Esophagus
Patrick A. Dillon
Washington University School of Medicine, St. Louis Children’s Hospital, St. Louis, Missouri 63110.
EMBRYOLOGY
Although the normal esophagus can be identified as a distinct structure by the fourth week of embryogenesis, the development of the esophagus has remained controversial. The development of the esophagus is intimately related to the embryology of the trachea, and the separation of these two foregut structures is complete before the fifth week of gestation. The separation usually proceeds in a caudad to cephalad direction. During subsequent development, the esophagus increases in length more rapidly than the fetus as a whole and reaches its final length (8 to 10 cm at birth) by 7 weeks (1). A more recent theory supports the idea of the respiratory epithelium developing from the ventral foregut and creating a stalk (Fig. 64-1) of tissue that will form the trachea. Experimental studies support aspects of both theories (2,3). Ciliated columnar epithelium appears in the esophagus at approximately 10 weeks’ gestation and stratified squamous epithelium replaces it at around 20 to 25 weeks, a process that begins in the midesophagus and proceeds both caudad and cephalad. The muscular fibers of the esophagus appear to develop at different rates. Circular muscle is present at 8 weeks, whereas longitudinal muscle becomes apparent by approximately 13 weeks’ gestation in the human embryo. In fetuses, the thickness of the muscularis externa increases linearly from 8 weeks to term (40 weeks), then growth slows postnatally (4,5). Neurons can be recognized concomitantly with circular muscle at 8 weeks, with peak density occurring by 16 to 20 weeks. Subsequently, there is rapid decline in the number of neurons during the second trimester, and this is reduced further toward adult levels during infancy. The numbers of ganglion cells and nerve fibers in the myenteric plexus are also maximal at 16 to 20 weeks. However, their density decreases with increasing gestational age, and by 30 weeks, it becomes constant despite further esophageal growth (4,5). Relationships between neuropeptides, neuronal function, and the ontogeny of esophageal motor activity have yet to be characterized (5).
Maturation of esophageal motility appears to progress in an orderly fashion postnatally. However, the relevance of certain developmental events in utero is not known. For example, we do not know whether the functional status of preterm infants [reduced lower esophageal sphincter pressure, simultaneous contractions and noncoordinated peristalsis, and frequent transient lower esophageal sphincter (LES) relaxations] represents merely delayed development or confers some specific adaptive advantage to the third-trimester human fetus. Fetal swallowing can be detected as early as 11 weeks’ gestation, with sucking movements beginning as early as 18 and 20 weeks (6). The swallowing of amniotic fluid begins very slowly with a few milliliters per day and increases to 450 mL per day in the third trimester (7). In animals, fetal swallowing defects have been correlated with failure of growth of the gastrointestinal (GI) tract, as well as ultrastructural abnormalities (8). Careful studies of human fetuses are not available.
ANATOMY
The arterial blood supply to the esophagus is generally considered with regard to the cervical, thoracic, and abdominal segments of the esophagus.
The arterial blood supply to the pharyngoesophageal junction and the cervical esophagus is derived from branches of the inferior thyroid artery. In addition, the junctional area of the esophagus is supplied by small arterial branches of the subclavian, common carotid, vertebral, superior thyroid, and costocervical trunk vessels (9). The thoracic esophagus is supplied from branches of the aorta, the bronchial arteries, and the right intercostal arteries. Bronchial artery branches enter the esophagus at the level of the carina and proceed inferiorly along the ventral aspect of the esophagus. Accessory esophageal branches are also present directly from the aorta, the internal
mammary, common carotid, and superior intercostal arteries (10). Esophageal branches of the aorta supply the esophagus immediately below the level of the carina. These vessels have ascending and descending branches that form anastomoses with the inferior thyroid and left gastric arterial branches (10). The left gastric artery provides esophageal blood supply to the abdominal segment of the esophagus in most individuals. Rarely, esophageal arteries will arise from an accessory left hepatic artery. In fewer than one-half of individuals, the esophagus receives arterial blood via the left inferior phrenic artery, and rarely from the right inferior phrenic artery (9). A well-developed subepithelial network of capillaries is present in the esophageal mucosa and submucosa (11,12). Venous drainage from the esophagus includes intrinsic, extrinsic, and longitudinal vessels. The intrinsic system includes subepithelial and submucosal veins that join gastric veins, and perforating veins that join with the extrinsic system of veins. The extrinsic veins include larger longitudinal vessels that run on the outer surface of the esophagus and are close to the vagus nerves. These vessels connect the left gastric vein to the azygous or hemiazygous veins either directly or indirectly or via the posterior bronchial veins. Extrinsic veins include the cervical drainage into the inferior thyroid, vertebral, and deep cervical veins. Esophageal veins at the level of the cardia join the phrenic and abdominal esophageal veins to drain primarily into the left gastric vein, as well as the gastroepiploic and splenic veins (13). This may be a point of importance when dealing with a patient with portal hypertension.
mammary, common carotid, and superior intercostal arteries (10). Esophageal branches of the aorta supply the esophagus immediately below the level of the carina. These vessels have ascending and descending branches that form anastomoses with the inferior thyroid and left gastric arterial branches (10). The left gastric artery provides esophageal blood supply to the abdominal segment of the esophagus in most individuals. Rarely, esophageal arteries will arise from an accessory left hepatic artery. In fewer than one-half of individuals, the esophagus receives arterial blood via the left inferior phrenic artery, and rarely from the right inferior phrenic artery (9). A well-developed subepithelial network of capillaries is present in the esophageal mucosa and submucosa (11,12). Venous drainage from the esophagus includes intrinsic, extrinsic, and longitudinal vessels. The intrinsic system includes subepithelial and submucosal veins that join gastric veins, and perforating veins that join with the extrinsic system of veins. The extrinsic veins include larger longitudinal vessels that run on the outer surface of the esophagus and are close to the vagus nerves. These vessels connect the left gastric vein to the azygous or hemiazygous veins either directly or indirectly or via the posterior bronchial veins. Extrinsic veins include the cervical drainage into the inferior thyroid, vertebral, and deep cervical veins. Esophageal veins at the level of the cardia join the phrenic and abdominal esophageal veins to drain primarily into the left gastric vein, as well as the gastroepiploic and splenic veins (13). This may be a point of importance when dealing with a patient with portal hypertension.
Oblique muscular fibers that fuse with pharyngeal constrictor muscles and transverse fibers that encircle the esophagus compose the cricopharyngeal (CP) muscle. The CP muscle is a unique striated muscle in that contraction occurs while at rest. During swallowing, belching, and vomiting, relaxation of the muscle occurs and the upper esophagus opens (14). The CP muscle is located at the pharyngoesophageal junction, attaches to the cricoid cartilage, and forms a C-shaped muscular band with innervation by the pharyngeal plexus of the vagus nerve and the recurrent laryngeal nerve (Fig. 64-2). The recurrent laryngeal nerve projects to the anterior motor units located in the anterior segments of the horizontal part of the muscle, whereas the pharyngeal plexus projects to the posterior motor units of the muscle (15). The main function of the CP muscle is to control luminal flow between the pharynx and esophagus. The CP sphincter muscle is tonically contracted at rest and relaxes during swallowing. The major component of the upper esophageal sphincter (UES) is the CP muscle, although the inferior pharyngeal constrictor and striated muscles of the proximal esophagus also contribute (16). The CP muscle posteriorly is where the longitudinal muscles diverge to attach to the cricoid cartilage. This area is vulnerable to perforation during esophagoscopy. Videofluoroscopy and manometry studies have been the source of data used to link the CP muscle to the UES in deglutition (17).
The LES area corresponds to the position of the CP muscle in the cervical esophagus, although there is no specific muscle to correspond at the LES. There is a sphincter equivalent at the level of the gastroesophageal (GE) junction. The primary role of the LES is to prevent gastroesophageal reflux (GER). The LES relaxes as a primary esophageal wave moves through the esophagus toward the
GE junction. The LES is also responsive to intraabdominal pressure, gastrin, secretin, narcotics, benzodiazepines, theophylline, and its derivatives, caffeine, chocolate, and alcohol.
GE junction. The LES is also responsive to intraabdominal pressure, gastrin, secretin, narcotics, benzodiazepines, theophylline, and its derivatives, caffeine, chocolate, and alcohol.
