Acute Liver Failure
Vicky Lee Ng
Liver failure is defined in adults by the requisite hallmarks of the presence of hepatic encephalopathy and uncorrectable coagulopathy within 8 weeks of the development of clinical jaundice, in the absence of known preexisting chronic liver disease. In children, a modified working definition for pediatric acute liver failure has been achieved by consensus of an expert panel (the Pediatric Acute Liver Failure [PALF] Study Group) as follows:
1. No known evidence of chronic liver disease.
2. Biochemical evidence of acute liver injury.
3. Hepatic-based uncorrectable coagulopathy defined as an international normalized ratio (INR) greater than or equal to 1.5 (approximate to a prothrombin time [PT] ≥ 15 sec) in the presence of clinical hepatic encephalopathy OR (3a) an INR ≥ 2.0 (approximate to PT ≥ 20 sec) without hepatic encephalopathy.1
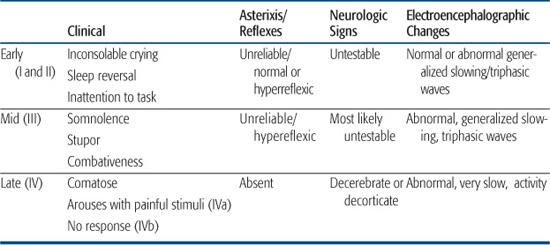
These modifications to the definition for pediatric acute liver failure notably recognize the difficulty of detecting hepatic encephalopathy, particularly the earlier stages, in infants and small children; markers of liver synthetic failure, such as an uncorrectable coagulopathy, as important indicators of liver failure even in the absence of hepatic encephalopathy; and children presenting in acute liver failure may in fact have a chronic liver condition not previously suspected or known. A clinical coma grade scale has been adapted for infants and children under the age of 4 years (Table 424-1).2
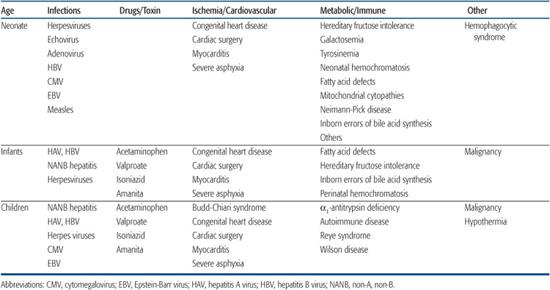
The approach to the child with acute liver failure should include the following: (1) establishment of an accurate diagnosis; (2) provision of intense, comprehensive medical supportive therapy; (3) anticipation, prevention, and timely treatment of complications, which may preclude the realization of spontaneous recovery; and (4) early referral to a liver transplant center, prior to the onset of complications of multiorgan failure, to assess both for indications and contraindications to liver transplantation. The causes of acute liver failure in children include a variety of age-dependent etiologies (Table 424-2). The diagnostic evaluations for these disorders is discussed elsewhere.
Table 424-1 Assessment of Encephalopathy for Young Children: Birth to Age 3 Years
SUPPORTIVE MANAGEMENT
Complications are common and can involve every organ system (Table 424-3). The child is best served if complications are anticipated and prevented. Death is usually attributable to cerebral edema with or without herniation, massive hemorrhage of the upper intestinal tract from stress injury, sepsis, or multisystem organ failure.3
 CARE ENVIRONMENT
CARE ENVIRONMENT
The child with acute liver failure should be cared for in a pediatric intensive care unit that allows close serial observation with surveillance for potential life-threatening complications, yet provides a quiet environment with minimal stimulation to prevent increases in intracranial pressure. Enteric isolation procedures must be enforced, and blood specimens should be labeled as potentially infectious. All medical personnel should consider wearing protective gowns, gloves, and masks when dealing with a child in acute liver failure.
 MONITORING AND BASIC CARE
MONITORING AND BASIC CARE
Venous access must be established immediately. The older and larger patient with aggressive delirium is a particular risk to care providers, and restraint and sedation may be necessary to protect staff. A central venous catheter is useful for assessment of central venous pressure and maintenance of volume status and euglycemia (targeting serum glucose levels between 110 and 130 mg/dL). Serial surveillance of electrolyte concentrations, body weight, and strictly maintained records of intake and urinary output are needed to evaluate fluid status and guide fluid requirements, which may be in the range of 85% to 100% of maintenance fluids. Close attention to the onset of renal dysfunction is warranted, as overzealous use of diuretics, (used to treat edema or ascites), or the use of nephrotoxic antibodies may be potential precipitants of dehydration, acute tubular necrosis, or functional renal failure (hepatorenal syndrome). Hypotension should be treated promptly. The use of “renal doses” of dopamine may help to maintain renal perfusion. When urine output decreases to less than 1.0 mL/kg/hour, it may become impossible to maintain fluid balance, and consideration should be given to begin renal supportive therapy, such as continuous venovenous hemofiltration.
A nasogastric tube may be passed electively in the patient with altered mental status and a poor gag reflex, and used for regular gentle saline lavage to detect upper gastrointestinal hemorrhage. Placement to gravity is helpful to avoid the gastric mucosal lesions associated with intermittent suction. Gastric pH is maintained above 4.0 with intravenous proton pump inhibitor agents (eg, pantoprazole 1 to 1.5 mg/kg/day IV daily) or an H2 receptor antagonist to prevent gastrointestinal bleeding.
 NEUROLOGIC MONITORING AND MANAGEMENT OF ENCEPHALOPATHY
NEUROLOGIC MONITORING AND MANAGEMENT OF ENCEPHALOPATHY
Neurovitals and frequent evaluation of neurologic function is essential to monitor the progress of hepatic encephalopathy. Gastrointestinal hemorrhage, infection, constipation, sedatives, electrolyte imbalance, hypoglycemia, and hypovolemia may precipitate encephalopathy and should be identified and corrected. Sedation usually is not needed, and the use of benzodiazepines should be avoided. Flumazenil, a benzodiazepine antagonist, may reverse early hepatic encephalopathy. Morphine or other opiates used in small doses can relieve pain associated with monitoring and catheter placement.4
Hyperammonemia is associated with the development of encephalopathy that may respond to lactulose at a dose that results in one to two loose stools per 8 hours. Mechanical ventilation is initiated for hypoxia or evidence of progressive coma and respiratory compromise. Mannitol should be considered with changes detected on neurologic examination or the onset of papilledema. The doses of mannitol required are usually in the range of 1.0 g/kg every 2 to 6 hours. Serum osmolarity should be monitored during mannitol therapy and should not exceed 320 mOsm/kg. Mild hypothermia may also be considered for the treatment of increased intracranial pressure (ICP).
 MANAGEMENT OF COAGULOPATHY
MANAGEMENT OF COAGULOPATHY
Aggressive attempts to correct coagulopathy with fresh frozen plasma may be warranted for the child who is clinically bleeding or for whom invasive procedures are anticipated, with attention to avoiding fluid overload and hypernatremia. Blood infusions are given to correct volume deficits from identified hemorrhage, and to maximize oxygen delivery to tissue. Vitamin K supplementation should be administered to any child with coagulopathy. Nutritional support must continue for these critically ill patients. Initial protein intake should not exceed 1 g/kg/day. However, prolonged protein restriction may be unnecessary, and greater amounts of protein are used if serum ammonia levels remain in an acceptable range.
Table 424-2. Conditions Associated with Acute Liver Failure at Different Ages
 INFECTION
INFECTION
Susceptibility to infection is common and a result of poor host defenses. Daily surveillance cultures from all indwelling catheters are recommended. Blood and urine cultures should be obtained with any significant changes in clinical condition. Ascites may be a site for secondary bacterial or fungal infection, and a diagnostic paracentesis should always be considered to evaluate for spontaneous bacterial peritonitis. Sepsis is the most frequent severe infection, with the most frequently implicated organisms being gram-positive (Staphylococcus aureus, S epidermidis, and streptococcus) organisms, presumably of skin origin. Occasionally gram-negative bacteria or fungal infections are observed. Urinary tract infections (complicating indwelling catheter use) and pulmonary infections are also common. Positive cultures in the absence of clinical infection should result in removal or replacement of the infected catheter and a brief course of empiric use of antimicrobials may be justified if sepsis is suspected, with attention to the possibility of additional, perhaps opportunistic, infection. Avoidance of antibiotics with nephrotoxic effects such as aminoglycosides is recommended if at all possible. An infant with multisystem organ failure and liver failure may have herpes simplex infection and should be treated with acyclovir until results of viral cultures are known.
 OTHER COMPLICATIONS
OTHER COMPLICATIONS
Significant pancreatitis, if present, may contribute to pain, hypotension, and disturbed calcium homeostasis, and monitoring of serum amylase is recommended. Bone marrow failure, a relatively common and usually ultimately fatal complication of acute liver failure associated with non-typable hepatitis, has been postulated to result from hepatitis viral infection of bone marrow elements. Although it may not be evident before transplantation, low blood counts should prompt an evaluation for potential bone marrow failure.
TREATMENT OPTIONS FOR ACUTE LIVER FAILURE
The mortality rate is high for patients with acute liver failure. At present, liver transplantation holds the greatest life-saving potential for patients with acute liver failure but the decision process regarding listing a patient for possible transplantation, and proceeding with transplantation if a donor organ is available, is complex. The cause of the acute liver failure is an important factor in determining whether transplantation therapy should be utilized (see also Chapter 130). Patients with drug-induced liver disease such as that caused by acute acetaminophen intoxication have good outcomes with intensive medical therapy and the early use of targeted therapy with N-acetylcysteine (NAC). On the other hand, children with acute liver failure secondary to an indeterminate cause or Wilson disease should be immediately offered liver transplantation. However, even in the current era of liver transplantation as primary treatment of acute liver failure for those who do not undergo spontaneous recovery, many patients die either as the result of complications of this devastating disease or because of lack of available donor organs in a timely fashion. Continued efforts to identify methods to improve hepatocyte function and patient survival are clearly needed.
Although NAC is proven therapy for acute and chronic acetaminophen hepatoxicity via replenishment of mitochondrial and cytosolic glutathione stores and prevention or amelioration of the degree of liver injury and cell death, there are currently no data supporting its empiric use in children with acute liver failure not resulting from acetaminophen overdose. Forthcoming results from a double-blind, placebo-controlled, randomized trial of intravenous NAC as treatment in children with acute liver failure not resulting from acetaminophen toxicity will hopefully provide guidance to this specific and important question. As a bridge to transplantation, experimental treatment strategies have included growth hormone, plasmapheresis, antioxidants, and other cytoprotective agents, along with temporary “bioartificial” liver support. The latter includes perfusion of plasma through a matrix of hepatocytes derived from human or porcine cell lines or hepatocyte transplantation. The use of auxiliary grafts, living related donors, and split livers may help improve the outcome for children with liver failure.5
Table 424-3. Complications in Acute Liver Failure



