Vertebral Subluxation Complex
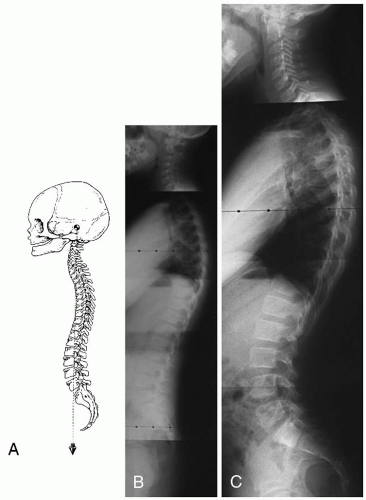
The vertebral subluxation complex (VSC) has a number of components (
25,
26,
27,
28,
29). The spinal changes associated with the VSC include kinesiologic, myologic, neurologic, and histologic factors.
Hildebrandt (
19) has reviewed the clinical basis for chiropractic spinography. Chiropractic spinography can be defined as a roentgenological diagnostic procedure that uses postural (weight-bearing) x-rays for the principal purpose of evaluating the spinal column and pelvis for evidence of clinically significant biomechanical irregularities (
19). The use of x-ray examination in the chiropractic profession dates back to 1910, when B.J. Palmer initially used the device as a research tool to evaluate the accuracy of spinal palpation. In later years, the x-ray was used as a common diagnostic procedure for the detection of abnormal spinal biomechanics (
30).
Global postural spinal problems can be examined through external postural analysis and global range of motion assessed through goniometry (
25,
26,
27,
28,
29,
31). However, global assessments are limited because they primarily evaluate the extrinsic spinal musculature. The intersegmental biomechanical effects on the ligamentous elements, fixation dysfunction, normal motion, and instability—in fact, all intersegmental phenomena—can be more accurately assessed with plain film techniques (
32). No alternative and less invasive procedures are currently available to the practicing chiropractor for accurate assessment of the intersegmental kinesiologic components of the subluxation complex.
Clinical research and observation suggests spinal biomechanical compromise can occur in utero (constraint positions) or as a result of birth trauma (
21,
32,
33). Multiple microtraumatic episodes and macrotraumas can occur in the child throughout spinal development. During the formative years, shear stress deformities, changes in the instantaneous axis of rotation, and altered intersegmental biomechanics create the environment for abnormal vertebral cartilaginous and osseous remodeling, resulting in permanent structural deformity (
34).
Radiographs should not be used independently to rule out the presence of a joint abnormality (i.e., subluxation) requiring an adjustment. As with most diagnostic tests, plain film is great for the interpretation of some things and completely unnecessary for others. To evaluate the multiple-component nature of the subluxation, tests should be weighed differently when evaluating particular patients, spinal regions, or injury scenarios. The clinical and/or symptomatic picture should always be correlated with radiologic findings because the subluxation is a multivariate complex. The practitioner should first find the location (i.e., segmental level) of the joint abnormality on the patient and not on the radiograph. Factors that are proposed to be weighed heavily in the clinical examination are the presence of edema, tenderness, and joint fixation.
Prevention of Deformity and Injury Chiropractic care may be more effective if it prevents the VSC from causing the development of permanent osseous of soft tissue asymmetry (
12). The pediatric spine is particularly vulnerable as the cartilage of the fetus makes its transition to bone in the adult. In some families, there may be genetic predilection for the development of certain spinal problems.
To the extent possible, applying preventive adjustments to motion segments that may not yet be symptomatic could have the potential for minimizing abnormal cartilage and bone formation during the growth of the child. This logic applies as well to the promotion of certain exercises or postural practices and the limiting of others.
Some spinal anomalies can best be detected through plain film. Low cost combined with minimal risks, when used judiciously, makes plain film examination the imaging modality of choice in most circumstances. The presence of a small cervical central canal, measured from the lateral cervical radiograph, should alert the attending clinician and athlete that certain sports, in which the potential for neck trauma is high, must be avoided (
35).
Ligamentous Injuries The onset of disc degeneration in the early stages often corresponds with the onset of symptoms (
36), although some individuals will experience no symptoms. In these patients, early signs of spinal degeneration such as retrolisthesis or disc dehydration can only be determined through objective analytical procedures, such as plain film radiography or MRI, combined with palpatory signs of inflammation such as edema or tenderness.
In low back disorders, the first pathological changes occur in the annulus. These early changes take the form of small circumferential separations between the annular lamellae. Evidence of lamellar separation has been reported as early as 8 years of age (
36). In the vast majority of disc injuries, healing occurs in the form of granulation tissue and vascularization. The new blood supply comes from the outer annulus and the end-plate (
36,
37).
Recent advances in imaging technology have allowed better visualization of ligamentous structures, such as the intervertebral disc. Paajanen et al. (
38) used MRI to study disc degeneration in young patients with low back pain. The average age of the patients was 20 years. Fiftyseven percent of those suffering from low back pain had one or more abnormal lumbar discs. A control group of pain-free individuals was also analyzed with MRI. Approximately 35% of these individuals showed signs of degeneration. End-plate changes, detected radiographically, were associated with disc degeneration. Therefore, damaged end-plates are likely to be one etiological and/or associated factor in the development of disc degeneration. Many of the MRI-detected abnormal joints had no marked radiographic changes. Early degenerative disc disease may exist long before thereis loss of disc height
or other obvious radiographic findings of degenerative joint disease (
39).
Paajanen et al. (
38) did not evaluate subtle postural changes with plain film radiography, nor movement abnormalities. Because disc degeneration begins at an early age, it is important for the chiropractor to direct into the motion segment adjustments that do not cause further stress to the annular fibers. The avoidance of long axis rotational forces is one method for reducing the chance for disc injury with an adjustment (
40).
Incorporating alignment and movement considerations during the delivery of an adjustment will less likely result in ligamentous injury to the spine. Ligamentous damage could result from a misdirected thrust by moving the joint further into the direction of ligamentous sprain (i.e., into the direction of hypermobility) or potentially could cause a separation of the endplate at its attachment to the disc.
Low Back Problems Pellise et al. (
41) assessed the prevalence of low back pain in a cohort of 1,470 adolescents with a mean age of 15.05 years (SD, 1.17 years). Low back pain was reported by 39.8%. Olsen et al. (
42) assessed the prevalence of low back pain in a cohort of 1,242 adolescents (aged 11 to 17 years). Approximately 30% of the adolescents had low back pain. One-third of the individuals with low back pain reported restricted activity and 7.3% sought medical attention. Based on the results of the investigation, the authors suggested that low back pain is a serious public health problem. If one-third of the adolescent population is experiencing symptomatic back problems, others may have underlying subclinical pathology (i.e., subluxation with only mild sprain). Low back pain is a frequent reason for adult patients to seek chiropractic care, and “spinal manipulation” has received endorsement as an efficacious treatment from two independent reviews (
43,
44).
Plain film radiography is a highly efficient means for detecting subtle alignment changes in the spine, thought to be of importance to chiropractors when directing treatment for patients. In addition, tropism, transitional segments, lumbar scoliosis, and leg length inequality are all structural entities that are readily identifiable with plain film and that can alter both the direction and site of a high-velocity, low-amplitude thrust and other treatments (e.g., heel lift). The presence of these structural changes in the low back also impacts the clinical diagnosis and prognosis of the patient. Although the findings that typically are seen on plain film radiographs of patients with low back pain are not necessarily relevant to a practitioner of internal medicine or a physical therapist because they will do little to direct the approach to treatment, these findings do have direct applicability to the adjustment/management issues facing the chiropractor (
6,
15).
Clinical Examination Spinal trauma will usually result in signs of inflammation, especially over the posterior aspect of the spinous processes where ligamentous sprain injury caused by hyperflexion moves the supraspinous ligament through the greatest arc of motion. The presence of the signs of inflammation may warrant radiographic examination. Signs of inflammation include palpable spinal tenderness (
45), edema, or erythema. Palpable tenderness is relatively reproducible in interexaminer reliability experiments (
45,
46).
When physical abnormalities such as skin temperature asymmetries (
47,
48,
49), the red response (
50), or skin texture abnormalities suggestive of autonomic disturbances or denervation supersensitivity (
51,
52) exist, then radiographs are usually indicated for the assessment of other components of the subluxation, such as alignment and movement changes (
15). These palpatory and instrument findings, indicative of inflammation or subclinical neuropathology, should guide the clinician toward further investigation (e.g., plain film) to address the need, if any, for the application of a specific adjustment.
Asymptomatic Subluxation The chiropractic paradigm incorporates the idea that abnormal spinal function, such as reduced movement (
20,
53,
54,
55) or alignment abnormalities (
56,
57), are significant and warrant chiropractic intervention (i.e., adjustment). The argument that early chiropractic intervention should be used, regardless of whether a patient has symptoms, lends support for the use of objective means of assessment, such as plain film radiography. Exacting analysis and treatment theoretically could avert more serious problems later or alleviate currently silent nerve pathology, thus influencing the general health of the patient. Long-term prospective investigations will need to be performed to address the salient issues surrounding the asymptomatic spinal subluxation and its putative effect on general health outcome measures (e.g., the quality and quantity of life).
Kinesiopathology Kinesiopathologic factors associated with spinal trauma include intersegmental postural and movement abnormalities as well as global assessments of spinal function and posture. Abnormal patterns of movement, compensatory hypermobility because of fixation dysfunction, and spinal and pelvic misalignments (i.e., positional dyskinesia) are entities that should be scrutinized carefully when evaluating the spinal column for signs of trauma or functional disturbances.
Fixation Dysfunction If movement irregularities, such as a reduction in global range of motion or intersegmental abnormalities such as fixation dysfunction or hard
end-feel, are present, then radiographic assessments are usually indicated because there is likely to be adjustive intervention for these dysfunctions (
15). The information derived from the radiograph is likely to be useful in the delivery of care (i.e., ruling out contraindications, identifying anomalies, and determining patterns of thrust consistent with improved biomechanics). Limited information is available on the use of various radiographic findings as outcome measurements. Bronfort and Jochumsen (
31) report on a series of patients with low back pain in whom functional radiographic examinations of the low back were obtained. An analysis of a subset of the cohort of adults who had low back pain and received spinal adjustments demonstrated improvements in intersegmental motion after treatment.
Positional Dyskinesia
Upper Cervical Spine Biedermann (
21), a manual medicine practitioner, studied biomechanical problems (i.e., subluxation) of the upper cervical spine in newborns. Approximately 135 babies who were available for follow-up were reviewed in the report. The babies were referred to the author because of asymmetrical posture, and the case histories included the following disturbances:
Tile posture of the head or torticollis
Head tilt during flexion
Uniform sleeping patterns; the child cries if the mother tries to change its position
Fixation of the sacroiliac (SI) joints
Extreme sensitivity of the neck to palpation
Loss of appetite
The symptoms described by the patients’ parents could be caused by a variety of pathologic conditions. Biedermann (
21) states that if motor asymmetries, sleeping alterations, or facial scoliosis are present, then the suboccipital articulations should be evaluated for blockages (i.e., fixation dysfunction). He also advocates the use of plain film radiographs for determining malalignment of the suboccipital region and for determining the appropriate vector of force during the adjustment. In addition, the radiograph is used for the detection of malformations. Biedermann (
21) states that basing treatment on information not taken from the radiograph is why his colleagues probably do not have as favorable results. A high proportion of the newborns in this study experienced prolonged labor times during delivery when compared with normal babies. Most patients only required one to three adjustments before remission of symptoms occurred. However, no long-term follow-up of these patients was reported. These findings parallel the clinical observations of many practicing chiropractors and indicate that chiropractic care for newborns is promising. Further research on suboccipital subluxation, including prospective controlled studies, should be undertaken to control for the natural history of these disorders.
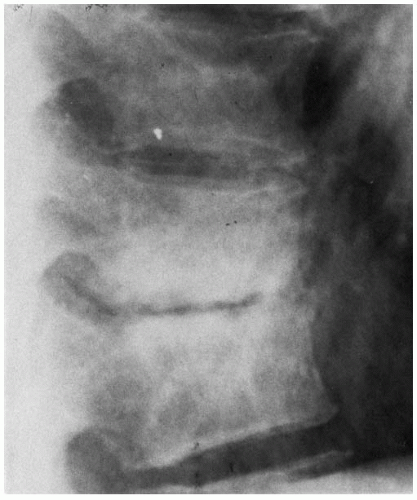
Lumbar Retrolisthesis Plaugher et al. (
56), in a retrospective consecutive case analysis of pretreatment and comparative radiographs from 49 adult outpatients attending a chiropractic clinic, found that retrolisthesis of the L5 or L4 vertebra was reduced about 34% after an average of eight adjustments directed at the level of displacement. No statistically significant change was detected in a retrospective control group. The doctor whose records were scrutinized usually performed comparative evaluations just before the 10th visit and the patients usually continued care on an individual basis after this comparative analysis. Twenty-five patients who entered the clinic between January 1, 1986, and March 1, 1986, had their records added to those of another 25 patients who entered the clinic between April 1, 1986, and June 1, 1986. Because of poor quality radiographs in one case, a total of 49 patients were analyzed. There were 31 women (63%) and 18 men (37%). The mean age was 44 years (SD, 20 years). The most common complaint at entrance was low back pain, which occurred in 79% of the population. Fifty-three percent of the patients had mid-back or neck symptoms. Sixty-four percent of the patients had referred pain to either shoulder or upper and/or lower extremity. Fortyseven percent of the patients had viscerosomatic or somatovisceral symptoms. Patient complaints included headache, constipation, dysmenorrhea, shortness of breath, and nervousness.
Sacral Base and Lumbar Lordosis Angles In the aforementioned study (
56), measurements were also made of the sacral base angle and the lumbar lordosis angle in the adult patients. No statistically significant changes were observed before or after treatment. The length of time between analyses was about 1 month and occurred before the 10th office visit. The use of these radiologic parameters as outcome measurements in short-term trials (i.e., <1 month) of chiropractic adjustments is questionable.
Banks (
57) has shown that reduction of the hyperextension component of the lower lumbar motion segments is readily attainable in adults with side posture manipulation. A statistically significant decrease in the average disc angle at the involved level was detected in his sample of 13 patients, with clinical diagnoses of facet syndrome (i.e., hyperextension of the lower lumbar and lumbosacral disc spaces with concomitant facet jamming).
Cervical Lordosis Plaugher et al. (
56) observed no significant change in the cervical lordosis after examination of the initial and comparative radiographs. On average, six and a half cervical and upper thoracic adjustments
delivered between the initial and comparative radiographs. All patients who reported for care were analyzed, regardless of the level of adjustment.
These findings contrast with the results of Leach (
58), who showed significant improvement in the cervical lordosis after treatment, in the magnitude of 2 to 5 degrees. Because Leach’s study did not evaluate the reliability and examiner measurement error of his analysis, these results can be questioned.
Giesen et al. (
59) evaluated radiographic findings in children with hyperactivity disorder as part of a smallscale time-series study of seven patients. A moderate level of correlation was found between radiographic findings before treatment and baseline skin conductance levels. In four of the seven subjects, the number of positive x-ray findings reduced after specific adjustive treatment.
A case report has been presented by Thornton (
60) of a 13-year-old patient with a cervical kyphosis. Three specific adjustments to the atlas subluxation was followed by a complete return of the normal cervical lordosis.
Harrison et al. (
61), in a preliminary study of adult patients, evaluated the efficacy of cervical extensioncompression traction in the restoration of the cervical lordosis. Treatment was approximately 3 to 4 months. Their pilot study demonstrated a positive effect of this treatment on the lordosis. The addition of supine-positioned diversified spinal manipulation, including lateral flexion and rotational forces combined with prone drop-table adjustments, did not enhance the effect demonstrated with extension-compression traction treatment alone. The results of this study should provide the impetus for a large-scale, controlled clinical trial. Research should also focus on the type and duration of treatment that is most effective in restoring the cervical lordosis. Comparison clinical trials of different techniques should be a high priority for the chiropractic profession.
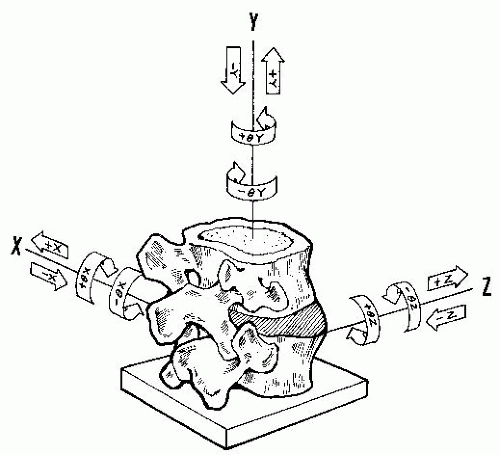
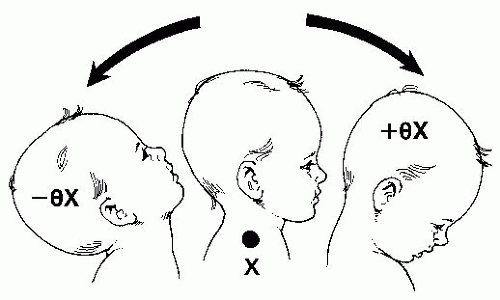
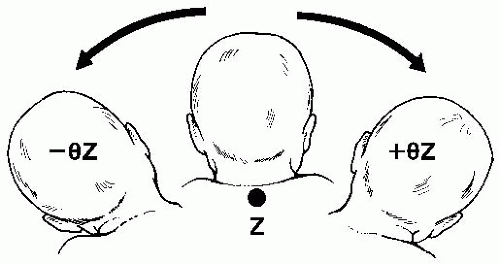
Coronal Plane Spinal Posture Grostic and DeBoer (
62), using a retrospective design, compared atlas laterality (±θZ) after specific adjustments. The data, from a sample of 523 case files, tended to show a reduction in this type of displacement after chiropractic care. Plaugher et al. (
56) detected no changes in the posture of the shoulder girdle (42 patients) or scoliosis magnitude (18 patients) in their retrospective consecutive case analysis. These patients were primarily adults with scoliosis. Each patient received an average of eight adjustments between examinations. Although there are several case studies describing the role of chiropractic care in the patient with scoliosis (see
Chapter 14), more formal prospective trials are needed to adequately address the plethora of issues facing the attending clinician, especially in the case of mild curvatures (i.e., <20 degrees).
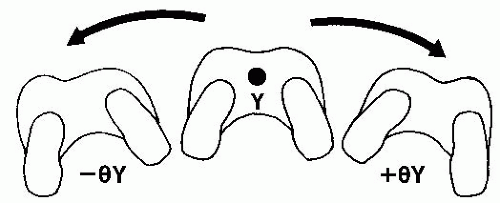
Transverse Plane Posture Grostic and DeBoer (
62), in a retrospective study of case files, found that Y-axis rotational subluxation of the atlas reduced after specific adjustments.
Leg Length Inequality In the pediatric patient, the clinical assessment of leg length is irrelevant for a newborn, someone who is nonambulatory, or in an active toddler who never stops moving. Most of the clinical application of leg length inequality evaluation pertains to the juvenile or adolescent.
Should leg length inequality be detected below the level of palpatory findings of injury, then radiographic assessment of the more caudad areas is often indicated (
15). This is because pelvic unleveling can cause compensational changes (i.e., scoliosis) in the spine above. Plain film usage must always answer the question of whether the information obtained is of clinical benefit. The findings from the radiographic examination are likely to alter the therapeutic course by providing alignment information.
The issue of whether leg lengths should be equal at a certain stage in a child’s life, considering the fact that leg length growth may be far from even, deserves discussion. Asymmetrical growth that evens out later should be balanced with the appropriate clinical goal of avoiding asymmetrical loading on the endplates during skeletal maturation, resulting in slight wedging of the vertebrae (i.e., Heuter-Volkmann Law) (
34). If orthotic inserts are prescribed, then follow-up with low-exposure radiographic investigation with the appliances worn needs to be performed to assess periodic and final leg length. All appliances, from heel lifts to orthotic inserts, must be continually posturally evaluated (iliac crest height) at each chiropractic visit during a child’s growth (
63). An appliance, if incorrectly applied, can cause permanent vertebral deformation through bone remodeling and asymmetrical epiphyseal plate growth (
34). The high prevalence of leg length inequality in adults (
64,
65,
66) should alert the clinician to the potential for this type of asymmetry in children.
Ionizing Radiation
Unfortunately, the various sorts of useful information derived from radiographs must be weighed against the harmful effects of ionizing radiation. There are potential negative biological effects of human exposure to ionizing radiation. Exposure effects are cumulative. The use of ionizing radiation in examining any patient, including children and adolescents, should be based on clinical need.
Growing concern for the hazards of ionizing radiation and the availability of alternative imaging techniques may cause our reliance on plain film to change. The best course to take is to minimize exposure by using the latest technology for patient protection. According to a recent National Research Council report, low doses of x-radiation pose a human cancer risk three to four times higher than previously reported. The report also noted that some fetuses exposed to radiation face a higher than expected risk of mental retardation (
74). Radiation protection is particularly important when x-raying infants, children, adolescents, and adults in their reproductive years. The effects of radiation on individuals with high rates of cellular division (i.e., children) are greater. The physician should always adhere to the principle of “as high as reasonably achievable” with regard to diagnostic yield, and “as low as reasonably achievable” with regard to radiation exposure. Retake examinations should be minimized.
How Much Radiation? With modern technology, the amount of radiation that patients receive has been substantially reduced (
75,
76,
77). Some sacrifice in film quality might be observed with the very high speed systems currently available (e.g., 1,200 RSV) (
78). This potential reduction in the clinical utility of high-speed systems, however, has not been subjected to scientific verification. A 400 to 800 screen/film speed (
79) coupled with a high frequency generator; high kilovoltage factors; shielding over the breasts, gonads, and eyes; and Niobi-X filtration (
12), produces dosages that are much less than previous technology could provide.
A report by Kalmar et al. (
80) states that use of higher kilovoltage, 1,200 high-speed screen systems, leaded compensation filters, and shielding of sensitive structures demonstrated an immediate dose reduction of approximately 75%, continuing to 95% before image quality became unreliable. They concluded that satisfactory image quality can still be obtained using readily available radiation reduction equipment.
There are several units of radiation measurement in common use. In English-speaking countries, the rad and rem are commonly employed, whereas most other countries favor the gray (Gy) and the sievert (Sv), from the International System of Units (SI). The unit of absorbed dose is the gray. One Gy is defined as 1 J of energy absorbed per kilogram of matter: 1 Gy = 100 rad. The unit of dose equivalent is the sievert: 1 Sv = 100 rem.
One rad is equivalent to 1,000 mRad. An anteroposterior (AP) full-spine x-ray exposed at 88 in. (224 cm) with a 1,200 speed system for an averaged size adult (77 kg) results in approximately 65 mRad of exposure (
81). It is not known how harmful this quantity of radiation is to adults or children because no long-term studies currently exist.
Genetic Effects To date, radiation-induced genetic effects from diagnostic radiography have not been directly observed in humans. The largest source of material for genetic studies involves the survivors of Hiroshima and Nagasaki, but the 77,000 births that occurred among the survivors showed no evidence of genetic effects (
82).
Pregnancy There is evidence that 1,000 mRad of exposure to a fetus during the first trimester of gestation will result in an increase in the prevalence of carcinoma by 0.6 deaths per 1,000 (
82). The occurrence of cancer death from natural causes is approximately 1.4 per 1,000. From 1,000 mRad of exposure during pregnancy, the occurrence of mental retardation and small head size increases. A pregnant woman should usually not be exposed to radiation unless the trunk and pelvis can be adequately shielded or if not performing the examination would jeopardize the health of the mother (
12,
83).
Cancer Little information exists about the effects of radiation from diagnostic x-rays on the incidence
of cancer among the general population. Evans et al. (
84) determined that radiation-induced leukemia represented approximately 1% of all cases. Less than 1% of all cases of breast cancer are caused by the effects of diagnostic radiography (
85). Evans et al. (
84) concluded that x-rays for diagnostic purposes have only a small influence on the occurrence of leukemia and breast cancer.
Thyroid neoplasms can result from exposure to high levels of diagnostic x-rays. Pillay et al. (
86) report on two patients who received between 90 and 525 rad of total exposure after an initial diagnosis of congestive cardiac failure at the age of 3 years. Radiographic procedures also included catheterization. Both children were diagnosed with thyroid cancer at age 14.
Chromosomal abnormalities associated with ionizing radiation have been reported, but these usually involve frequent repetition or extremely high radiation levels not typically encountered in diagnostic radiography (
12,
87,
88,
89).
Risk Assessment The scientific controversy surrounding the determination of the magnitude of the health risk from low-level radiation should not divert public attention from the fact that even conservative estimates place risks from radiation well within the range of risks from other perils that are considered acceptable. One approach to risk education is through the presentation of quantified risk estimates, such as one in a million chance of dying or a decrease in life expectancy as a result of exposure to a variety of hazards. The carcinogenic risk of radiation exposure is 100 to 200 deaths per million people exposed per rad per year. The exposure to a typical patient should be far <1 rad (see “How Much Radiation?” above) (
90,
91).
There is no conclusive evidence to show any shortening of the life span, even among radiologists who are exposed to much more radiation than would be received by a patient, as the result of diagnostic use of roentgen rays (
92).
Clinical practice guidelines produced by the PCCRP (
22) describe the two models of radiation effects on organisms: the linear no-threshold model and the radiation hormesis model. The linear no-threshold model is designed based on data derived from the atomic bombing of Japan. This model is used to estimate risks from low levels of radiation, such as diagnostic radiography. However, as previously noted, conclusive supporting data is lacking. The radiation hormesis model suggests that there may actually be health benefits associated with low levels of exposure to radiation. Using either model, the clinical benefits of appropriate diagnostic x-rays likely outweighs any risk.
The use of ultra-high-speed cassette/film and longwavelength filters will likely reduce the risks associated with further ionizing radiation exposure. Digital imaging systems and software have the potential to produce quality diagnostic film at low radiation levels. As with most controversial areas in health care, additional research will be needed before more accurate assessments of risks and benefits can be made for low levels of diagnostic radiation.
General Considerations Several inherent pitfalls are involved in imaging pediatric spines. Patient motion is an ever present problem. Even when short exposure times are used to limit the effects of motion on the finished radiograph, a true postural study may be difficult to obtain. Immobilization of an uncooperative patient can yield a film that is useful diagnostically, but may not accurately depict postural pathomechanics. If an unclear or improperly exposed film is likely to result from a particular examination (i.e., because of patient positioning difficulties), then that view should be omitted rather than exposing the child to unnecessary radiation. Radiographic procedures for children and adults should include every safety precaution to ensure the lowest possible exposure to ionizing radiation. Biological effects from exposure to ionizing radiation are both tissue and dosage dependent. The breast, eyes, and gonads are extremely sensitive to radiation and can be selectively shielded for many radiographic examinations. Taking appropriate safety measures (i.e., shielding), including the use of long film focal distances (FFDs), can significantly reduce the entrance skin exposure (ESE) to the patient (
93). The information that follows should be used as a summary guide for clinicians and technologists who perform x-ray examination so that the appropriate technical precautions are taken to minimize radiation exposure.
All doctors need to determine their clinical and diagnostic needs and then maximize the available equipment to minimize the radiation exposure to both the patient and the technician. As with any piece of equipment, regular calibration checks of the generator by an x-ray physicist is recommended (
94). During this check, re-alignment of the central ray to the cassette will minimize abnormal projection magnification.
Potential trade-offs should be considered when attempting to change radiographic technique. Two representative examples are presented:
Film-Screen Speeds Although an 800 to 1,200 film screen speed combination is sufficient for most radiologic assessments, especially in the case of a pediatric patient, there are situations when the need for detail may outweigh the benefit of reduced patient exposure (
12). This can occur when there is a potential spinal or extremity fracture in which the use of lower speed screens may be more appropriate for the issue of high detail. A careful history and physical examination will dictate which screen/film speed is most appropriate. The chiropractor can more effectively care for the individual patient by matching the appropriate system to the specific clinical presentation by having available one high-speed system of 800 to 1,200 for spinography and one slower-speed system, of 200 to 400, for more detailed evaluations (
12).
Presently, the fastest screen/cassette/film on the market was introduced by Kodak as a 1,200 speed system comprising Lanex Fast screen with Kodak PDH-1 film. It substantially decreases radiation exposure while producing a diagnostic quality image.
In the darkroom, some of the high-speed films (e.g., 1,200) are very sensitive to many light spectrums. The technologist should adhere to the recommended safety light provided by the manufacturer of the film. One can test a sheet of unexposed film by holding it up in the safety light. If the film develops clear, then the safety light spectrum is within the tolerance of the film.
Although not yet in widespread use, cassetteintensifying screens with a 1,200 screen/film combination speed are recommended for spinographic evaluation of pediatric patients to reduce ESE. Comparative radiographs and x-rays used to assess spinal motion should also have a minimum 1,200 screen/film speed.
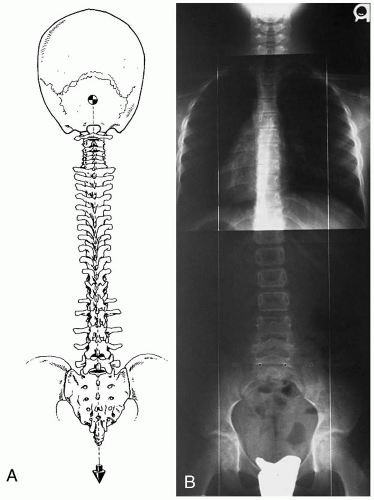
Film Sizes Depending on the child’s size, a smaller film size can be substituted for the standard 14 × 36 in. for full spine radiographs. The technician should measure from the occiput to the lower sacrum to include all sacral segments. Allowing for slight magnification of the image, if the measurement is <17 in., then a 14 × 17-in. film size can be used. Strict collimation should be used, excluding the skull and femurs from exposure. For sectional radiography or bending films, the smaller film sizes (e.g., 8 × 10, 10 × 12, or 14 × 17) are more appropriate.
If the entire spine needs to be imaged, then fullspine views are preferable to sectional studies because of the necessary overlap and double exposure in two regions of the spine (
12). Comparative dosimetric evaluations between full-spine and sectional radiography have shown lower exposure levels with full spine (
97). Phillips (
98) has reported on the comparative diagnostic utility of full-spine versus sectional radiographs. In a survey of Diplomates of the American Chiropractic Board of Radiology, it was judged that, although adult full-spine x-rays are inferior in the quality of diagnostic detail compared with sectionals, the diagnostic information/yield obtained from both procedures was essentially the same (
98).
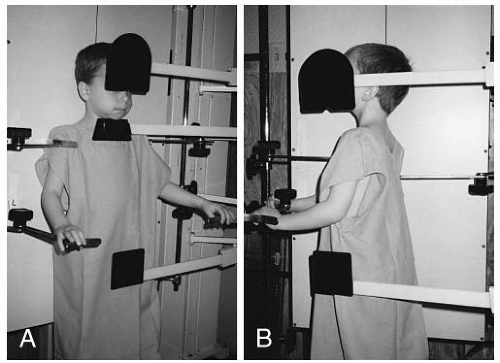
Positioning X-ray positioning demands can be challenging for a child. They may need to hold a stance or opposition that might be painful. Thoroughness during positioning is essential for radiographs obtained for the purpose of imaging spinal biomechanics. Positioning instructions should be carefully explained to the child and adapted so that the child can reduce motion artifacts and the need for unnecessary repeat radiographs. If a child cannot stand still (e.g., cerebral palsy patient or infant), parental assistance may be necessary. Lead shielding (e.g., apron, gloves) can be provided to the assisting parent. The assistance of an outside radiological facility may be necessary in some unusual circumstances.
Collimation The smallest possible collimation of the x-ray beam is preferred during the exposure. In addition to protecting the patient and the technician from excessive dosage, collimation also increases the quality of the radiograph by reducing the amount of scatter radiation, thus improving contrast and detail. Ideally, the exposed radiograph should have two edges that reveal the collimator (
99). It is not appropriate for the entire skull and three-fourths of the femurs as well as the lateral aspects of the trunk and arms to be exposed in a full-spine radiograph.
Shielding Shielding for the reproductive organs, thyroid gland, and bone marrow protection should be provided (
100,
101,
102). Because children undergo more rapid cellular division than adults, they are more susceptible to the mutagenic effects of ionizing radiation. Also, cellular compaction in most glands is greater in children than in the adult, causing a potentially greater proportion of risk per square inch of surface area exposed to ionizing radiation. Lead contact shields can be placed directly on the patient, especially in front of the eyes and gonads.
Breast tissue is very sensitive to radiation and must be shielded from the x-ray beam. This can be accomplished through collimator-mounted or contact shielding (
12) without compromise to spinal and pelvic evaluations.
The thyroid gland should be shielded whenever possible because of its high radiosensitivity (
86). Systems that offer partial shielding of this gland are currently available (
102) (
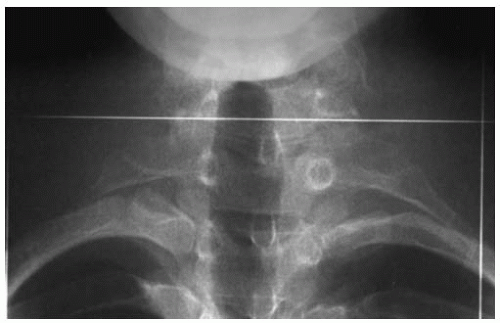
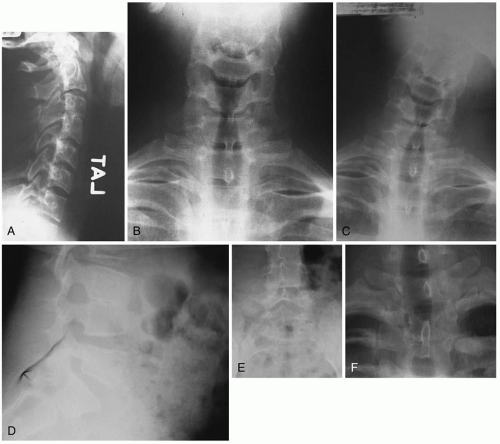
Fig. 4-1A,B).
Grids Grids reduce the amount of secondary exposure and improve the film quality. They are coordinated with the x-ray unit, depending on the highest kVp usually used. Because a high kilovoltage technique (e.g., 100-110 kVp) is recommended for most spinal column assessments because of the decreased entrance skin dose, a higher grid ratio of 10:1 to 12:1 is preferred (
12,
103).
Grids minimize scatter radiation by allowing most useful electrons to pass through perpendicular to the cassette, thereby increasing film clarity. Most grids are rated by the ratio of the depth of the grids to the width and the number of lines per inch.
Grid Focus A problem seen in some clinics can be the lack of coordination between the radiographic grid focus distance and tube distance. This distance should be known and strictly adhered to for optimum radiographs. It is the doctor’s responsibility to check this equipment requirement. Some technicians may not be aware of this important consideration during the initial equipment set-up, especially if unusual (but appropriate) distances are used during radiography (i.e., >84 in. for full spines) (
90).
Filtration Prepatient filtration is integral to producing good quality radiographs. Because of variances in size and density of various regions of the spine and pelvis, prepatient filtration can modulate the x-ray beam, thereby creating more uniform penetration. This is especially important when full-spine evaluations are being made.
Prepatient filtration systems that accommodate for tissue density and thickness have been used in the chiropractic profession and have improved diagnostic quality while at the same time reducing ESE (
104). Because no shielding contacts the patient, this filtration is hygienically positive. The radiation also is attenuated at the collimator. When properly used, pre-patient filtration focuses on the body part being studied and selectively minimizes radiation exposure.
Bucky Stand Shielding Bucky stand shielding is another quality barrier for scatter radiation reduction. Lead sheeting placed behind the bucky as close as possible to the cassette will minimize post-entry rebound scatter radiation. This is a relatively inexpensive safeguard.
Long Wavelength Filtration Long wavelength filtration, such as Niobi-X, is currently available (
12). The element niobium is used to reduce the low-energy, long wavelength radiation. At short FFDs, this type of filtration can substantially reduce exposure.
In the clinical arena, Niobi-X radiation filters significantly reduce the ESE. Field testing using the Kodak Lanex/PDH-1 film with the Niobi-X filter revealed an approximate 50% reduction of millirems (mR) compared with exposure without the Niobi-X filter. This Lanex/PDH-1 film with the NIOBI-X filtration combination equates to an approximately 90% reduction of mR in the AP cervical spine study with a patient who has 10 cm body part thickness when compared with the average of the Nationwide Evaluation of X-ray Trends tabulated by the Bureau of Radiological Health, January 1, 1981, to December 31, 1981 (
80,
105,
106).
Film Focal Distance The shorter the FFD, the more magnification of the patient on the radiograph. Shorter FFDs also result in more marked apparent distortions of patients when they have been improperly positioned for the exposure. As the distance between the tube and patient is increased, there is less angulation, or angle of inclination, between the focal spot and the object (
12). A longer FFD also results in less patient exposure and is therefore recommended (
107).
High-Frequency Generators Ultrahigh-frequency generators decrease exposure time and lower overall patient dose, as well as increase technical accuracy and consistency of imaging. These generators produce a higher quality image with greater image contrast detail (
12,
108).
Automatic Timers Automatic exposure timers have experienced a recent resurgence in popularity because of increased electronic technology. Each cassette houses a sensor that detects the pre-set radiation exposure required for an optimum exposure. Once the pre-set radiation has been sensed, a signal is sent back to the radiographic controller, which is attached to the generator, and the exposure is stopped. The timer allows an optimum kVp and mA setting for body density
and thickness, and the time is automatically stopped by the sensor. This equipment is most helpful for doctors who are meticulous about patient placement. The sensor must be located behind the object desired. Any deviation of the desired body part from the sensor will result in a substandard radiograph (
94).
Split Screens Non-homogeneous speed-intensifying screens (i.e., split screens) for full-spine radiographs can also compensate for regional variation in size, but result in more radiation exposure to the patient. Their use is outdated because of the advances made in prepatient filtration (
12). It is recommended that doctors currently using this technology switch to homogenous high-speed screen/film systems (e.g., 1,200 speed).
Processing Film processing chemistry must be carefully maintained. A properly performing circulation pump will keep the chemicals at the same concentration throughout the tank.
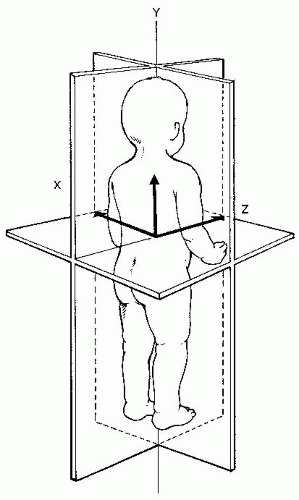
Patient Positioning and Equipment Alignment The x-ray beam must be perpendicular to the bucky and the patient. If the beam is not centralized, this will result in postural distortion of the area under examination. In addition, measurements of the pelvis, including the femoral heads, are affected from this offcentering. The pelvis is especially susceptible to rotational (Y axis) malpositioning (
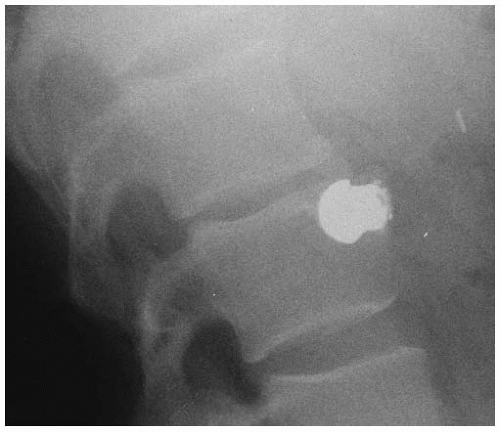
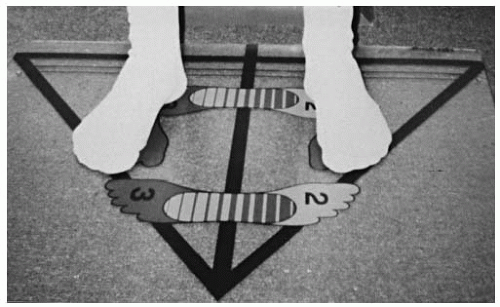
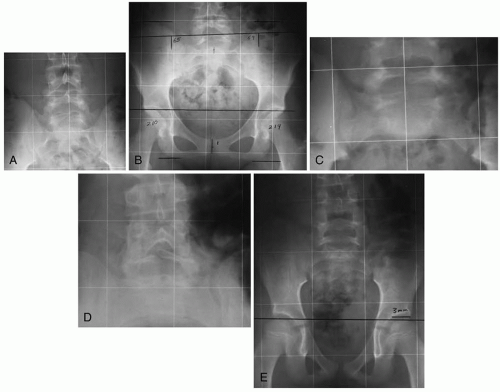
109). A foot positioning grid should be used to position the patient reliably on a level surface (
110,
111) (
Fig. 4-2).
The patient should always be positioned in the upright posture whenever possible. Recumbence tends to lessen the effects of gravity on the spine, minimizing displacements of the motion segments (
12,
112,
113).
For the toddler through adolescent, the patient’s heels are placed parallel to the bucky at one of three grid lines. The heels should be kept equidistant from the midline of the foot positioning grid and approximately 4 to 8 in. apart. The patient should be instructed to maintain their natural foot flare and to keep the knees in a locked position. A potential problem with foot placement markers is the tendency for patients to stand with their feet to match the marks, thus altering natural foot flare.
Immobilization straps attached to the bucky are available for stabilizing those patients who have tremor or sway while standing. These straps should be used only to stabilize and not to distort the patient’s normal gravitational standing posture.
When attempting x-ray examination of the pediatric patient, the doctor should explain carefully the procedures that are being performed. More time is needed for these examinations, especially in the case of the infant or toddler. An informed and cooperative child will minimize the potential for re-take examinations.
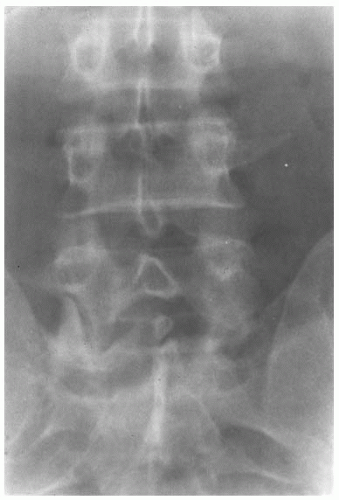
Congenital Variants
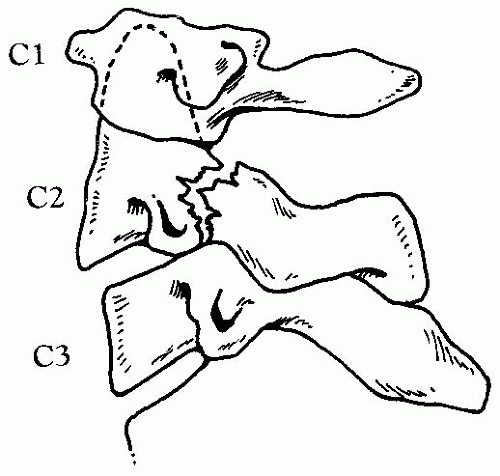
Non-segmentation A lack of segmentation of the primitive sclerotome results in a “block vertebra” (
Figs. 4-3,
4-4,
4-5). In the cervical spine, this occurs most frequently at the C5-C6 and C2-C3 levels. Non-segmented vertebrae appear structurally as one and function as one. Failure of the non-segmented vertebrae to contribute to the composite motion of the region affected may lead to hypermobility and degenerative changes at other segmental levels, often above the site of non-segmentation. When non-segmentation occurs at the occipitoatlantal articulation, the term “occipitalization” is applied (
Fig. 4-6). Although non-segmentation by itself rarely produces neurologic compromise, brain stem or cord compression have been reported in cases of upper cervical fusion (
119,
120,
121).
MacGibbon and Farfan (
122) studied various common anatomical variants demonstrable on plain films of the lumbar spine. Six hundred forty-two subjects were studied. The investigators reported that two main types of anatomic spinal variations are identified in the majority of individuals. The presence of L4-L5 injury and degeneration is likely to be associated with the following anatomical factors:
L5-S1 degeneration was associated with the following:
Down’s Syndrome Other variations may also occur in the upper cervical spine. In children, the atlantodental interspace should not exceed 5 mm (
1). An increase may be caused by congenital absence of the transverse ligament, as seen in Down’s syndrome. Although previously considered to be of little clinical significance, increased participation by such children in athletic activity (e.g., Special Olympics) requires careful assessment of the upper cervical spine. Radiologic studies, including flexion/extension views, are advocated for such children at about 2½ to 3 years of age to assess possible atlantoaxial subluxation (
123,
124,
125,
126). Juvenile rheumatoid arthritis or traumatic rupture of the transverse ligament may also result in an increased atlanto-dental interspace (
127,
128).
Odontoid Process Variations Variations also occur in the development of the odontoid process. The tip of the dens develops from an ossification center, which appears at age 2, and unites at 10 to 12 years. If such union does not occur, a terminal ossicle remains. If the dens remains ununited at its base, the condition is termed os odontoideum (
Fig. 4-8A-D). Instability and cord compression may result (
129). Hypoplasia or congenital absence of the dens may also occur, resulting in an unstable articulation (
130). Unstable os odontoideum, although rare, should be considered in the differential diagnosis of a child complaining of neck pain with decreased mobility. The diagnosis will be confirmed by stress radiographs taken in the extremes of flexion and extension (
131).
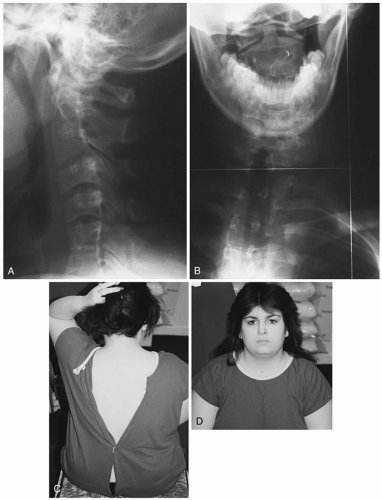
Klippel-Feil Syndrome This condition is characterized by multiple block vertebrae of the cervical spine. The
patient may present with a short neck, low hairline, and genitourinary anomalies. The condition predisposes the spine to injury and possible cord damage (
132) (see “Nonsegmentation,” above).
Sprengel’s Deformity Congenital non-descent of the scapula can often be detected clinically. Radiographs will demonstrate an omovertebral bone in 30% to 40% of cases (
133).
Cervical Ribs Ribs may arise from a lower cervical segment (
Fig. 4-9). These ribs may cause neurovascular compression (scalenus anticus syndrome) later in life, but are usually only contributing factors. In children, they are usually asymptomatic (
134).
Butterfly Vertebra A sagittal cleft in a vertebral body may occur, usually in the thoracic or lumbar spine. Most are asymptomatic and clinically insignificant (
135).
Hemivertebra Failure of the lateral half of a vertebral body to develop produces a lateral hemivertebra. The inevitable consequence is a scoliosis. Rarely, a dorsal or ventral hemivertebra occurs, which may cause an alteration of lordotic and kyphotic curves (
136).
Spina Bifida Occulta Spina bifida occulta is a failure of fusion of the posterior elements of a spinal segment without meningeal protrusion. It is often seen at the L5-S1 levels and is usually of little clinical significance (
Fig. 4-10A-E). It does not increase susceptibility to athletic injury (
124). Spina bifida is a serious condition in which there is protrusion of the spinal membranes, with or without cord tissue, through absent posterior vertebral arches.
Facet Tropism Asymmetry of the facets at the L5-S1 level may produce asymmetrical biomechanics and joint dysfunction (
137) (
Fig. 4-11). Their identification provides a more complete analysis for the purposes of motion palpation or motion x-ray interpretation.
Knife Clasp Deformity Spina bifida occulta in association with an elongated L5 spinous process may result in painful and limited extension (
138) (
Fig. 4-12).
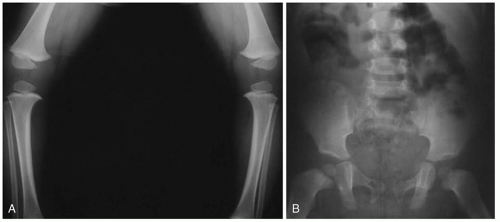
Congenital Hip Dysplasia Deformities of the acetabulum and dislocation of the femur from an anomalous acetabulum characterize this condition. Radiologic manifestations of congenital hip dysplasia were described by Putti (
141). Putti’s triad consists of a small or absent proximal femoral epiphysis, lateral displacement of the femur, and increased angulation of the acetabular roof.
Slipped Capital Femoral Epiphysis This condition is usually seen in children older than 10 years. It may be associated with a specific traumatic episode or may appear gradually. A limp with hip pain is the characteristic clinical presentation. Boys are more commonly affected than girls. Overweight children are also more likely suffer from this condition. Radiologically, a widening of the growth plate is seen initially. An abnormal relationship between the femoral neck and femoral head may be appreciated. This condition can also cause an aseptic necrosis of the femoral head with resultant deformity. AP and frog leg views are recommended in the assessment of slipped capital femoral epiphysis (
1).
Postnatal Abnormalities
“Pseudo” Subluxation The concept of a “pseudo” subluxation has been presented by many different authors throughout the years. The differentiating factor
in pseudo subluxation versus subluxation is that in the former the spinolaminar line is preserved and it is not in the latter. Physicians and radiologists learned early on the problems in mislabeling certain injuries that could have resulted in unnecessary surgical operations; these findings have more relevance to the practitioner using nonoperative methods (e.g., chiropractor). Some recent publications present radiographs diagnosed as pseudo subluxation. However, other biomechanical abnormalities are clearly of clinical use to chiropractors.
Since most patients are x-rayed because they have suffered a trauma to the spine or have pain, the labeling of a pseudosubluxation may be a result of poor interpretive skills (
142). Labeling something as normal when a clinical scenario is present does a disservice to the patient. The scenario of perhaps overdiagnosing spinal biomechanical abnormalities in children stems from the observation that many asymptomatic individuals exhibit similarly minimal findings. Radiographs should always be correlated with the presenting clinical picture. A “normal” radiograph in the presence of a symptomatic patient should not be weighed very heavily when resolving the lack of agreement between the two examinations. If the patient is asymptomatic, some of these findings may have less clinical relevance. Their potential effects on future spinal growth, deformity, or neurologic health should be carefully outlined to the patient or guardian.
Spinal Cord Injury Without Radiographic Abnormality Some patients with spinal cord injury will have “normal” or near normal radiographs. This is caused by the potential lengthening of the spinal column without a commensurate increase in the elasticity of the spinal cord. In cadaver studies it was determined that the canal can stretch up to 2 in. because of the elasticity of spine ligaments. The spinal cord can only stretch about a 1/4 in. before injury or rupture occurs (
143). This mismatching of elasticity accounts for, in part, neural injury seen in normal radiographic vertebral anatomy. Mechanisms for spinal cord injury without radiographic abnormality (SCIWORA) include simple anatomical differences as well as transient subluxation, reversible disc protrusion, vasospasm, and vascular occlusion. Dickman and Rekate (
143) have provided a list of the most possible mechanisms for SCIWORA (
Table 4.1).
Structural and Functional Variation In addition to structural variation, functional variation in the pediatric spine warrants careful consideration by the chiropractor. Sullivan et al. (
144) examined lateral cervical radiographs of 100 normal children and discovered that in 20% of cases, the C2 vertebra appeared subluxated anteriorly on the C3. This phenomenon is usually observed in children younger than 9 years of age and is caused by the more horizontal facet orientation in the younger child. It is particularly pronounced during flexion (
145). The preservation of the spinolaminar line differentiates true subluxation from pseudo subluxation (
146). Whether these “normal” findings represent early changes predisposing to subluxation degeneration
has not been explored. Following subjects with these purportedly “normal” pseudo subluxations throughout life and comparing the incidence of degenerative changes in the spine with controls is suggested as an area for additional research.
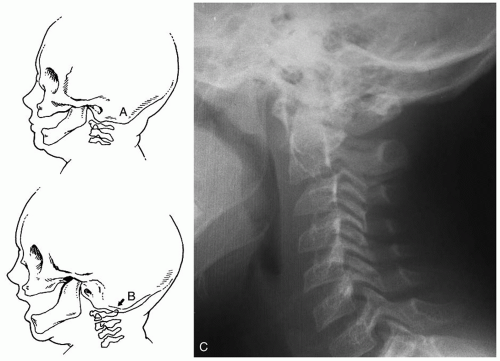
Atlanto-Occipital Hypermobility and Sudden Infant Death Syndrome A triple-blind study of sudden infant death syndrome (SIDS) and non-SIDS infants was undertaken by Schneier and Burns (
147). Analysis of radiographs of 53 infant cadavers revealed that in all cases in which the atlas inverted into the foramen magnum, SIDS was listed as the cause of death. However, not all SIDS infants exhibited atlas inversion. Atlas inversion is the condition in which the posterior arch of the atlas is positioned within the foramen magnum (
Fig. 4-13A,B). These investigators also reported that measurements made on neutral, flexion, and extension radiographs suggested that a correlation may exist between atlantooccipital hypermobility and SIDS. Some cases of atlas inversion may represent occipital subluxation into hyperextension (i.e., ¯θX, antero-superior condyle) with compensatory hyperflexion at the atlanto-axial level (
Fig. 4-13C).
Adjusting Considerations for Developmental Variants Hadley (
4) lists five causes of neurologic compromise in cases of cervical spine anomalies and notes that symptoms often do not appear until the second or third decade of life:
Constriction of the foramen with resultant pressure on nervous structures
Adhesions
Ischemia from interference with blood supply
Interference with the dynamics of the cerebrospinal fluid between the ventricles and subarachnoid spaces causing hydrocephalus
Increased pressure within the cerebellar fossa from basilar impression or invagination.
Forceful adjustments, particularly those employing rotation of the head, should be avoided. This does not mean that patients with spinal anomalies should be categorically denied the potential benefits of chiropractic
care. If the decision is made to apply gentle adjusting procedures, the response of the patient should be carefully monitored. If an adverse reaction occurs, an alternative procedure or no procedure at all should be considered.
The authors suggest that the chiropractor consider the following when selecting adjustment techniques for patients demonstrating nonsegmentation:
Pediatric Spine Fractures Children younger than age 16 account for 7% or less of injuries to the spine (
148,
149). Although pediatric spine injuries are relatively uncommon, their prompt recognition and proper management are essential in chiropractic practice. See
Chapter 23 for further information on the management of adolescent patients with acute spinal fractures and dislocations.
Motor vehicle (including motorcycle) accidents account for more than 50% of the injuries, with team sports, diving injuries, and physical abuse accounting for most of the remainder. The most common area of injury is the cervical spine but can occur anywhere (
150,
151,
152). In cases of spinal trauma, plain AP and lateral radiographs should be taken of the entire cervical, thoracic, and lumbar spine because of the high occurrence of contiguous and non-contiguous injuries (
153,
154,
155). If an abnormality is detected on plain films, CT may be useful in characterizing bony abnormalities (
152,
156). In cases of neurologic involvement, MRI is the technique of choice (
157,
158,
159).
Denis et al. (
160) reported that 50% of deaths due to pediatric spine injuries were associated with injuries to the occipito-atlantal complex. According to Henrys et al. (
149), upper cervical injuries are more common in children and adolescents. The Powers ratio (
161) can be used to assess such injuries on plain radiographs. This ratio is between the distances of the basion to the posterior arch of the atlas and the distance from the anterior arch of the atlas to the opisthion. Powers ratio should be equal to or less than 1 in the normal cervical spine.
Upper Cervical Fractures Jefferson fractures are rare in children. Two cases, children aged 7 and 12 years, have been reported in the literature (
153). The most frequently encountered fracture of the axis is the dens fracture (
162,
163), although five cases of bilateral pedicle (hangman) fractures in children were reported by Pizzutillo et al. (
164) (
Fig. 4-14). Jefferson fractures are usually not neurologically unstable (
165). Many have been treated with entirely conservative methods.
Lower Cervical Fractures Lower cervical spine fractures are seen more frequently among adolescents than young children (
153). Most are associated with flexioncompression injuries in collision sports (
166). Motor vehicle accidents are another important cause of these injuries (see
Chapters 20 and
23).
Thoraco-lumbar Fractures A variety of fractures may present in the pediatric thoracic and lumbar spine. The most common vertebral fracture seen in children younger than 10 years of age is the compression fracture (
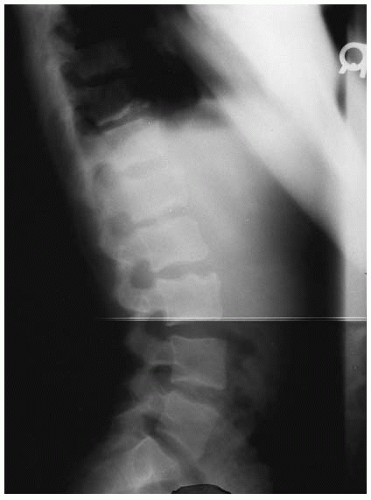
152). The cause is a compressive flexion force. Schmorl’s nodes occur from excessive compression loading (
Fig. 4-15).
Seatbelt injuries can result in a compressive distractive force leading to the Chance fracture (see
Chapter 23). Fracture through the bone as well as soft tissue damage may result, although the ligaments are usually spared (
167).
Spine Injury from Physical Abuse Gunshot injuries (
Fig. 4-16) and child abuse (see
Chapter 16) are other causes of spine fractures (
160). Avulsion fractures of the spinous processes in the cervical spine and compression fractures in the thoracic and lumbar region may occur as a consequence of violent shaking (
168,
169).
Radkowski (
170) has presented seven specific points that the astute clinician should consider regarding suspected child abuse and the interpretation of plain film radiographs:
The radiographic manifestations of the abused or battered child combined with the clinical findings are usually so specific that there is little doubt regarding the appropriate diagnosis.
Most of the conditions considered in the differential diagnosis may be readily identified by a careful interpretation of the clinical history, physical, and laboratory data.
Children with pre-existing disease may also be abused and/or neglected.
Innocent trauma to bone may cause lesions that simulate battering.
Although the radiographic findings may be classical for abuse-related trauma, careful attention should be given to the overall bone mineralization and architecture to rule out predisposing disease.
A conclusion should be drawn from adequate studies. An effort should be made to resolve apparent discrepancies in radiologic findings by different imaging modalities.
Thorough knowledge of the medical, social, and dietary history of the child is essential in a complete evaluation of someone suspected of being abused (
170).
Pediatric Spine Neoplasms Spine tumors in children are relatively uncommon when compared with adults. In Western populations, children younger than age 15 account for only 1 in 200 of all cancers (
171). Because patients with signs of neurologic impairment that may or may not be caused by a mechanical lesion may be brought to the attention of chiropractors, it is important to carefully differentially diagnose a mechanical lesion from a malignant cord tumor. Cancer is more common in younger children. Half the cumulative risk occurs within the first 6 years of life (
171). About one-third of all childhood cancers are leukemias and of these, 80% are acute lymphoblastic leukemia. Between one-quarter and one-fifth of childhood cancers are brain or spinal cord tumors. Of these, one-third are astrocytomas (
171).
Although it has been estimated that 80% of adults will seek professional care at some time for back pain, only 2% of children and adolescents presenting at an orthopedic clinic reported back pain (
172). Others (
173) have reported that the most frequent reason for
a visit to a chiropractor by a child was for respiratory and ear-nose-throat conditions (e.g., otitis media). It is unknown how often patients with neoplasm first present to chiropractors. Spine tumors in children may be primary benign tumors, primary malignant tumors, or metastatic tumors.
Primary Benign Tumors
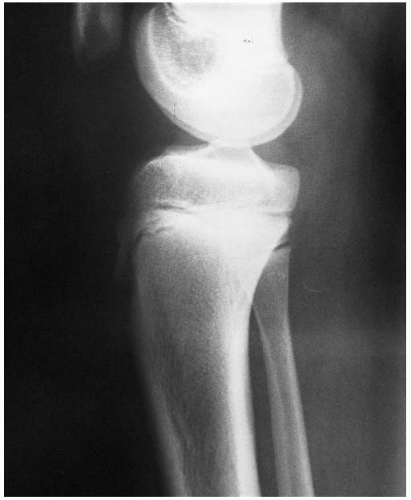
Osteochondroma This tumor is simply an exostosis. It is the most common benign tumor of bone, although only 2% occur in the spine. Seventy-five percent of osteochondromas occur in patients younger than age 20, and men are more frequently affected than women (
174). Spinal osteochondromas rarely cause symptoms (
175). Osteochondromas arise from metaphyseal sites in other bones, with 50% being found in the shoulder and knee. Radiographic findings in extraspinal lesions include a pedunculated mass presenting with a “coat hanger” or “cauliflower” appearance. This finding is characteristic in the knee, hip, and ankle.
Osteoid Osteoma About 1% of spine tumors are osteoid osteomas; these are seen more frequently in men than women and usually appears between the ages of 10 and 25 years. The posterior elements are involved more frequently than the vertebral body. The lumbar spine is more frequently affected than the cervical or thoracic region. Common extraspinal sites include the femur and tibia. Radiologically, osteoid osteoma presents with a lucent nidus surrounded by reactive sclerosis (
Fig. 4-17). Localized pain, worse at night and relieved by aspirin, is characteristic of the disease (
176). Osteoid osteoma is one of the most frequent causes of a painful scoliosis (
177).
Osteoblastoma Approximately 40% of these lesions occur in the spine (
178). Most patients are younger than 30 years of age, and the posterior elements are involved more frequently than the vertebral bodies. Radiologically, an expansive lesion with a thin, clearly defined rim is characteristic (
179). Like osteoid osteoma, pain is usually the presenting symptom. Unlike osteoid osteoma, however, the pain is not worse at night (
180).
Aneurysmal Bone Cyst Although these tumors account for only 1% of primary bone tumors, 11% to 22% occur in the spine. The lesion is usually painful. Neurologic deficit may result from the expansile nature of the tumor (
181,
182) (
Fig. 4-18). Most aneurysmal bone cysts are found in the 5- to 20-year-old age group, and females account for about 60% of cases (
183). Extraspinal sites most commonly affected are the femur and tibia. A “blown out” appearance is characteristic. According to Yochum and Rowe (
1), the aneurysmal bone cyst is the only benign bone tumor known to cross the epiphyseal plate.
Eosinophilic Granuloma This lesion occurs in the second or third decade of life and may not be a true neoplasm. The clinical presentation is often that of an adolescent with back pain. Vertebra plana often occurs, but neurologic deficit is rare. In the absence of neurologic deficit, the condition is self limiting, and reconstitution of height is the rule. This condition was previously reported as Calve’s disease, incorrectly believed to be a form of juvenile ischemic necrosis (
1,
184).
Simple Unicameral Bone Cyst Simple bone cysts are very rare in the spine. Two cases have been reported
in the literature (
185,
186). Most unicameral bone cysts occur in the humerus or femur. These cysts are most prevalent in the 2- to 20-year-old age group, and men are affected more frequently than women. These lesions are characterized radiologically by a geographic lucency. The lesion is asymptomatic unless a pathological fracture occurs, which is common. A “fallen fragment” of cortex freely floating within the cyst is considered pathognomonic, but does not occur in all cases (
187).