ESOPHAGOSCOPY
Pediatric esophagoscopy was first used for the removal of foreign bodies. Presently, it is used to evaluate symptoms of dysphagia and GER, to evaluate and dilate congenital or acquired esophageal strictures, to evaluate the esophagus after trauma, for sclerotherapy for bleeding esophageal varices, and to carry out gastrostomy tube or button placement. Before esophagoscopy, an evaluation of the child should be undertaken that is appropriate for the condition being addressed. The radiologic evaluation of most esophageal disorders begins with a frontal and lateral chest radiograph, a contrast esophagogram, or a chest computed tomography (CT) imaging study. The definitive diagnosis, however, of many of the disorders in childhood depends on direct observation by esophagoscopy.
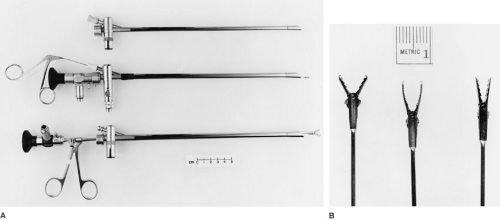
Both flexible and rigid esophagoscopes are available that are suitable for use in children. The advantage of the flexible esophagoscope is that it may be used with topical anesthesia and sedation for routine diagnostic endoscopy in children. The disadvantages of this instrument are that the biopsy and foreign-body instruments that pass through the operating channel are relatively small, and therapeutic esophagoscopy can be impractical.
Rigid esophagoscopes are available in sizes suitable for use in any infant or child (Fig. 64-3). These instruments employ the same Hopkins rod-lens telescope used for rigid bronchoscopy and provide superior visualization compared with flexible instruments. Foreign-body and biopsy instruments may be passed through a separate channel of the esophagoscope, or larger instruments may be coupled to the telescope and passed directly through the lumen of the scope. In addition to the availability of a broader range of sizes of endoscopes, the rigid esophagoscope allows passage of larger instruments, thus facilitating therapeutic esophagoscopy.
Diagnostic esophagoscopy with the flexible gastroscope may be performed under topical anesthesia with intravenous sedation. Pretreatment with atropine is used to reduce oral secretions and block reflex bradycardia. These children should be observed with cardiac and oxygen saturation monitors during the procedure. The child is placed in the left lateral position with the neck slightly extended. A plastic mouth guard may be used in older children, but is not needed for infants without teeth. The esophagoscope is passed gently over the tongue, and a slight deflection is placed in the tip as the patient is induced to swallow. With gentle pressure, the scope is pushed through the CP sphincter into the upper esophagus. It is then passed through the length of the esophagus, keeping the lumen under direct
vision. The GE junction may be visualized from below by passing the instrument into the stomach and retroflexing. Care must be taken not to insufflate excessive air because many smaller children experience respiratory distress with gastric distension. The region of the CP sphincter is more carefully examined as the esophagoscope is withdrawn.
vision. The GE junction may be visualized from below by passing the instrument into the stomach and retroflexing. Care must be taken not to insufflate excessive air because many smaller children experience respiratory distress with gastric distension. The region of the CP sphincter is more carefully examined as the esophagoscope is withdrawn.
The technique of rigid esophagoscopy is more difficult to learn and has a higher incidence of complications in inexperienced hands. Rigid esophagoscopy is performed under general anesthesia in children. Because of the flexibility of the larynx and upper airway, these children should be intubated for airway control before insertion of the esophagoscope. The patient is placed supine, and a soft roll is placed under the shoulders to extend the cervical spine. The appropriate-size esophagoscope is passed gently along the right border of the tongue into the right piriform sinus under direct vision. The scope is then moved medially to visualize the right arytenoid cartilage and the posterior wall of the larynx. The tip of the scope is gently insinuated behind the posterior laryngeal wall and directed anteriorly to expose the CP sphincter. Under general anesthesia, this sphincter is usually relaxed and open, and the esophagoscope can be passed under direct vision into the upper esophagus. If the sphincter is in spasm, a small filiform dilator or a nasogastric tube can be passed through the esophagoscope into the upper esophagus and used as a guide. The esophagoscope is supported and manipulated by the surgeon’s left hand, which also protects the child’s teeth. The endoscope is passed through the body of the esophagus under direct vision. To pass the esophagoscope through the GE junction, the head must be hyperextended and the instrument passed to the left, anteriorly. It should be possible to visualize the entire length of the esophagus from the CP sphincter to the GE junction with this equipment.
Complications of esophagoscopy are more common than with bronchoscopy. The complications of passage of either the rigid or flexible scopes are usually encountered at the level of the CP muscle. Perforation of the cricopharyngeus occurs in about 0.03% of patients with flexible esophagoscopy, but mucosal lacerations are not unusual. Perforation of the piriform sinus or the posterolateral aspect of the CP sphincter is more common with the rigid esophagoscope and occurs in about 0.1% of patients. Perforation of the body of the esophagus is rare and occurs principally when biopsy specimens are taken or in patients with esophageal stricture.
Iatrogenic perforation of the esophagus is the most common cause of perforation encountered in children. The diagnosis is suspected with the development of a spiking fever or pain and crepitation in the cervical region after esophagoscopy. The diagnosis is confirmed by demonstration of mediastinal or cervical emphysema on plain radiograms and extravasation of contrast on esophagogram. Most iatrogenic perforations are small and well contained. These may be treated with intravenous antibiotics, with the child receiving nothing by mouth. Larger perforations and those communicating with a pleural space need open drainage and attempts at closure. Pleural flaps or intercostal muscle flaps may be used to secure the esophageal closure.
FOREIGN-BODY INGESTION
The accidental ingestion of aerodigestive foreign bodies by children occurs frequently and, although is usually associated with minimal morbidity, can occasionally result in significant morbidity and even mortality (18). More than one-half of the children are less than 4 years old. In most cases, the episode is either witnessed by an adult or the child tells of the ingestion. Young children tend to sample their environment by placing things in their mouth. For this reason, all manner of objects may be swallowed. The majority of them are not excessively large in proportion to the esophagus and are not sharp edged. They can be swallowed and not become impacted in the esophagus. If the object enters the stomach, there is good likelihood that it will pass through the remainder of the GI tract. An exception is the child with a congential or acquired intestinal stricture, such as a child after an episode of necrotizing enterocolitis. Coins continue to be the most common objects swallowed. Of note, there is increasing incidence of small button-type batteries being ingested (19). These batteries can leak chemicals, which can cause esophageal scarring or perforation. Approximately 20% of ingested foreign bodies become lodged in the esophagus and will require removal (20). The inability of the esophagus to propel the object into the stomach may be due to the size of the object, its configuration, or the degree or lack of esophageal peristalsis.
Dysphagia, excessive salivation, neck pain, and occasional choking are the symptoms commonly seen in these children. Approximately 10% may be asymptomatic (21). This is a high enough incidence that if there is a clinical suspicion of ingestion, radiologic evaluation should be carried out. Patients at increased risk for foreign-body obstruction are those who have undergone repair of an esophageal atresia or tracheoesophageal fistula, who are neurologically impaired, or who are psychiatric patients. The diagnosis is usually made at the initial evaluation, but a delay in recognition is not unusual and is directly related to the incidence and severity of complications in removal of the foreign body (22).
The most common sites of foreign-body impaction are at points of relative narrowing in the neck at the level of the CP muscle, in the thorax at the level of the aortic arch and left mainstem bronchus, and at the GE junction. Another point of obstruction can be at an anastomotic stricture. Objects lodged at the level of the CP muscle can cause neck pain. A foreign body in the upper third of the thoracic esophagus can produce respiratory symptoms because
of its position in the esophagus directly contiguous with the membranous trachea. Pain may be produced throughout the length of the esophagus due to mucosal irritation or erosion and perforation. This process is usually acute; however, occasionally an object may be chronically impacted and cause obstruction due to its presence as an inflammatory mass (23). Foreign bodies lodged in the upper and middle third of the esophagus should be removed because it is unlikely they will spontaneously pass. In contrast, the majority of coins in the distal esophagus will pass spontaneously (24). Allowing the patient to drink some liquids and a short period of waiting is reasonable in selected instances (25).
of its position in the esophagus directly contiguous with the membranous trachea. Pain may be produced throughout the length of the esophagus due to mucosal irritation or erosion and perforation. This process is usually acute; however, occasionally an object may be chronically impacted and cause obstruction due to its presence as an inflammatory mass (23). Foreign bodies lodged in the upper and middle third of the esophagus should be removed because it is unlikely they will spontaneously pass. In contrast, the majority of coins in the distal esophagus will pass spontaneously (24). Allowing the patient to drink some liquids and a short period of waiting is reasonable in selected instances (25).
The incidence of esophageal perforation is low, approximately 1%. However, if the diagnosis of an esophageal foreign body is delayed, there is a greater risk of morbidity, including perforation and mediastinitis (26). All retained foreign bodies and those with sharp edges should be removed.
The removal of the foreign body can be done in several ways. The majority of cases are treated by endoscopic removal with a rigid esophagoscope under a general anesthetic to protect the airway. The rigid esophagoscope has ports large enough to pass the appropriate foreign-body graspers and telescopes. For smooth foreign objects, particularly in the upper half of the esophagus, balloon extraction performed with procedural sedation in the radiology suite or in the operation room is a reasonable option. Antegrade bougilnage and flexible endoscopy are appropriate in selected cases.
Patients with esophageal perforation may present with respiratory distress, including tachypnea, stridor, retractions, and supplemental oxygen requirement. The child may present in this manner initially, or this may be seen shortly after foreign-body extraction. Hematemesis or hemoptysis may signal a vascular erosion (26).
Treatment of the patient with an esophageal perforation includes removal of the foreign body, surgical drainage of the mediastinum, and repair or diversion of the perforation. In selected cases with a contained mediastinal perforation, endoscopic removal of the foreign body, intravenous antibiotics, and avoidance of oral intake may suffice.
CAUSTIC ESOPHAGEAL INJURY
Although federal legislation has greatly improved product labeling, packaging, and their contents, caustic ingestion in children continues to be a significant problem. Anderson et al. estimated approximately 17,000 ingestions in children (27). The vast majority of these cases are accidental and seen in children younger than 5 years old. These caustic substances are usually separated into acids and alkalis. Household and industrial acids include hydrochloric acid (toilet bowl and swimming pool cleaners), sulfuric acid (storage batteries), and phosphoric acid (metal cleaners). Strong acids, usually with a pH less than 2, produce a coagulation necrosis, and penetrating injury may occur if a sufficient volume of acid is ingested. Ingested hydrofluoric acid, in contrast, results in a liquefaction necrosis of the esophagus and can cause death secondary to an imbalance in calcium metabolism from fluoride absorption. Most and the most severe caustic injuries are due to household cleaning alkalis (28). The volume and nature of the alkali will determine the depth and extent of injury to the esophagus. Alkalis produce a liquefaction necrosis often deep and transmural, and are frequently more severe when compared with acid ingestion. There may be associated vascular thrombosis, perforation, and contracture of the esophagus. Sodium hydroxide, commonly used as a drain cleaner, can be especially dangerous. It often comes in liquid form, is easily ingested and may cause injury to the surrounding organs, such as the larynx, trachea, aorta, colon, or pancreas (29). Although household bleach may be the most frequently ingested material, this rarely causes serious injury. Newer dishwashing agents are known to have a high pH and can be especially injurious to the esophagus (30).
The signs and symptoms seen in children with an ingestion injury include oropharyngeal pain, irritability, vomiting, drooling, and at times, respiratory distress. The mouth and the pharynx should be inspected for evidence of injury, although the absence of visible oral burns does not preclude esophageal or gastric involvement. Initial care is aimed at control of the airway, if necessary, administering intravenous fluids, and control of pain. Chest and abdominal radiographs are obtained to evaluate for mediastinal or intraperitoneal air. With the patient stabilized, endoscopic evaluation for esophageal injury beyond the cricopharyngeus should be carried out within the initial 24 hours following injury to avoid the time of maximum edema. This procedure is performed under general anesthesia and preferably uses the rigid esophagoscope, although a flexible endoscope can also be used. The esophagoscope should be passed only to the first area of injury beyond the cricopharyngeus to prevent iatrogenic injury. If respiratory symptoms are also present, laryngoscopy and bronchoscopy should also be performed. Endoscopic assessment of the injury can be graded (Table 64-1) according to the extent of mucosal injury and can be useful in planning future management. First-degree injuries of the esophagus usually result in mucosal erythema and edema, and no additional therapy is required. Second- and third-degree injuries are characterized by mucosal ulceration and the formation of pseudomembranous plaques. Second-degree injuries are noncircumferential, whereas third-degree injuries are circumferential and may involve mucosal sloughing and thrombosis of submucosal esophageal vessels (31).
Patients with second- and third-degree burns are generally treated with parenteral antibiotics. The use of corticosteroid for caustic ingestions of the esophagus remains
controversial (27,32,33,34). Many surgeons favor treatment for several weeks with prednisone 2.0 to 2.5 mg per kg per day and ampicillin 50 mg per kg per day to attempt to minimize an inflammatory response and subsequent stricture formation. However, there is no contemporary evidence-based study to support this protocol. Steroids may be more effective in the established stricture by allowing a significant increase in time between dilatations (30). Esophageal perforation or hemorrhage is an indication for emergency thoracotomy and esophagectomy. Twenty-five percent of patients will develop strictures and require dilation. Triamcinolone injection into the stricture may be helpful (35). Esophageal dilations have remained the mainstay of treatment for esophageal strictures. There has been some more recent use of esophageal stents to treat refractory strictures. The development of obstructing granulation tissue and stent migration has limited their effectiveness in the pediatric population. Despite these drawbacks, stents may provide limited relief and may reduce the overall frequency of esophageal dilatations (30,36). Determining when to abandon esophageal dilatation and proceed to esophageal replacement surgery can be difficult. Factors making esophageal replacement surgery more probable include a delay in the time of ingestion injury to the start dilatations (more than 1 month), the length of the stricture (more than 5 cm), and esophageal perforation during dilatation (36).
controversial (27,32,33,34). Many surgeons favor treatment for several weeks with prednisone 2.0 to 2.5 mg per kg per day and ampicillin 50 mg per kg per day to attempt to minimize an inflammatory response and subsequent stricture formation. However, there is no contemporary evidence-based study to support this protocol. Steroids may be more effective in the established stricture by allowing a significant increase in time between dilatations (30). Esophageal perforation or hemorrhage is an indication for emergency thoracotomy and esophagectomy. Twenty-five percent of patients will develop strictures and require dilation. Triamcinolone injection into the stricture may be helpful (35). Esophageal dilations have remained the mainstay of treatment for esophageal strictures. There has been some more recent use of esophageal stents to treat refractory strictures. The development of obstructing granulation tissue and stent migration has limited their effectiveness in the pediatric population. Despite these drawbacks, stents may provide limited relief and may reduce the overall frequency of esophageal dilatations (30,36). Determining when to abandon esophageal dilatation and proceed to esophageal replacement surgery can be difficult. Factors making esophageal replacement surgery more probable include a delay in the time of ingestion injury to the start dilatations (more than 1 month), the length of the stricture (more than 5 cm), and esophageal perforation during dilatation (36).
TABLE 64-1 Endoscopic Grading of Caustic Esophageal Injuries. | ||||||||
|---|---|---|---|---|---|---|---|---|
| ||||||||
There is increased risk of the development of esophageal adenocarcinoma in these patients. Long-term follow-up and surveillance is necessary.
ESOPHAGEAL CYSTS
Esophageal cysts and duplications comprise approximately 10% of all GI tract duplications. Fallon et al. proposed two classes of esophageal cysts: intramural esophageal cysts and enteric cysts (37). Intramural esophageal cysts occur within the wall of the esophagus and are believed to represent defects of vacuolation of the primitive esophagus (38). During the fourth week of development, the esophageal mucosa proliferates to obliterate the esophageal lumen completely. At 6 weeks’ gestation, vacuoles begin to form within this solid mass of epithelial cells, gradually coalescing to reestablish an esophageal lumen. Disruption of this process presumably leaves epithelial cells within the wall of the esophagus, which can lead to development of intramural esophageal cysts (39). These cysts are lined by columnar or pseudostratified columnar epithelium with cilia, which is consistent with the foregut epithelium of a 4- to 6-week embryo. These lesions have been referred to as true duplications of the esophagus and archenteric cysts, although the term intramural esophageal cysts seems most appropriate. The embryology of enteric cysts is more controversial, but most authors believe they are caused by abnormalities that occur during separation of the endoderm from the notochord. Persistence of neuroenteric canals or a split notochord syndrome is often used to explain the development of posterior mediastinal cysts when there are vertebral abnormalities or an extensive duplication (40). The notochord appears at the third week of gestation and simultaneously is believed to begin separation from the endoderm (Fig. 64-4). A gap in the notochord can occur during separation, and a diverticulum of the foregut can lead to a number of anomalies. Vertebral anomalies indicate spina bifida and hemivertebrae. In addition, a tract can form, and the gut may form short or long diverticula or fistulas along any portion of the GI tract (41). Esophageal duplications are usually identified in the thoracic esophagus, although cervical esophageal duplications have been reported (42). Two-thirds of enteric cysts in the esophagus are identified during childhood.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree