Imaging in Gynecologic Emergencies
Marcia E. Murakami
Joseph G. Cernigliaro
Ultrasound is the most useful imaging modality in the evaluation of gynecologic emergencies. Moreover, ultrasound does not pose the risk of ionizing radiation, which is a consideration when examining the potentially pregnant patient. Transvaginal imaging, in particular, permits exquisitely detailed examination of the uterus and ovaries, so that a specific diagnosis can often be made with great confidence. Plain radiographs are rarely useful as the initial screening study. Computed tomography (CT), in selected cases, can provide more global information for extensive disease, especially when the pathologic process extends out of the pelvis.
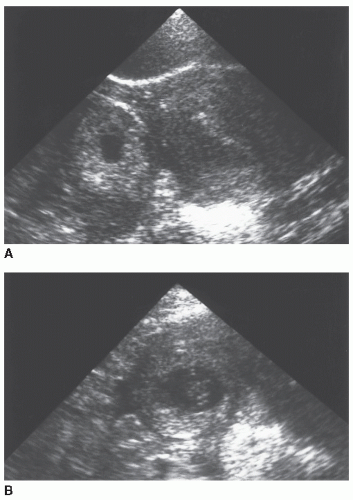
Although some authors think that transvaginal scanning (TVS) alone is sufficient for defining pelvic pathology (1,2), it is our view that transabdominal scanning (TAS) should be performed first. For patients who are suspected of having an emergent gynecologic problem, the sonographer quickly scans the upper abdomen to exclude free intraperitoneal fluid, which is highly suspicious for hemoperitoneum in this patient population. Scanning through the urinary bladder affords a wide field of view and a survey of the entire pelvis. Although the diagnosis often can be made using TAS alone (Fig. 28.1), TVS almost always follows to better characterize the transabdominal findings (Fig. 28.2). The transvaginal examination is therefore directed and performed with the confidence that pathology is not outside the limited field of view of the transvaginal probe. Other authors suggest that TVS may be performed first, with addition of TAS as needed (3,4,5).
THE PREGNANT PATIENT
The development of an accurate and rapid pregnancy test has narrowed the differential diagnosis of otherwise nonspecific clinical findings. Still, the list of diagnostic possibilities in the early stages of pregnancy remains long and includes intrauterine pregnancy (IUP), ectopic pregnancy, embryonic or fetal demise with missed or incomplete abortion, completed abortion, and molar pregnancy. Ultrasound can make a specific diagnosis in a number of cases or at least aid in the clinical management of the patient. Establishing the presence of a normal IUP essentially excludes an ectopic pregnancy. Evaluation of the gestational sac and its contents can often confirm embryonic demise. Often, correlation of the ultrasound findings with the clinical history may strongly suggest incomplete or completed abortion.
Normal Early IUP
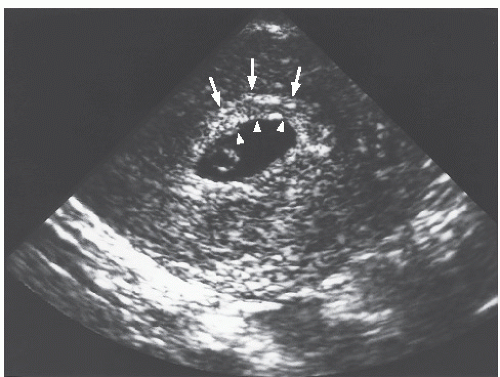
At the time of implantation, between day 20 and day 23 (menstrual age), the conceptus is only about 0.1 mm in diameter (6), much too small to be detected by transabdominal or transvaginal probes. Focal echogenic thickening of the endometrium can be visualized at the implantation site between 25 and 29 days. The earliest that a sac may be seen within the uterus is at 3.5 weeks, as a tiny anechoic fluid collection within the thickened decidua, termed the
intradecidual sign (Fig. 28.3) (7). More commonly, an early gestational sac is reliably detected at approximately 4.5 weeks’ menstrual age by TVS and at 5 weeks’ menstrual age by TAS (8). Correlation with serum human chorionic gonadotropin (hCG) levels is extremely helpful. Sac detection discriminatory levels of 1,800 IU/L (Second International Standard [2nd IS]) or approximately 3,600 IU/L (International Reference Preparation [IRP]) TAS (9,10,11) and 1,000 IU/L (2nd IS) or about 2,000 IU/L (IRP) TVS (10,11) have been established. (The 2nd IS is approximately half the IRP value.) At these levels or higher, a definite intrauterine gestational sac should be visualized. Below
these levels, a normal intrauterine gestation may be too small to detect. If the hCG level is disproportionately low relative to the gestational sac size, an abnormal pregnancy should be suspected (9). In general, the intrauterine findings of an early pregnancy are visualized on TVS approximately 1 week earlier than on TAS (12).
intradecidual sign (Fig. 28.3) (7). More commonly, an early gestational sac is reliably detected at approximately 4.5 weeks’ menstrual age by TVS and at 5 weeks’ menstrual age by TAS (8). Correlation with serum human chorionic gonadotropin (hCG) levels is extremely helpful. Sac detection discriminatory levels of 1,800 IU/L (Second International Standard [2nd IS]) or approximately 3,600 IU/L (International Reference Preparation [IRP]) TAS (9,10,11) and 1,000 IU/L (2nd IS) or about 2,000 IU/L (IRP) TVS (10,11) have been established. (The 2nd IS is approximately half the IRP value.) At these levels or higher, a definite intrauterine gestational sac should be visualized. Below
these levels, a normal intrauterine gestation may be too small to detect. If the hCG level is disproportionately low relative to the gestational sac size, an abnormal pregnancy should be suspected (9). In general, the intrauterine findings of an early pregnancy are visualized on TVS approximately 1 week earlier than on TAS (12).
The double decidual sac sign (13) may be the earliest confirmatory sign of an IUP on TAS or TVS (Fig. 28.4) (14,15). Although a definite double decidual sac sign is not identified in all normal IUPs, when this sign is clearly present, it is a very useful indicator of IUP (16). It is based on the visualization of the chorionic cavity
surrounded by two layers of echoes, the inner echogenic ring representing the decidua capsularis and chorion and the outer echogenic ring, the decidua parietalis. The combination of the gestational sac plus the decidual layers forms a much larger complex than the chorionic cavity itself and may be more readily identified at an earlier stage.
surrounded by two layers of echoes, the inner echogenic ring representing the decidua capsularis and chorion and the outer echogenic ring, the decidua parietalis. The combination of the gestational sac plus the decidual layers forms a much larger complex than the chorionic cavity itself and may be more readily identified at an earlier stage.
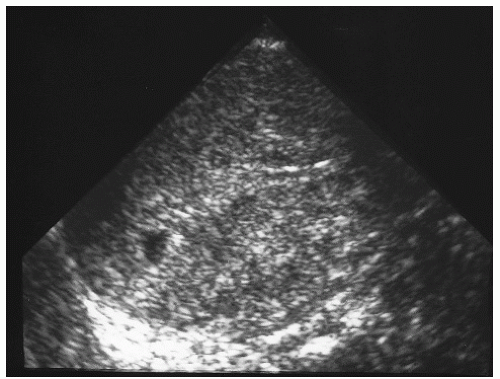 FIGURE 28.3 Intradecidual sign. The very small eccentric fluid collection within the decidua represents a very early (<4-week) IUP. |
Normally, the yolk sac is the first structure seen within the gestational sac (Fig. 28.5). It should always be visualized with a mean sac diameter (MSD) of 20-mm TAS (17) and 8-mm TVS (18). (The MSD is calculated by dividing the sum of the three orthogonal dimensions of the fluid sac by three.) Whereas the double decidual sac sign is not absolutely specific for an intrauterine gestation, the presence of a yolk sac is definitive (14). Between 5 and 10 menstrual weeks, a yolk sac should never exceed 5.6 mm in diameter (19). As early as 5.5 weeks, a second sac may be seen adjacent to the yolk sac. This second sac represents the amnion, and this, together with the yolk sac, forms the double bleb sign (20). The embryonic disc lies between the two sacs. The amnion continues to grow and eventually fills the chorionic cavity by weeks 14 to 16. Normally, the amnion may be seen as a separate membrane until this time (Fig. 28.6).
Once a yolk sac is visualized within the gestational sac, a search should be made for an embryo immediately adjacent to the yolk sac (Fig. 28.7). Transabdominally, pulsation of the embryonic heart may be identified at real time, establishing a
live pregnancy, even though a distinct embryo is not visible (21). An embryo should always be visualized with an MSD of 25-mm TAS (9) and 16-mm TVS (10). An embryo is consistently detected transabdominally once it has reached a crown-rump length ≥5 mm. Cardiac activity is often visible transvaginally in embryos with a crown-rump length of 2 to 4 mm (about 6 weeks). However, TVS can identify normal embryos without cardiac activity when they are <5 mm (22). The absence of cardiac activity in these small embryos should not be construed as embryonic demise.
live pregnancy, even though a distinct embryo is not visible (21). An embryo should always be visualized with an MSD of 25-mm TAS (9) and 16-mm TVS (10). An embryo is consistently detected transabdominally once it has reached a crown-rump length ≥5 mm. Cardiac activity is often visible transvaginally in embryos with a crown-rump length of 2 to 4 mm (about 6 weeks). However, TVS can identify normal embryos without cardiac activity when they are <5 mm (22). The absence of cardiac activity in these small embryos should not be construed as embryonic demise.
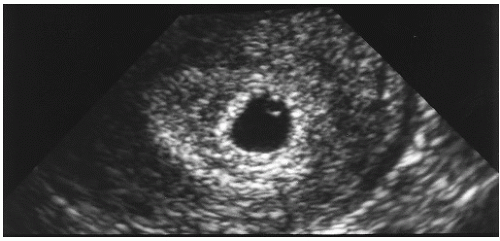 FIGURE 28.5 Yolk sac. Perfectly spherical, thin-walled yolk sac is noted in the periphery of the gestational sac. The 10-mm MSD corresponds to a 5-week gestation. Note the double decidual sac sign. |
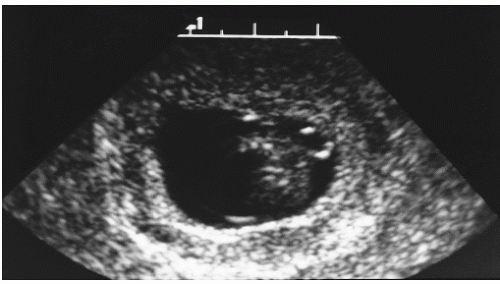 FIGURE 28.6 Yolk sac and amnion. The delicate amniotic sac envelops an 8-week embryo. The amnion has not yet fused with the chorion. Note the yolk sac adjacent to the embryo. |
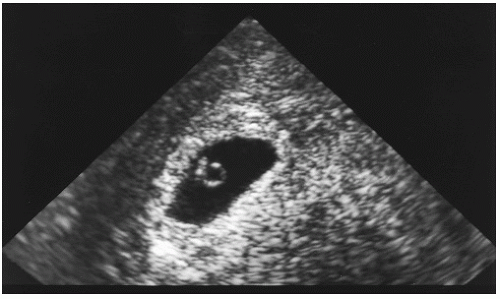 FIGURE 28.7 Embryo. Gestation of 5.5 weeks (13-mm MSD) with yolk sac and adjacent embryo. Cardiac activity was present. |
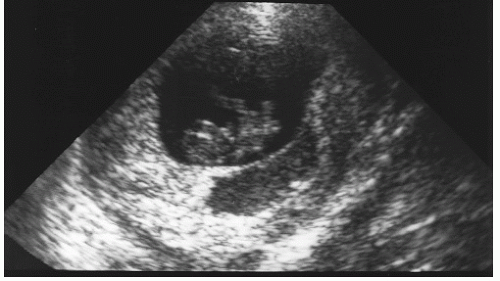 FIGURE 28.8 Subchorionic hemorrhage. A 9.5-week living IUP in a patient who was first seen with acute vaginal bleeding. Hemorrhage is more echogenic than the fluid within the gestational sac. |
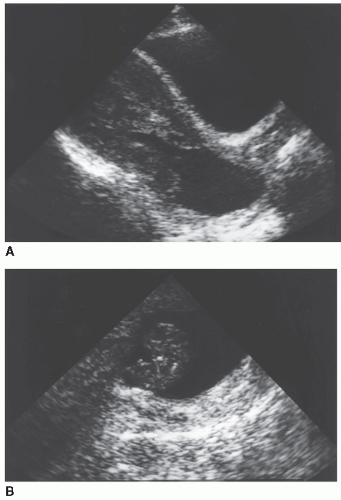
Subchorionic hemorrhage is a common finding late in the first trimester and may be associated with vaginal bleeding. The hemorrhage causes elevation of the chorionic membrane, appearing acutely as a fluid collection more echogenic than amniotic fluid (Fig. 28.8), becoming more hypoechoic in 1 to 2 weeks. The significance of these hematomas is somewhat controversial. Some researchers believe that the prognosis depends on the volume of the hemorrhage, with a
better prognosis associated with the smaller hematomas. Others suggest that the vast majority of pregnancies with subchorionic hemorrhage detected before 20 menstrual weeks end in a normal term delivery (23).
better prognosis associated with the smaller hematomas. Others suggest that the vast majority of pregnancies with subchorionic hemorrhage detected before 20 menstrual weeks end in a normal term delivery (23).
Corpus luteum cysts are commonly detected in the first trimester. The cysts may be simple or hemorrhagic (Fig. 28.9). They are usually 3 to 6 cm in size but may be as large as 10 cm. These cysts usually resolve spontaneously by 16 weeks.
Abnormal Early IUP
Ultrasound has proved to be extremely helpful in the evaluation of the failed pregnancy. With TVS, a single examination is often conclusive in establishing embryonic demise. A large gestation sac (MSD, >25-mm TAS [9] or >16-mm TVS [10] without an embryo; MSD, >20-mm TAS [9] or >8-mm TVS [10] without a yolk sac) is diagnostic of an anembryonic gestation or blighted ovum (Fig. 28.10). Distorted gestational sac shape is also highly specific for abnormal pregnancy, although it is a somewhat subjective feature and is relatively insensitive. Suggestive but less specific findings include a thin (<2 mm), weakly echogenic or irregular choriodecidual reaction, absent double decidual sac sign, and low position of the sac within the endometrial cavity (9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree