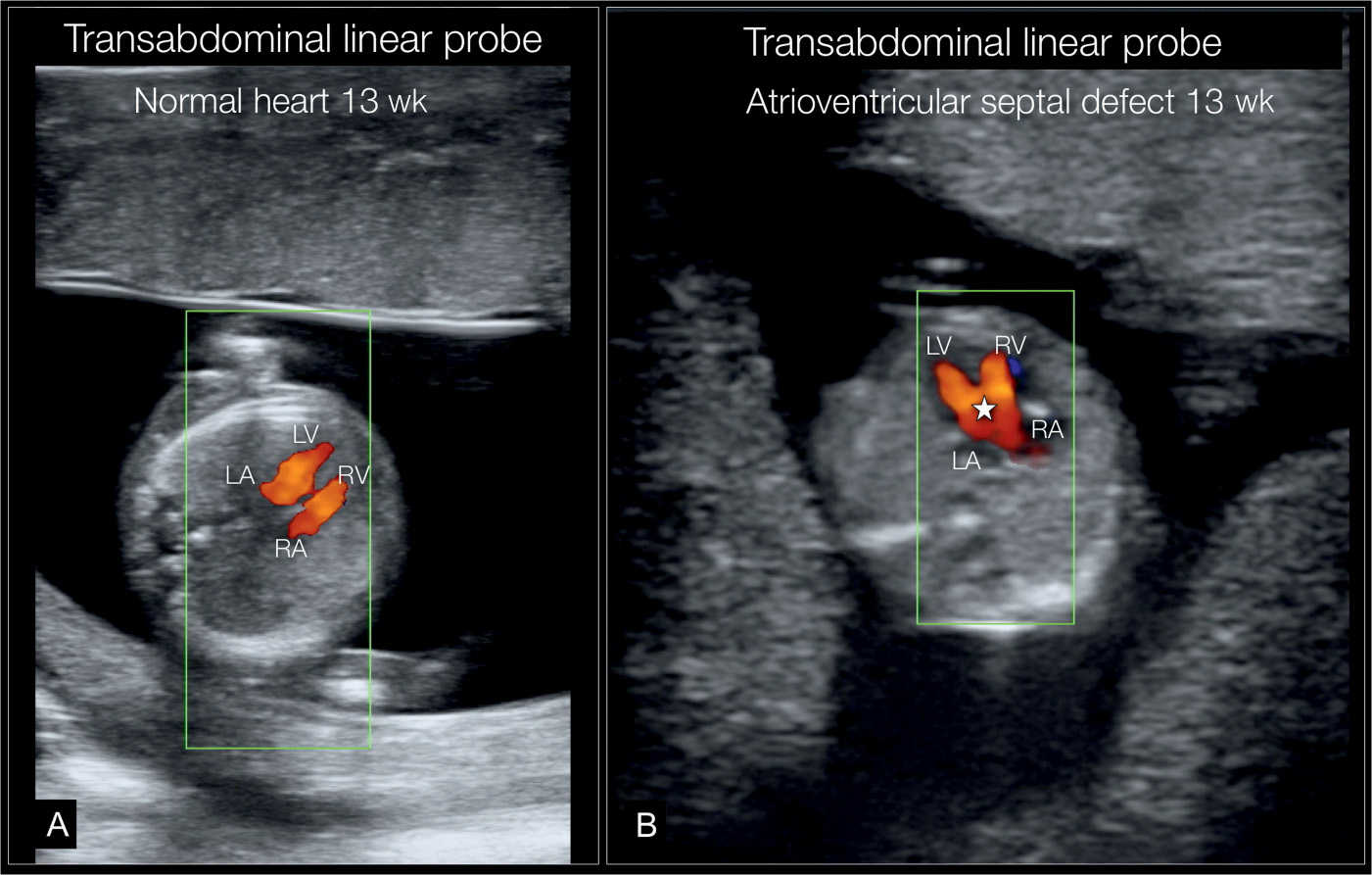
Figure 16.6: Transabdominal ultrasound in color Doppler, using a high-resolution linear probe (6–9 MHz), in two fetuses (A and B) at 13 weeks. In fetus A, a normal apical four-chamber view is shown. In fetus B, an apical four-chamber view is shown with an atrioventricular septal defect (star) seen in the center of the heart. RV, right ventricle; LV, left ventricle; RA, right atrium; LA, left atrium.
We recommend an approach that is targeted to the gestational age, maternal body habitus, and the position of the fetus in the uterus (Fig. 16.5). A combined transvaginal and transabdominal approach may be required in some cases, especially when a fetal cardiac malformation is suspected.
Cardiac Planes in Gray Scale and Color Doppler
Grayscale Examination
The optimal approach to the grayscale examination is summarized in Table 16.1. A transverse view of the fetal abdomen (Fig. 16.7) and the four-chamber view (Figs. 16.3 and 16.8) are reliably achieved with two-dimensional gray scale in early gestation. Abnormal cardiac anatomy at the level of the four-chamber view can be clearly demonstrated as early as 11 to 12 weeks’ gestation under optimal scanning conditions (Fig. 16.9). In many cases, the anatomic orientation of the right and left ventricular outflow tracts are not reliably seen due to their small size. The lumen of the vessel can, however, be better delineated by changing the insonation angle to align the great vessels in a transverse position (Fig. 16.10). In most cases, it is recommended to use color or high-definition power Doppler to reliably visualize the great vessels (see what follows).
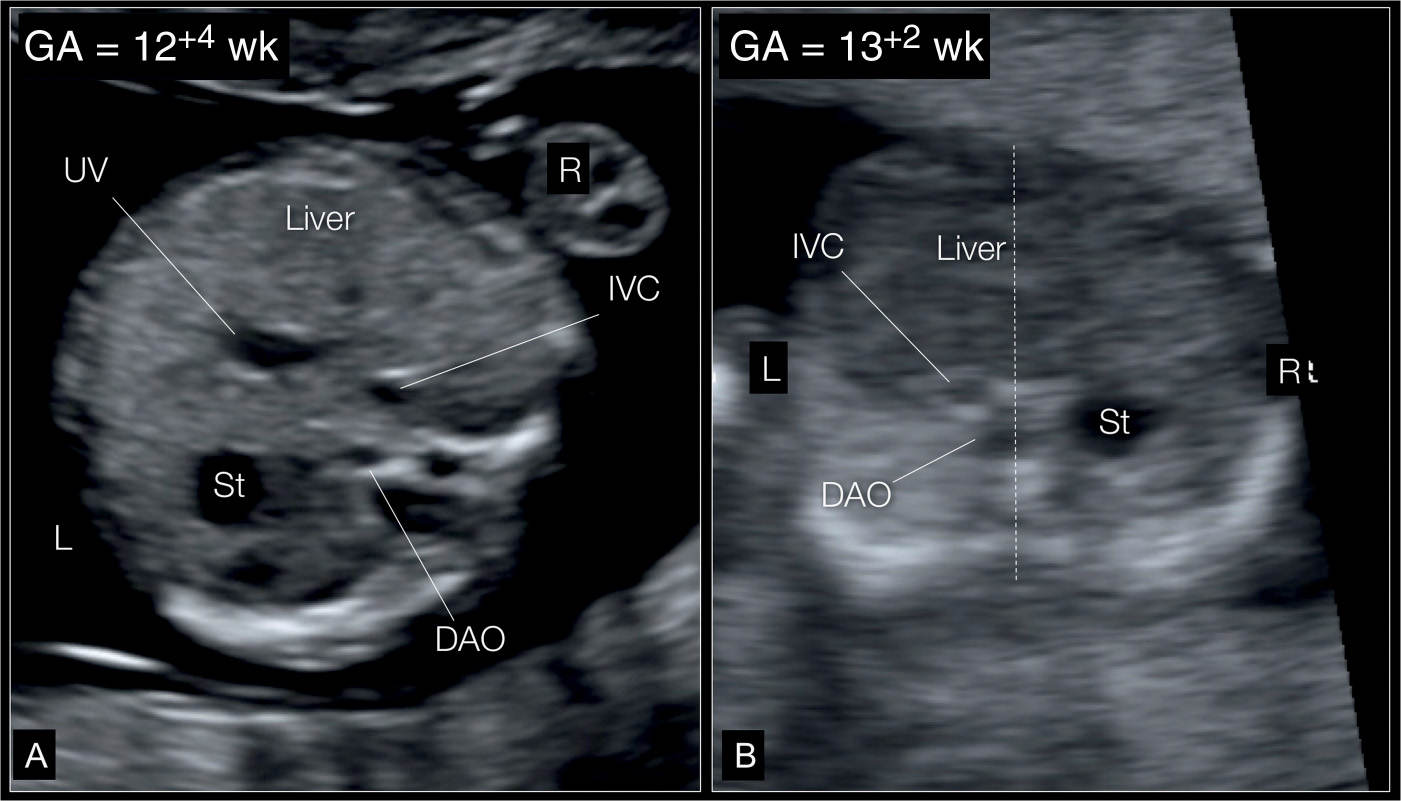
Figure 16.7: A: Transverse section of the upper abdomen in a normal fetus at 12+4 weeks’ gestation imaged by high-resolution transvaginal ultrasound. The stomach (St) and the descending aorta (DAO) are left sided, while the inferior vena cava (IVC) and liver are right sided. The umbilical vein (UV) can also be identified. This plane is visualized routinely in order to exclude situs anomalies. B: Transverse section of the upper abdomen in a fetus with right isomerism at 13+2 weeks’ gestation imaged with high-resolution transabdominal scanning. The stomach (St) is right sided, whereas the aorta (DAO), inferior vena cava (IVC), and liver are left sided. The DAO and IVC are on the same side (called juxtaposition), suggesting the presence of situs ambiguous with right isomerism (see also Chapter 30). This fetus also had a complex cardiac defect. L, left; R, right.
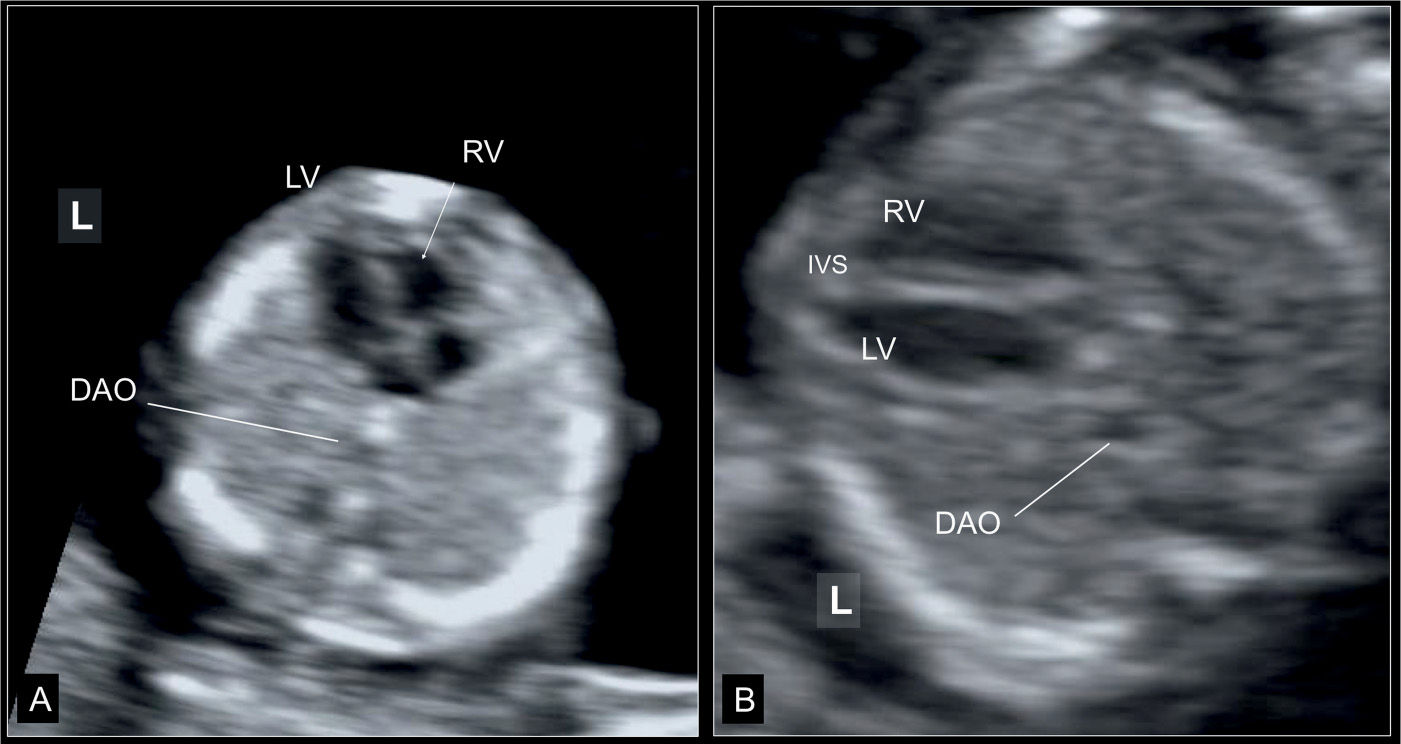
Figure 16.8: Apical (A) and axial (B) planes of the four-chamber view at 13 weeks’ gestation in two normal fetuses imaged transabdominally. Note the more apical insertion of the septal leaflet of the tricuspid valve (arrow) in A. Descending aorta (DAO) is seen in both planes and the interventricular septum (IVS) is most optimally seen in the axial or transverse plane (B). LV, left ventricle; RV, right ventricle; L, left.
Color Doppler Examination
Color Doppler is a major tool in the early cardiac scan and its use is not only limited to the detection of flow events. Due to the low resolution of the gray scale at this stage, color Doppler helps enormously in delineating the shape of the vessels and chambers and it is thus used for a structural assessment as well (Figs. 16.11 to 16.13). Optimal use of color Doppler is summarized in Table 16.2. Color or high-definition power Doppler provides significant advantages in cardiac imaging in early gestation by demonstrating blood flow events in addition to flow direction. The color or high-definition power Doppler filling of an apical or basal four-chamber view separated by the septum is a good adjunct to the grayscale image (Fig. 16.11). We feel that color Doppler at the level of the four-chamber view in early cardiac examination is essential in identifying normal and abnormal cardiac anatomy (Figs. 16.4, 16.6, 16.11, and 16.14). Color or high-definition power Doppler demonstration of the upper transverse views in the chest, including the three-vessel-trachea and the transverse ductal views, is, however, superior to what can be provided by the grayscale evaluation alone (Figs. 16.12 and 16.13). Aortic and ductal arches are more easily recognized in their anatomic location, size, patency, and blood flow direction (Figs. 16.12, 16.13, and 16.15) and the demonstration of the right and left pulmonary veins draining into the left atrium (Fig. 16.13B). Several cardiac abnormalities involving the outflow tracts can be recognized in the three-vessel-trachea view, and a right aortic arch can also be clearly identified (Fig. 16.15). Table 16.3 summarizes abnormal grayscale and color Doppler findings at the level of the four-chamber view and three-vessel-trachea view in early cardiac scan.
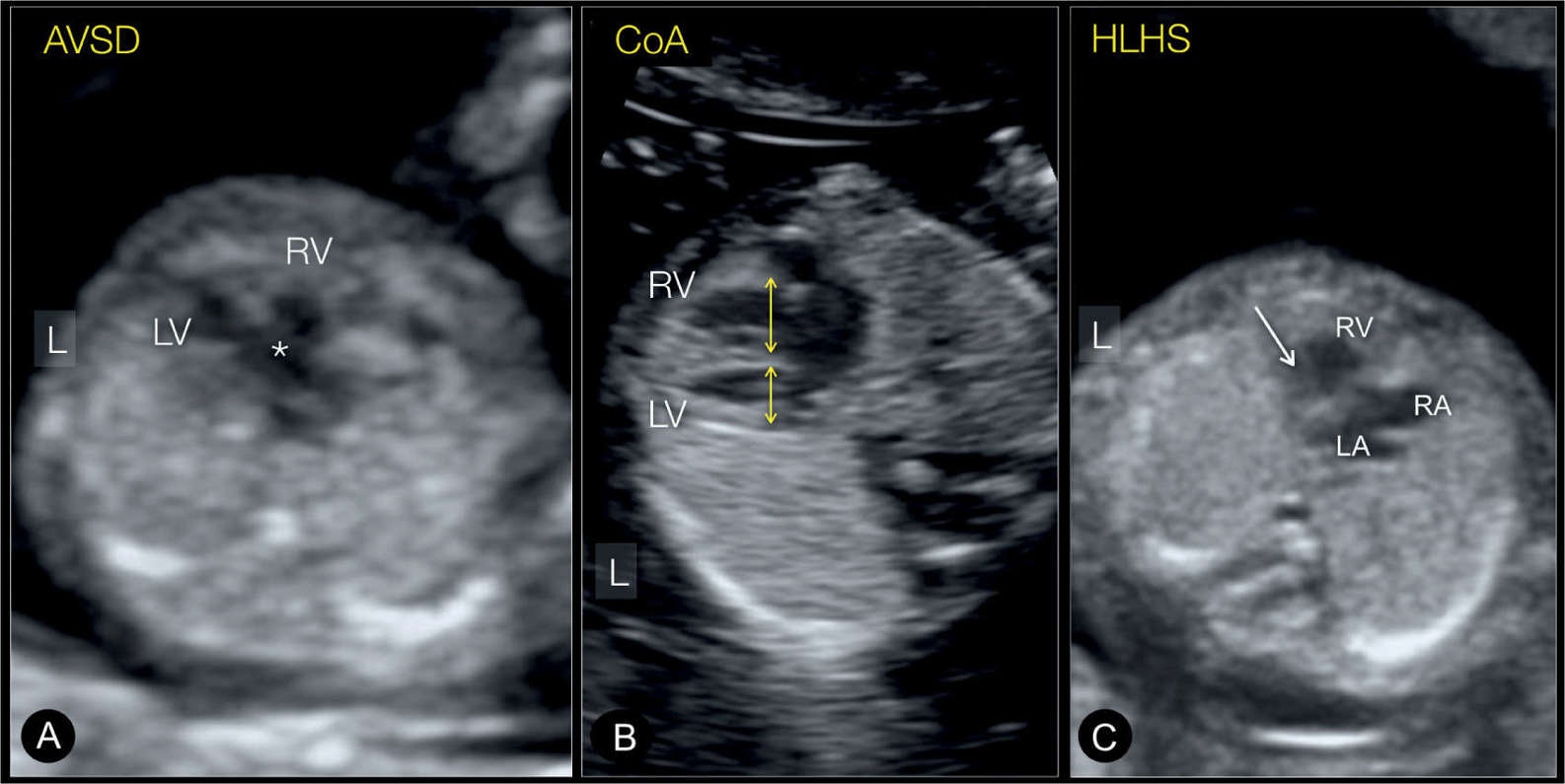
Figure 16.9: Transverse four-chamber views in gray scale in three fetuses (A, B and C) at 12 to 13 weeks’ gestation with abnormal cardiac anatomy. In fetus A, a large atrioventricular septal defect (AVSD) (star) is demonstrated in the center of the heart between the right (RV) and left (LV) ventricles. In fetus B, ventricular disproportion is seen with a smaller LV in aortic coarctation (CoA). In fetus C, there is only one RV seen with the left ventricle missing (arrow). Comprehensive examination in color Doppler in C revealed a hypoplastic left heart syndrome (HLHS). L, left.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