Primary and Metastatic Tumors
Astrocytoma Astrocytomas were formerly graded on a scale of 1 through 4, with a grade 1 being benign and a grade 4 denoting malignancy. This system has been supplanted by the terms astrocytoma, anaplastic astrocytoma, and glioblastoma.
Shafrir and Kaufman (
188) presented a case report of a 4-month-old boy who had torticollis since birth. The chiropractor did not take radiographs of the patient. Roentgenograms obtained after presentation as a tetraplegic after a chiropractic adjustment demonstrated widening of the pedicle widths, indicative of a spaceoccupying lesion. An infant presenting with a persistent congenital torticollis should undergo radiographic examination for a potential skeletal anomaly (i.e., Klippel-Feil) or a widened interpedicular distance suggestive of spinal cord tumor.
Multiple Myeloma The most common primary malignant tumor in bone, multiple myeloma, usually occurs in patients older than age 50, but rarely is seen in young patients. Multiple lytic lesions and altered serum proteins are characteristic (
172). The vertebrae, ribs, pelvis, and skull are the sites most frequently affected.
Ewing’s Sarcoma This tumor rarely involves the spine, but when it does, localized pain is usually present. The 5- to 20-year-old age group is most often affected. Metastasis can occur. This is an aggressive and potentially fatal tumor (
1,
172). Long bones frequently affected include the femur, tibia, and pelvis. An “onion skin” periosteal reaction in long bones is classic, accompanied by underlying intramedullary destruction (
187).
Malignant Lymphoma Osseous lesions are seen in about 15% of persons with lymphoma. An “ivory vertebra” appearance in a patient with Hodgkin’s disease is characteristic (
187). This condition may be seen in young adults. Metastasis can occur. Lymphoma is a potentially fatal tumor (
189).
Osteosarcoma Primary involvement of the spine is rare, and spinal osteosarcoma is usually caused by metastasis. Less than 2% originate in the spine. The condition is most commonly seen during the second decade of life. Spinal involvement may be difficult to treat, and the condition is potentially fatal (
190,
191). Osteosarcoma typically affects the 10- to 25-year-old age group and is more common in men. Most cases involve the knee, particularly the distal femur. A “sunray” periosteal reaction with Codman’s triangles is often present. Osseous lesions may be sclerotic, lytic, or mixed (
1,
187).
Chondrosarcoma, fibrosarcoma, and chordoma rarely occur in children or adolescents. Metastasis to the spine in children is most frequently from neuroblastoma and leukemia (
172). Neuroblastomas are tumors of infancy and childhood. The peak incidence is at 2 to 3 years, and neuroblastomas are uncommon after age 7 to 8 years. They arise in sympathetic nervous tissue, most frequently in the abdomen, and an adrenal gland is often involved. The presenting finding is usually an abdominal mass (
192). When metastasis to the spine occurs, destruction of a pedicle may be the earliest radiographic sign. Larger lesions may be lytic, mixed, or sclerotic (
172).
Pediatric Spine Infections Infections in the pediatric and adolescent spine are uncommon in the United States. When infections do occur, the route is usually hematogenous. There are four main categories of pediatric spinal infections (
193,
194).
Discitis This condition usually follows a benign course. Low-grade fever, irritability, back rigidity, muscle spasm, and tenderness may present clinically. Treatment consists primarily of immobilization and rest. Antibiotics are sometimes used, although this treatment is controversial (
195). Radiographically the condition demonstrates collapse of the affected disc, narrowing of the disc space, and marginal destruction with sclerosis of the end plates (
Fig. 4-19). Usually the condition is localized to one site (
192). CT scans may be helpful in the differential diagnosis of discitis, especially in early and atypical clinical presentations or in the case of a nonspecific plain film examination (
196).
Non-tuberculosis Vertebral Osteomyelitis
This rare condition is far more serious than disc space infection. Toxemia may be evident. High fever can occur, and the child will appear very ill. Back pain may be present. Staphylococcus aureus is the most common bacteria isolated (
194). The radiographic appearance of osteomyelitis includes osteolysis with severe deformity—not the isolated endplate involvement that characterizes discitis (
197). In the patient with osteomyelitis, the radiographic examination can yield a range of findings, including a normal radiograph or subtle soft-tissue
swelling to frank bone changes (
198). Radionuclide bone scans may be helpful in the differential diagnosis of the child that presents with bone pain, joint tenderness, soft-tissue swelling and erythema, fever, and bacteremia (
198).
Tuberculosis of the Pediatric Spine The age of onset of this condition is usually between 2 and 5 years of age. The most common site is the thoracic and lumbar vertebral bodies. A reversal of the height:width ratio of the vertebral bodies may occur. The radiographic changes can appear worse than the clinical condition of the patient. Advanced bony destruction may be evident. An “ivory vertebra” may be seen, as well as an associated abscess. The condition can lead to neurologic involvement and skeletal deformity. The disease is associated with poor sanitation and housing conditions. Most pediatric cases in the United States occur among immigrant children (
194).
Spinal Epidural Abscess These are among the most serious infections of the spine and may lead to paraplegia and death. The patients often present with pain, high fevers, and appear very ill. Unlike osteomyelitis, however, plain film radiographs often appear normal. MRI is the technique of choice in such cases (
199,
200) (
Fig. 4-20).
Juvenile Rheumatoid Arthritis Juvenile rheumatoid arthritis is an important chronic disease affecting the joints of children. It is important to remember that articular disease is only one manifestation of rheumatoid disease. When the arthritis is associated with splenomegaly, lymphadenopathy, and pericarditis, the condition is termed Still’s disease. The disease usually begins at 3 to 5 years of age with pain, swelling, and stiffness in the knee. The joints of the hands, hips, and cervical spine are likely to become involved. Radiographic signs of peripheral involvement include soft tissue swelling, osteoporosis, periostitis, marginal erosion, and narrowing of joint space (
192). Cervical spine involvement is characterized by an increase in the atlanto-dental interval, odontoid erosion, subluxation, apophyseal joint erosions, disc narrowing, and generalized osteopenia (
1).
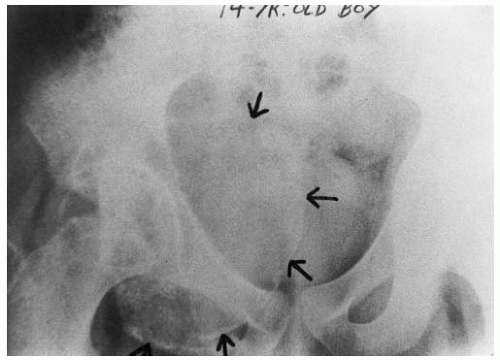
Ankylosing Spondylitis Ankylosing spondylitis is a condition that begins in late adolescence or early adulthood. Most cases affect men. Clinically, low back pain is the usual presenting symptom. As the condition progresses, stiffness will also develop as a byproduct of ligamentous ossification. Decreased chest excursion may also occur. Radiologically, the first evidence of ankylosing spondylitis is irregularity in the sacro-iliac joints. Erosion followed by bony ridging is characteristic. In the vertebrae, ossification of the spinal ligaments leads to a “bamboo spine” appearance. Earlier signs include “squaring” of the vertebral bodies, erosions of the corners of the vertebral bodies, and reactive sclerosis in response to inflammation. The human leukocyte antigen B27 is almost universally present, although most patients do not have the rheumatoid factor. In addition to the skeleton, cardiopulmonary, ocular, gastrointestinal, and genitourinary manifestations of ankylosing spondylitis have been reported (
1,
187).
Scleroderma Progressive systemic sclerosis, known as scleroderma, is a connective tissue disorder of unknown etiology. Manifestations of the disease can differ among adults and children, especially in the hands. In a radiologic survey of 12 children with this disease by Shanks et al. (
201), no osteolysis or erosions of the hands was evident, although two children did have flexion deformities. Soft tissue atrophy was seen in three-fourths of the patients’ hand radiographs. Tuft resorption was detected in two-thirds of patients and generalized osteopenia was present in all but two patients.
Scoliosis Scoliosis may be caused by muscular imbalance, structural asymmetry, decompensation of adaptational curves, or be idiopathic in nature (
202). Adolescent idiopathic scoliosis is, in part, a hereditary condition (
203). Recently, investigators have reported abnormal proprioceptive function believed to be caused by a posterior column abnormality. Abnormal vibratory sensation in both upper and lower extremities suggests that the lesion is located in the cervical spinal cord (
204).
Scheuermann’s Disease This condition is sometimes known as juvenile kyphosis or Scheuermann’s kyphosis. The etiology is controversial, but is believed to be an abnormality of the cartilaginous endplate. This results in anterior Schmorl’s node formation (
205,
206) (
Fig. 4-21). The 13 to 17-year-old age group is most frequently affected (
207). Bradford (
208) has proposed that the following criteria are most accurate for determining the presence of Scheuermann’s kyphosis:
Hyperkyphosis >40 degrees
Wedging of 5 degrees or more at one or more vertebrae
Apparent loss of disc space height
Endplate irregularities
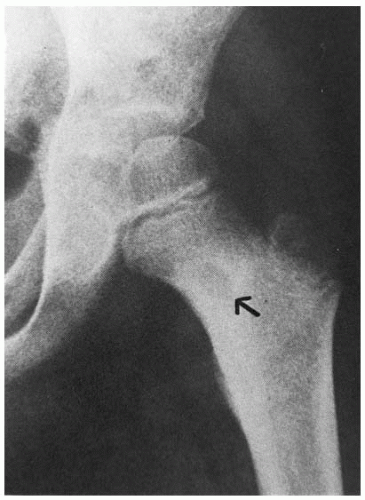
Legg-Calve-Perthes Disease The condition was originally described by Legg of Boston, Calve of France, and Perthes of Germany in 1910 (
209,
210,
211). Legg-Calve-Perthes disease is an avascular necrosis affecting the capital femoral epiphysis. The condition is usually unilateral. Weight bearing may lead to deformity, and crutches can reduce weight bearing. The disease is self-limiting. Boys are affected more than girls; Legg-Calve-Perthes disease affects one in 820 boys and one in 4,500 girls (
212). The condition is most common in children between 4 and 7 years of age, but the disease occasionally affects older children and adolescents (
213). Early appearance of the disease is associated with a more favorable prognosis than late onset (
214). The condition is rare in blacks and persons of Chinese descent (
215,
216). A family history is present in about 6% of cases (
217). The disease is associated with urban areas and occurs with greater frequency in families of lower socioeconomic status (
216). Bilateral involvement is present in about 10% of cases and should suggest the possibility of hypothyroidism (
218). The etiology is controversial, although the pathology is osteonecrosis (
219,
220). Necrosis is observed in both the marrow and trabeculae. Healing is associated with revascularization of the necrotic portion of the femoral head (
218). The time required for the entire process varies from 2 to 8 years. Four stages describe the progress and resolution of the disease:
Avascular stage
Revascularization
Repair
Toby et al. (
221) have proposed that MRI be used to further evaluate avascular necrosis of the hip. They point out that areas of necrosis and the articular cartilage are easily identified with MRI. MRI also provides information concerning the shape of the femoral heads in Legg-Calve-Perthes disease that is of comparable quality to that obtained from arthrography, although the former is not an invasive test and general anesthesia is not needed. MRI is also superior to a pin-holed collimated bone scan in the precise identification of
avascular areas and the percentage of femoral head involvement. Revascularization in Legg-Calve-Perthes disease is easily detected with MRI, which may provide important information for the potential discontinuation of treatment (e.g., bracing, crutches) (
221).
Other Epiphyseal Disorders Numerous eponymic disorders of developing epiphyseal centers have been described. Some are believed to be caused by trauma or overuse (e.g., Sever’s disease of the os calcis and Osgood-Schlatter disease of the tibial tubercle). Others are thought to be caused by osteonecrosis.
Sever’s Disease Heel pain with an associated irregularity in the calcaneal apophysis is the classical presentation of Sever’s disease. Yochum and Rowe (
1), however, consider a fragmented, sclerotic, irregular calcaneal apophysis to be a normal finding and encourage eliminating the concept of Sever’s disease.
Osgood-Schlatter Disease This condition is now considered to be an avulsion injury rather than a form of aseptic necrosis. It most frequently occurs in children 10 to 15 years of age and affects more boys than girls. The clinical presentation includes local pain, tenderness, and swelling over the tibial tubercle. Radiographically, there is avulsion and fragmentation of the tibial tubercle with soft tissue swelling (
192) (
Fig. 4-22).
Spondylolysis and Spondylolisthesis The incidence of spondylolysis is 4% to 6% (
198). Most cases occur during the adolescent growth spurt. Spondylolysis is a stress fracture in most instances, although sudden macrotrauma in hyperextension can produce an acute lesion (
222) (see
Chapter 23). Anterior displacement of the involved vertebral body may lead to pathomechanical changes, although the association of the condition with back pain varies (
Fig. 4-23).
Rickets Rickets (meaning “to twist”) is a disease rarely seen today. It is caused by a deficiency of vitamin D or an abnormality of vitamin D metabolism. Radiologically, changes are best seen in the distal radius and around the metaphyseal end of the involved bone and fraying of the metaphyseal margins (
187) (
Fig. 4-24A,B). In addition to disturbances in growth, other symptoms can include, tetany, listlessness, and generalized muscular weakness. Fractures occur frequently (
223).
Scurvy Rickets Scurvy is caused by a deficiency of vitamin C and is found almost exclusively in infants fed on pasteurized or boiled milk preparations (
2). Radiologically, there is widening of the metaphyses with accentuation of the adjacent metaphyseal plate, which has a lucency underlying it. The epiphysis may present a “ring sign” lucency under its subchondral margins (
187).
Lead Poisoning Lead poisoning can occur with or without symptoms. Radiographs demonstrate opaque transverse lines in the metaphyses of long bones. These lines may persist into adulthood. Lead poisoning occurs in children who eat old paint containing lead or inhale lead in dust particles, although other sources must also be considered. Transverse lines in newborn infants may be the result of drugs given during pregnancy (
192).
Systematic Approach to Radiographic Interpretation
The use of a systematic approach to radiographic interpretation should assist the doctor in developing good film reading habits that will eventually become second nature. In the following section of this chapter, we first present each individual skeletal radiograph (e.g., lateral cervical, AP full spine) and a protocol to its interpretation. For each view, a general “checklist” for interpretation is presented. After each checklist is a table of common abnormalities that may be evident on the radiograph. These lists are not all-inclusive. Roentgenometric analysis (i.e., spinography) of spinal biomechanics is presented for each radiographic view. Spinography is used to evaluate the global postural and intersegmental static positions of the spinal column and pelvis. In the case of radiographs of the spine taken at the extremes of movement (e.g., lateral bending, flexion), spinographic procedures are presented to assist in the interpretation of vertebral motion. The chiropractor is encouraged to develop specific and thorough examination procedures consistent with the needs of the individual patient and the adjustive techniques employed by the doctor (
224,
225).
Roentgenometrics/Spinography Roentgenometrics involves the measurement of anatomical structures from radiographs. These measurements can be quantitatively based (i.e., mm or degrees) or assessed in a more qualitative manner. For example, an assessment of lateral bending of the lumbar spine may simply compare the relative efficiency of a motion segment to laterally flex to the right side when compared with the left. Chiropractic spinography can be defined as a roentgenological diagnostic procedure that uses postural (weight-bearing) x-rays for the principal purpose of evaluating the spinal column and pelvis for evidence of clinically significant biomechanical irregularities (
19).
Static Assumptions Certain assumptions of normal need to be made when analyzing the static upright posture of the spinal column, not the least of which is the assumption that the spinal column is at its highest efficiency when the individual is standing erect on both feet and that the spine is relatively straight when viewed in the coronal plane. The presence of structural anomalies (e.g., hemivertebra) decreases the validity of certain static assumptions in addressing the supposed optimal spinal position. These anomalies will also have direct impact on “normal” functioning of the motion segment.
For the sagittal plane, an assumption is made that there should be a balanced interplay between the lumbar lordosis, thoracic kyphosis and cervical lordosis (
226).
Some authors (
227) have maintained that the spinal curves that are evident in the sagittal plane can be quantitatively evaluated and that deviation from this model represents abnormal spinal posture. The assumptions made for the spinographic analyses presented here are as follows:
When an individual is x-rayed in the coronal plane while in the standing position with approximately equal weight on both feet, the spine is at its optimum if it does not deviate laterally and is relatively straight (
Fig. 4-25A,B).
When an individual is x-rayed in the sagittal plane, there should be a lordotic configuration of the lumbar lordosis with the apex of the curve at L3. The thoracic kyphosis should have its apex at T6-T7 and the cervical lordosis should have its apex at C4-C5. In addition there should be a relative balance of the magnitude of curve in each spinal region. A vertically drawn gravitational line should demonstrate that each spinal curve’s apex is furthest from the gravitational line (
Fig. 4-26A-C). Harrison et al. have presented a model for the normal cervical lordosis (
227).
Dynamic Assumptions As is the case when analyzing static upright posture, certain basic assumptions need to made when analyzing the movement of the spine at its extremes of bending. As is the case for the static upright posture, vertebral development is assumed to be symmetrical, and there will be minimal osseous malformation because this will have an effect on the function of the spine accordingly.
For movements such as lateral bending, there is an assumption that the quantity of movement both globally and on the intersegmental level will be relatively symmetrical in patients without dysfunction. There is also an assumption that coupled movements of the spine are relatively predictable (
54,
228).
In the analysis of spinal position at the extremes of lateral bending, an assumption is made that the spine is most normal when the quantity of movement at each spinal level is approximately the same as that at adjacent levels and that there are gradual increases and reductions in spinal movement as one moves from one spinal region to another. There should not be abrupt changes in the quantity of movement such that one motion segment exhibits minimal movement while its neighbor demonstrates substantial motion.
Gracovetsky and Farfan (
229) have proposed a model for the mechanism of the lumbar spine during lifting and locomotion.
Nomenclature The International Listing System. The right-handed orthogonal coordinate system (RHOCS) is used in the biomechanics community and in some chiropractic circles for communication of the kinematic aspects of the spinal column (
230,
231). Vertebral position and movement can be accurately and unambiguously described with this listing system for all six degrees of freedom of the motion segment (i.e., translation and rotation along or about the three cardinal axes [
Fig. 4-27]). Since the RHOCS has been proposed as an international standard for defining body parts, it is referred to as the “international system” (
232).
This system should be the primary method of communication for the various configurations and movements of the motion segment and should be adopted by the chiropractic profession (
232). Continuation of multiple, sometimes arbitrary, listing systems leads to confusion in the student and among practitioners, especially when referral of a patient is required. The use of different points of reference when using the various (often conflicting) systems has not been helpful, especially in state licensure standardization or instruction.
Instructors of technique should come to some consensus on this issue of nomenclature. Basic chiropractic technique research such as force parameters and patterns of motion should be communicated to the biomechanics community at large using the RHOCS or international system (
230,
231,
232).
The X axis runs from the center of the motion segment straight left (+X) or right (¯X) (
Fig. 4-28). The Z axis runs from the posterior (¯Z), to the anterior (+Z) through the X axis, whereas the Y axis, which is also referred to as the longitudinal axis, runs in a caudal (¯Y) cephalad (+Y) direction. Rotation clockwise (+θ), or counterclockwise (¯θ), is determined by looking from the negative pole of the axis toward the positive end and noting the direction of rotation. Rotation can also be determined by using the right-hand rule. By pointing the right thumb in the direction of the positive pole of the axis under scrutiny, the fingers will then curl in the direction of positive rotation (+θ). Translation is movement along the axis and can be in a positive or negative direction.
Figure 4-29 demonstrates rotation around the X-axis. Flexion motion equates with +θX and extension is ¯θX. Lateral flexion is described as rotational movement around the Z-axis (
Fig. 4-30).
Figure 4-30 depicts the Y-axis. The reader is reminded that interpretation of rotation around the Y-axis must be done by looking from the negative pole of the axis toward its positive end. Spinous rotation to the right is the same as clockwise rotation around the Y-axis (i.e., +θY). External or lateral movement of the right PSIS is denoted also as +θY (
Fig. 4-31).
By convention, the listing of movement or position of the motion segment is with respect to the vertebra below (
230,
231,
232). This is in contrast to many “upper cervical” listing schemes that list the atlas with respect to the occiput. For these scenarios, the occiput would be listed with respect to the atlas.
A necessary exception in terms of segmental contact and point of reference occurs at the lumbosacral junction. In some instances, in which there is failure of extension motion (S1-L5) and the posterior disc space remains open during this movement, it is often preferred to use a SI tubercle contact to create an extension movement at the motion segment. The term base posterior sacrum (S1 ¯θX) is used to describe this type of dysfunction (
Fig. 4-32). Because the contact point is the sacrum for the adjustment, this segment is listed. The dysfunction exists at the L5-S1 motion segment so the sacrum is listed with respect to L5. The sacral base is moved from a posterior to anterior direction during the adjustment, creating an extension moment at L5-S1. The base posterior sacrum is primarily listed as such because of the posterior to anterior direction of correction. An individual listing of the sacrum can have varying degrees of ±θX and retrolisthesis depending on the architectural characteristics of the articulations. Anomalies such as sagittally oriented facets at L5-S1 may allow larger degrees of posterior translation than in coronally oriented facet planes.