Ectopic Pregnancy
Mary E. Rausch
Andrew M. Kaunitz
Kurt Barnhart
The term “ectopic pregnancy” (EP) refers to any pregnancy resulting from the implantation of a fertilized ovum outside of the uterine cavity, most commonly in the fallopian tube. Although EPs account for approximately 2% of pregnancies, the true incidence is difficult to ascertain given the underreporting of EPs treated in outpatient units (1). The most concerning acute danger of an EP is tubal rupture with massive intra-abdominal hemorrhage, and this is a leading cause of first trimester morbidity and mortality (2). EP resulted in 7% of all pregnancy-related deaths between 1991 and 1997, with 85% to 92% of fatalities secondary to hemorrhage (3).
Pregnancy-related deaths associated with an EP are on the decline, likely because of earlier detection and treatment (3). One half of deaths could have been prevented by more prompt diagnosis and treatment of EP by health professionals, and one third of deaths could have been prevented by more prompt notification of a physician by the patient (4). Although the average age of women with an EP is 28 years, the mortality rate is highest for teenagers (4). Misdiagnosis of a gastrointestinal disorder, intrauterine pregnancy (IUP), or pelvic inflammatory disease (PID) is common in this setting.
ETIOLOGY
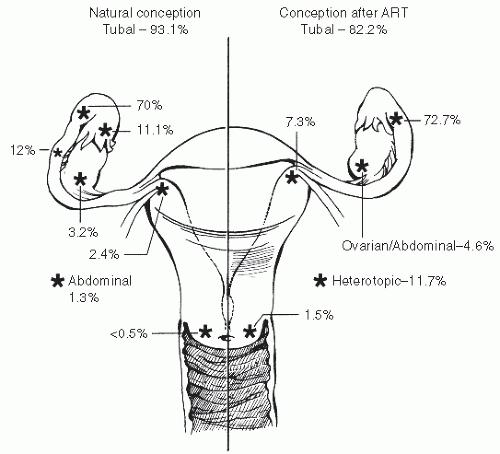
Of the 96% of EPs found in the fallopian tube, 70% are ampullary, 12% isthmic, 11% fimbrial, and 2% interstitial, with extratubal sites being rare (5) (Fig. 3.1). The tube serves a complex function in the process of fertilization and transport of the oocyte from the ovary to the uterus, where the blastocyst implants. At ovulation, the fimbriated end of the fallopian tube picks up the expelled oocyte with its cumulus mass of follicular cells. Conduction of the egg toward the uterus is thought to be effected primarily by the negative tubal intraluminal pressure generated by muscular contractions, with a secondary contribution from ciliary beating. Impaired muscular contractions, loss of ciliary action, or physical blockade could therefore prevent the embryo from reaching its normal location in the uterus. Tubal transport takes approximately 3 days, with fertilization occurring in the ampullary portion of the tube. Damage to the tube from prior infection, surgery, or tubal pregnancy can therefore subsequently increase one’s risk of future EP (6,7,8) (Table 3.1). A woman who experiences one EP has an increased risk of a second; women with an EP are 2.4 to 25 times as likely to have had a prior EP (8).
Although any form of contraception decreases the overall risk of pregnancy including EP, when contraceptive failure occurs in women using an intrauterine device (IUD) or following tubal sterilization, the risk of EP is elevated (7,9). With the copper T, approximately 6% of failures represent ectopic implantations (10). With the levonorgestrel IUD, this percentage is approximately 50 (11). Other factors in the history which may be associated with risk of EP include a history of salpingitis, tubal infertility, and DES exposure (6,7).
Among patients presenting to the emergency room with an early symptomatic pregnancy, the incidence of EP was lower for adolescents than adults (9.7% versus 21.7%) (12) and younger women (<25 years old) (8). However,
adolescents with EP present more often than adults with pain and a positive chlamydia and/or gonorrhea culture and less often with the classic risk factors of prior EP and prior pelvic surgery (12).
adolescents with EP present more often than adults with pain and a positive chlamydia and/or gonorrhea culture and less often with the classic risk factors of prior EP and prior pelvic surgery (12).
CLINICAL PRESENTATION
Although the classic signs and symptoms of EP are pain, amenorrhea, and vaginal bleeding, this diagnosis should be suspected in any reproductive-age woman presenting with pain or abnormal bleeding, as well as in women with symptoms of shock. The character of the pain is often nonspecific and may be diffuse, unilateral, bilateral, or even contralateral to the side involved. In tubal pregnancies, the pain may begin as vague lower abdominal discomfort that later becomes sharp and colicky as periodic tubal distention occurs. By contrast, the pain associated with the spontaneous abortion of an IUP is usually central and is likened to that of labor or menstrual cramps. Tubal rupture may be accompanied by a significant hemoperitoneum, resulting in poorly localized abdominal pain. Shoulder pain is possible secondary to phrenic nerve irritation when blood contacts diaphragmatic surfaces.
Although a history of recent amenorrhea is common in women with EPs, it is not unusual for a patient initially to deny having missed any menstrual periods. On a careful review, however, the most recent period may be described as lighter or abnormally timed, perhaps representing pathologic bleeding from decidualized endometrium. The abnormal vaginal bleeding reported by women with EPs is usually mild. Heavy bleeding or passage of clots is distinctly atypical and is more characteristic of inevitable or incomplete abortion of an IUP.
TABLE 3.1 Risk Factors for EP | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Factors in the patient’s history may increase the physician’s suspicion for EP. Questions regarding prior tubal surgery, pelvic infections, history of infertility, and type of birth control are appropriate. Current data indicate an ectopic rate for conceptions after the use of assisted reproductive technologies (ARTs) comparable to the estimated incidence of EP in the United States of 2% (13), but one third of conceptions resulting from sterilization are EPs (14). A history of induced or spontaneous abortion does not eliminate the possibility of an EP.
It should be stressed that history and physical findings, although necessary and important for assessing the patient and planning the appropriate follow-up and treatment, are not sufficient for exclusion or confirmation of an EP diagnosis (7). It should also be noted that whereas certain elements of the history may be more suggestive of a spontaneous abortion, such as heavy bleeding, passing of tissue, or midline cramping, they can also be found in some patients ultimately found to have an EP (7). Ultrasound in conjunction with human chorionic gonadotropin (hCG) levels may provide a definite diagnosis, and in stable patients in whom the diagnosis is uncertain, close follow-up is warranted.
DIFFERENTIAL DIAGNOSIS
The clinical presentation of a patient with an EP can mimic a number of other gynecologic and nongynecologic disorders (Table 3.2). Because most of these disorders are not immediately life threatening, it is important that the clinician excludes EP when considering these and other conditions in a woman of reproductive age with abdominal pain or abnormal bleeding. In addition, EP must be immediately suspected in a woman of reproductive age who presents with signs of hemorrhagic shock. The list of differential diagnoses can be easily separated
into those associated with pregnancy and those that usually are not. Of course, a positive pregnancy test does not eliminate the possibility that the patient could have another process occurring in addition to pregnancy.
into those associated with pregnancy and those that usually are not. Of course, a positive pregnancy test does not eliminate the possibility that the patient could have another process occurring in addition to pregnancy.
TABLE 3.2 Differential Diagnosis of EP | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||
Functional ovarian cysts are common in reproductive-age women. Rupture or torsion of an ovarian cyst can cause lateral pelvic pain, mimicking EP. A ruptured, hemorrhagic corpus luteum cyst can occur with both IUP and EP. It may be extremely difficult to differentiate an EP from a ruptured corpus luteum of pregnancy because pain and bleeding can occur with both, as well as evidence of hemoperitoneum. Although pelvic sonography may be able to demonstrate an intrauterine gestation, the presence of a substantial hemoperitoneum may mandate surgical intervention (15).
Nonviable IUPs are readily confused with ectopic gestation. Vaginal bleeding with threatened, inevitable, or incomplete abortion is usually described as being much heavier than a menstrual period, and the pain is often reported to be midline, similar to menstrual cramps or labor. If the abortion is indeed inevitable or incomplete, the cervical os may be noticeably dilated, with extruding tissue or clot. A decidual cast may be shed in patients with an EP and may be confused with products of conception associated with an incomplete abortion. If possible, all tissue passed by the patient should be examined. While an experienced observer may be able to identify the presence of chorionic villi without microscopy, false-positive results have potential life-threatening consequences. The histological presence of chorionic villi obtained from the uterus/cervix, or passed vaginally by the patient virtually excludes the diagnosis of EP. The use of serial quantitative serum hCG titers and transvaginal sonography to distinguish viable IUP from nonviable IUP and EP is discussed below.
Pelvic pain and abnormal vaginal bleeding may also occur with salpingitis (PID). Usually, the pregnancy test will be negative, and fever and leukocytosis will be present. In rare cases, PID can occur in the presence of a very early pregnancy. Gastrointestinal disorders including appendicitis are also included in the differential diagnosis of EP.
AMBULATORY EVALUATION
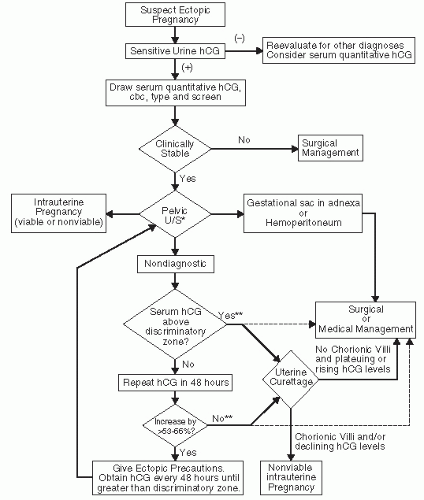
Diagnostic modalities available in ambulatory settings can expedite the diagnosis of EP, minimizing this condition’s morbidity, mortality, and cost. The initial evaluation of any woman of reproductive age complaining of abdominal pain or abnormal vaginal bleeding should include a directed gynecologic history, a physical evaluation, and a sensitive and rapid urine pregnancy test. An algorithm for the evaluation and management of suspected EPs is presented in Fig. 3.2.
History
An appropriate interview in this setting focuses not only on the nature of the pain but also on menstrual history, sexual activity, contraceptive use, prior pregnancies, and gynecologic disease. Pain is a common symptom with EP, and it varies considerably in clinical presentation, owing to the duration of the gestation, the site of implantation, and the existence of rupture and a hemoperitoneum. A history of amenorrhea or abnormal vaginal bleeding may be difficult to elicit in some patients. It is imperative that the timing and character of the last two or three menstrual periods be investigated through direct questioning. Finally, attention must be paid to the obstetric and gynecologic history, particularly with regard to known risk factors for EP.
Physical Examination
The physical examination of the patient with an EP varies, depending on the gestational age and the presence of rupture with a resulting hemoperitoneum. The physical exam should include vital signs, with attention to orthostatic changes in pulse and blood pressure, as well as abdominal and pelvic examinations. Tachycardia or hypotension can indicate hypovolemia due to intra-abdominal bleeding, but this can also occur in patients with spontaneous abortions due to vaginal bleeding as well as in patients with IUP who have a ruptured corpus luteum cyst or hyperemesis (7). Orthostatic changes and narrowed pulse pressure are unusual except in the case of massive intra-abdominal bleeding.
On abdominal exam, tenderness is the most common physical finding. The tenderness is classically unilateral and in the lower quadrant, but it can be bilateral. Rebound tenderness, guarding, and rigidity are not usually present except in cases with significant hemoperitoneum. Peritoneal signs are not commonly found in patients with EP but, when present, are predictive of EP (7,16).
A speculum exam of the vagina should be performed, looking closely at the source of any bleeding, the amount of blood present, and the presence of tissue at the cervical os. A bimanual pelvic exam will allow estimation of uterine size, determination of cervical dilation, and evaluation of the presence and tenderness of adnexal masses. A pelvic mass is found in the minority of patients with EP and is not predictive of EP—in fact, most of the patients with a palpable mass have an IUP, with the mass likely representing a corpus luteum cyst (7). Given the potential risk for tubal rupture and subsequent hemoperitoneum with a digital vaginal exam, some authors have suggested that the limited additional diagnostic information obtained may not warrant the hazards of performing the exam in patients with suspected EPs, especially in light of the diagnostic capability of ultrasound and serum hCG levels (17).
A minority of EPs result from implantation in the interstitial portion of the oviduct or in the uterine cornu. These cases characteristically present at a more advanced gestational age. On examination, the uterus is enlarged to a degree consistent with an uncomplicated IUP, and fetal heart motion may be detected. These patients may have only vague pain and an unimpressive examination until rupture occurs, at which time they often present with hypovolemic shock.
Pregnancy Tests
Given that the differential diagnosis for abnormal vaginal bleeding with or without pain in a woman of reproductive age is dependent on knowing her pregnancy status, a screening urine pregnancy test should be done as part of the initial evaluation. This will facilitate more timely diagnosis and minimize the risk of misdiagnosis. Using currently available urine pregnancy tests, 54% of tests are positive 11 days from the LH surge, and 98% are positive 14 days from the LH
surge (18). However, these data are from normal pregnancies and may vary for abnormal pregnancies. Some women with EPs will have hCG titers below that detectable by even the sensitive urine screening tests. To exclude this remote possibility, a serum hCG should be obtained in a woman with a presentation consistent with EP despite a negative urine pregnancy test.
surge (18). However, these data are from normal pregnancies and may vary for abnormal pregnancies. Some women with EPs will have hCG titers below that detectable by even the sensitive urine screening tests. To exclude this remote possibility, a serum hCG should be obtained in a woman with a presentation consistent with EP despite a negative urine pregnancy test.
Ultrasonography
Once a symptomatic patient is known to be pregnant, vaginal ultrasound plays a key role in differentiating first trimester pregnancy pathology. Hardware for performing vaginal ultrasound is becoming more accessible in emergency departments and physician’s offices, and the finding of an IUP on ultrasound virtually eliminates the possibility of an EP as heterotopic pregnancies are rare. Caution should be exercised in patients whose pregnancies are the result of ART, however, as the rate of heterotopics in these patients may be as high as 1% (19), although more recent data estimate the heterotopic pregnancy rate in the United States to be 0.15% for patients undergoing ART (20).
Accurate gestational age is the best determinant of when an IUP should be seen within the uterus, and a gestational sac or sacs should be visible by approximately 5 weeks on transvaginal ultrasound (21). In the absence of proper gestational dating, a discriminatory zone, or level above which a normal IUP should be visible, can guide management. Transvaginal ultrasound is more accurate and diagnostic of both IUPs and EPs than is transabdominal ultrasound (22) and is therefore the modality of choice. A commonly accepted cutoff for visualization of IUP via transvaginal ultrasound is 1,500 to 2,500 IU/L (23), although this may vary between institutions depending on the hCG assay as well as the equipment and experience of the sonographer. In the situation of multiple pregnancies, the hCG values are higher than singletons for any given gestational age and may reach well above 2,000 IU/L before ultrasound recognition of the pregnancy. Accordingly, the hCG level should be interpreted with caution in situations where multiples may be expected, as with the use of infertility treatment.
Although an IUP should be identified when the hCG level is above the discriminatory zone, ultrasound may provide useful information in symptomatic women whose hCG levels are below this level. In two studies of women ultimately found to have EPs, 39% with hCG <1,000 mIU/mL (24) and 42% with hCG <1,500 mIU/mL (25) were diagnosed on initial ultrasound. Free fluid can give insight into the presence and degree of hemoperitoneum, and alternative sources of pain, such as adnexal pathology, can be found. However, looking at all women who present with symptomatic pregnancies below the discriminatory zone, only 14% of women were diagnosed accurately and definitively with initial ultrasound. To avoid interrupting a desired viable pregnancy or subjecting the women to unnecessary surgery, caution must be exercised when correlating ultrasound findings with hCG values when the latter are found to be below the discriminatory zone (25).
When performing a transvaginal ultrasound, the bladder should be empty. First, the clinician should evaluate the uterus for the presence of a gestational sac. A gestational sac is defined as a central sonolucency surrounded by an echogenic ring, which can be detected when it reaches the dimensions of 2 to 3 mm (Table 3.3). Gestational sacs 5 mm or greater in dimensions can consistently be imaged using vaginal ultrasound (21




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree