Epidemiology of Childhood Cancer
Louise Parker
CANCER IS AN IMPORTANT CAUSE OF MORTALITY
Childhood cancer is diagnosed in around 1 in 600 children under age 15 years. Nonetheless, cancer is an important cause of death in children. After the first year of life, cancer is the single most common disease-related cause of death in children. In 2004 in the United States, there were 11,619 deaths in children ages 1 to 14 years; of these, 5365 were due to disease and 26% of these (ie, 1418) were due to cancer (eTable 444.1  ).1
).1
CHILDHOOD CANCER IS A NUMBER OF DIFFERENT DISEASES 
In children, the spectrum of disease is different to that in adults. In Canada from 2000 to 2004, leukemias accounted for around 33% of childhood malignancies, brain and other central nervous system tumors for 20%, (Fig. 444-1).2 The distribution is similar in other geographic areas.3,4 Over the course of childhood, the types of cancers change: In infants, the most common form of cancer is neuroblastoma (25%) and for 1- to 14-year-olds, the most common is leukemia (42%, ages 1–4; 34% of cases, ages 5–9; and 22% of cases ages 10–14; eFig. 444.1).2 Overall, the rate of cancer is about 20% higher in boys than in girls, with the difference being most marked for lymphomas, which are twice as common in boys (eFig. 444.2  ).2
).2
THE INCIDENCE VARIES BETWEEN POPULATIONS
Rates of childhood cancer have been reported for many countries, and much of these data have been assembled by the International Agency for Research in Cancer (IARC) in Lyon, France (http://www.iarc.fr/).5 A sample of US cases are reported in the SEER (Surveillance Epidemiology Endpoints Results) data set (http://seer.cancer.gov/), which covers around 26% of the US population. 
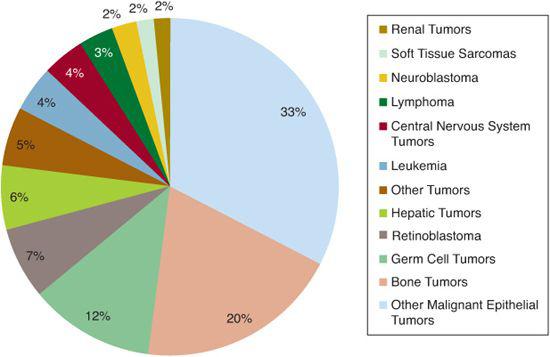
FIGURE 444-1. Distribution of childhood cancers, ages 0–14 years. (Source: Data from Canadian Cancer Society/National Cancer Institute of Canada: Canadian Cancer Society Statistics 2008. Toronto, Canada 2008.)
Across the 15-year age span, infants and 1-to 4-year-old children have the highest rates of malignant disease. Rates in older children are lower: 115 and 117 per million per year for those ages 5 to 9 and 10 to 14 years, respectively (eFig. 444.3  ).2
).2
Rates of childhood cancer can vary between and within countries. For example, the rate of childhood cancer reported for Canada was 158 per million per year for males, with a variation of 108 to 171 between provinces. In the United States, SEER data reports a rate of 163 per million per year for boys, with the within-country rate ranging from to 216. In Europe, rates range from 114 to 250 for boys.7 Hence, within Europe and North America, the incidence of childhood cancer varies by a factor of around 2 between countries and communities. The reasons for these variations are not well understood and are likely to include differences in genetic susceptibility and environment and lifestyle. 
TRENDS IN INCIDENCE 
The extent to which childhood cancer rates have increased in more recent decades is unclear.
In the United States, SEER data for 1992 to 2004 showed no significant trends. However, there was an incidence of all pediatric tumors of around 0.4% per year (95% CI, –0.1 –0.8%) and of leukemia of 0.7% per year (95% CI, –0.1–1.5%).8 That there is no evidence of a change in the rate of cancer in children in Canada between 1995 and 2004.2 The Automated Childhood Cancer Information System (ACCIS) group reported increased rates of childhood cancer of around 1% per year using data from 63 European population-based registries.9 In the United Kingdom, there have been reports of increasing rates of solid tumors in the north of England, with rates of increase being different between tumor types and between boys and girls.10
SURVIVAL
For many kinds of childhood cancer, the development of multimodal therapies, including surgery, chemotherapy, radiotherapy, and stem cell transplantation, has led to dramatic changes in outcome over the last 50 years.
Five-year survival from childhood cancer was 82% for children in Canada who were diagnosed between 1999 and 2003.2 For the majority of childhood cancers, 5-year survival is high (leukemia, 85%; lymphoma, 89%; central nervous system and brain tumors, 75%). For neuroblastoma and bone tumors, survival remains lower, at around 70% (eTable 444.2  ).2 Survival for childhood cancer altogether and for the individual diseases varies greatly across countries. For example, there are substantive differences in survival across Europe (eFigs. 444.4 and 444.5
).2 Survival for childhood cancer altogether and for the individual diseases varies greatly across countries. For example, there are substantive differences in survival across Europe (eFigs. 444.4 and 444.5  ).12
).12
SURVIVORSHIP
The majority of children treated with cancer in the developed world will survive their disease and its treatments. However, survivors carry with them a health burden due to the initial disease and to its treatments.13 For example, relapse of the first cancer can occur after more than 20 years, and the risk of a second primary tumor is at least four times greater than the general cancer risk to the population. This risk increases with the intensity, duration, and types of treatment. 
CAUSES AND RISK FACTORS
In adults, the majority of cancers arise from lifelong over- or underexposure to cancer-causing or cancer-protective factors. The process of carcinogenesis is complex and multi-factorial; seldom is there a single cause, children have had little opportunity to accumulate such lengthy and diverse exposures, and, just as the cancers themselves differ between adults and children, the causes also differ. There are a few rare genetic syndromes that result in an increased susceptibility to childhood cancers.  Children with congenital anomalies such as urogenital tract anomalies and Wilms tumor also have an increased risk of developing certain cancers. However, these conditions together likely account for less than 5% of all childhood cancers, and, with the exception of bilateral retinoblastoma, there is very little evidence of heritability of childhood cancer.15
Children with congenital anomalies such as urogenital tract anomalies and Wilms tumor also have an increased risk of developing certain cancers. However, these conditions together likely account for less than 5% of all childhood cancers, and, with the exception of bilateral retinoblastoma, there is very little evidence of heritability of childhood cancer.15
Despite a substantial body of epidemiological investigation into the etiology of childhood cancers, especially over the past four decades, the causes of the vast majority of cases remain unknown. 
There have been several reviews of the role etiological factors play in childhood cancer—especially leukemia. However, it is outside the scope of this chapter to review the substantial body of work in this area.16-18
 IONIZING RADIATION
IONIZING RADIATION
Ionizing radiation can cause cancer in adults and in children. It was first postulated as a cause of childhood cancer by Alice Stewart. She found that children whose mothers had been given x-rays during pregnancy were around two times more likely to develop leukemia and solid tumors than those whose mothers had not been exposed.19
There is little evidence that exposure to natural radiation (eg, to the radioactive gas radon) causes childhood cancer, though it is considered to be the second major cause of lung cancer after smoking and accounts for some 15% of lung cancer cases worldwide.21-23 However, it is extremely challenging to estimate lifelong radon exposures, even in children, in whom the time scales are necessarily shorter; therefore, reliable estimates of exposure are challenging to assemble.
While radiation can cause both hematologic and solid cancers in children,  overall radiation exposure to mothers and their children is too low to account for more than a very small fraction of childhood cancer cases.
overall radiation exposure to mothers and their children is too low to account for more than a very small fraction of childhood cancer cases.
 INFECTION
INFECTION
The role of infection and the infective process remains a focus for etiological studies of leukemia and other tumors. For leukemia, there is a sizeable body of evidence to suggest unusual patterns of antigen exposure plays a role,24 and evidence from twins and examination of blood samples taken early in life suggests that leukemia-related genetic changes occur in utero.25
 OTHER CAUSES
OTHER CAUSES
Many studies have explored the association between cancer risk and exposure to potential carcinogens such as pesticides, herbicides, tobacco, some recreational drugs, and so on. In general, associations have been weak and not consistent between studies, and no single exposure has been indentified as causal in a sizable proportion of childhood cancer cases.26
REFERENCES
See references on DVD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


