Adolescent Patients with Acute Spinal Fractures and Subluxations
Gregory Plaugher
David J. Rowe
David L. Cichy
Cheryl E. Goble
Richard A. Elbert
Christopher R. Hart
J. Larry Troxell
Peter Thibodeau
Although contemporary chiropractic authors have devoted considerable time in their writings to the discussion of acute traumatic disorders of the spinal column (1,2,3), the subject of chiropractic management of patients with spinal fractures and dislocations has not been presented. This may be a reflection of the relatively specialized nature of the endeavor and/or the lack of scientific substantiation for these treatments in the literature. It is important for the reader of this chapter to keep in mind the seriousness of evaluating and/or treating any patient who has suffered a trauma, especially one capable of causing a fracture or spinal dislocation. It is also the authors’ intent to provide as much detail as possible about this specialized area of chiropractic while also acknowledging the fact that not all clinicians will necessarily participate in this area of practice. It should go without saying that practice procedures for an individual patient cannot be gleaned from a textbook or single writing (e.g., case report), but arise from interactions and consultations with others who are more experienced, with careful attention paid to the nuances of the individual case.
The chiropractic scientific literature consists primarily of individual case reports or multiple case series of both successes and failures in the area of fracture management. The orthopedic, neurosurgical, and medical management literature also consists of both uncontrolled reports and nonrandomized comparisons of different customary (medical or surgical) procedures.
The relatively few case reports about the chiropractic management of spinal fractures or dislocations involve inappropriate diagnosis of the lesion with subsequent manipulation. Manipulation either did not resolve the patient’s complaints or aggravated the condition, necessitating eventual medical or surgical treatment (4,5), or there was directed referral of the patient for surgical intervention (6). Rowe (7) was the first author to report in a thorough manner the successful chiropractic management of acute, subacute, and chronic patients with spinal fractures and dislocations. Many of the case reports presented by Rowe (7) were initially misdiagnosed by other practitioners. Less than appropriate practice occurs in both the medical and chiropractic professions (see the section “Missed Fractures”). During the past decade there have been no new published cases of pediatric trauma producing sprain or fracture.
Rowe (7) has presented the biomechanical factors associated with spinal and pelvic fractures and dislocations, leaving the reader with a preliminary introduction to the topic. This chapter will present more detail on the specific chiropractic management of patients with spinal fractures and dislocations. The case studies also are presented in as much relevant detail as possible for the student and doctor to gain an appreciation for the nuances of this specialized form of chiropractic practice. Future comparison of chiropractic, medical, or surgical methods in combination or as sole treatments among specific patient populations will begin to attempt to sort out the most efficacious treatment.
PATIENT POPULATION
Chiropractic pediatrics encompasses the care of children from birth through adolescence. Adolescence is defined as the beginning of puberty through completed growth and maturity (8). Skeletal growth ceases between the ages of 18 and 25 (9). The case studies presented in this chapter comprise adolescents, and all injuries were a result of severe trauma.
Several of the cases presented in this chapter were a result of automobile injuries (see Chapter 20). There are also two water sports injuries. These two populations of children—automobile passengers and individuals engaged in recreation or sports—constitute the majority of adolescent injuries. Among younger children (e.g., younger than 8 years), falls comprise the majority of precipitating events.
ETIOLOGY
The injuries sustained by the group presented in this chapter represent the major kinds of trauma commonly encountered among adolescents. Injuries during this time can lead to lifetime deformities. Many such injuries may be missed during the initial presentation because the radiographs are interpreted incorrectly, improperly exposed or positioned, or not obtained at all. Because skeletal growth is not complete, deformity at this stage can progress as the bones continue to grow. At times there can also be growth and compensation that tend to mitigate the effects of the injury.
As can be seen from the types of acute spinal disorders presented here, the type of injury is dependent mostly on the mechanism of trauma and the amount of force involved rather than on any spinal biomechanical function substantially different from the adult. Although it is more common in the child, there can be severe neurological injury without fracture or dislocation at any age (10).
The cervical spine attains functions that are similar to the adult after approximately 8 years of age (11). In the case of the adolescent, cervical injuries, including fractures and dislocations, occur predominantly in the mid and lower cervical spine. Among infants and toddlers, the general patterns of injury to the neck seem to favor the upper cervical region, with injuries such as occipital subluxations and dislocations and fractures of the dens and atlantoaxial rotatory fixation being typical examples (11).
McGrory et al. (12) reviewed the records of 143 patients admitted to the Mayo clinic between 1950 and 1991. All patients had sustained injuries to the cervical spine. The injuries included fractures, dislocations or subluxations, and fractures with subluxation or dislocation. There was a clear demarcation of injuries sustained by children in two separate age groups. Children younger than 11 years of age had fewer injuries as a group. This group also had more injuries to the upper cervical spine, and most of the trauma was a result of falls. There was also a higher rate of mortality among children younger than 11 years of age. Children between the ages of 11 and 15 years more often were injured through sports and recreational activities. This group had injuries more often to the lower cervical spine. There was also a higher male to female ratio in this sample, and the pattern of injury was similar to that seen in adults (12). The age- and sex-adjusted incidence of cervical spine fractures and dislocations is 7.41 per 100,000 population per year (12).
CHIROPRACTIC LITERATURE
There is scant literature on the topic of chiropractic management of spinal fractures and dislocations (7,13,14). The literature detailing successful chiropractic management practices is contained in uncontrolled case reports that are fraught with confounding variables, lessening both their interpretability and generalizability.
Guebert and Thompson (6) present a burstcompression fracture of the lumbar spine that was initially diagnosed by a chiropractor but subsequently was referred to an orthopedist who performed Harrington rod surgery. The patient was neurologically intact at the initial presentation.
Clements et al. (15) report on fractures of the thoracolumbar spine in three adults. The cases were managed by either bracing, rest, physical therapy, mobilization, or massage. Clements et al. (15) advise that manipulation should be applied in these types of cases only above and below the site of the fracture. The authors of this chapter suggest an entirely alternate approach. If subluxation findings are present, then the fracture site, at times, will need to be adjusted (see the sections about fracture-subluxation and dislocation-subluxation).
Haldeman and Rubinstein (5) have brought attention to the factors involved in patients who have compression fractures and who are receiving spinal manipulation. The authors noted that, of the 89 cases involving malpractice litigation that were referred to their offices, four cases directly implicated chiropractic adjustments as the cause of the spinal compression fracture. There was no cause-effect relationship demonstrated by Haldeman and Rubinstein in their report for precipitation of a spinal compression fracture after manipulation (16). Iatrogenesis may be more prevalent within the medical profession when long-term use of steroid treatments leads to bone demineralization. The widespread use of steroids runs contrary to the lack of good evidence that these drugs are efficacious for the seemingly endless varieties of disorders for which they are prescribed (16).
Nykoliation et al. (4), reviewed three cases of cervical spine fractures and dislocations that were missed during examinations performed by chiropractors. Cervical manipulation was subsequently performed, without good result.. The patients eventually underwent spinal surgery. Nykoliation et al. (4) advise that manipulation of a patient with this disorder is contraindicated. Though it is true that an improper diagnosis before an
adjustment would contraindicate the procedure, it is the authors’ clinical experience that properly performed specific adjustment procedures applied at segmental levels where there is not reproduction of the mechanism of injury are not contraindicated. However, delaying surgical intervention when the neurological condition (see Chapter 11) of the patient continues to decline while under chiropractic care is not appropriate (7).
adjustment would contraindicate the procedure, it is the authors’ clinical experience that properly performed specific adjustment procedures applied at segmental levels where there is not reproduction of the mechanism of injury are not contraindicated. However, delaying surgical intervention when the neurological condition (see Chapter 11) of the patient continues to decline while under chiropractic care is not appropriate (7).
CHIROPRACTORS IN TRAUMA CENTERS
The authors are aware of several instances in which chiropractors have adjusted patients with severe subluxations and fractures in the hospital. One such patient is that presented in the case study of a burst fracture of T7, presented later. Ideally, there should be more cooperation between chiropractors that specialize in this area of patient management and nursing staff, emergency room physicians, and orthopedists or neurologists involved with the case. The patient can only benefit from such open communication and interdisciplinary case management. For too long, the absence of avenues of communication between doctors has been to the detriment to the patient.
Duke and Spreadbury (17) lament about surgeons and anesthesiologists overcoming their dread of making things worse when attempting closed reductions of lesions with manipulation. They advise performing the manipulation while the patient is under anesthesia. Duke and Spreadbury (17) present a case involving a bilateral facet dislocation of C5 on C6. A spondylolisthesis was present at the involved level. Closed manipulation resulted in good alignment. At 9 days’ follow-up there had been some forward slippage of the motion segment caused by the rupture of the various ligamentous elements. Chiropractors could fill an important role in trauma cases where highly skilled hands are necessary. The authors recommend more cooperation between skilled chiropractors and medical doctors in cases of acute spinal trauma.
MANIPULATION UNDER ANESTHESIA
The subject of spinal manipulation of patients while they are under conscious sedation, not with complicating factors (e.g., fracture), has a limited but growing following of advocates within the chiropractic profession. None of these advocates has described protocols for the pediatric population with or without complicating factors such as fracture. In neurologically stable patients, especially those seen on an outpatient basis, the subject of the role of manipulation under anesthesia deserves some mention here.
It is the authors’ opinion that to properly adjust patients who present with spinal fractures or dislocations it is necessary that the patient be fully conscious and understand the nature of the treatment. The patient’s cooperation during both the assessment and adjustment process is essential. It is necessary that the treating doctor be in full oral communication with the patient. Certain aspects of the adjustive process, such as preload thrust and the use of reflexive contraction of surrounding musculature (discussed later) as an indicator of the point of motion segment tension are impossible to determine properly if the patient is sedated. The chiropractor must always be able to assess the patient’s tolerance to the adjustment through constant communication. Any procedure, such as conscious sedation or general anesthesia, that restricts the ability of the patient to interface with the doctor during the adjustment is not recommended.
CHIROPRACTIC SCOPE AND STANDARDS OF PRACTICE
The scope of chiropractic practice varies from state to state in the United States and in all jurisdictions throughout the world. In some US states the issue of patients being adjusted when fractures are present often is not addressed.
Research on which to base standards of practice is sorely lacking for professionals who treat patients with spinal injuries. Chiropractic benefits cannot be discounted only because of the lack of currently available evidence when scientifically validated alternatives do not exist in many circumstances. The first axiom of the doctor must be to above all do no harm (primum non nocere).
Neither surgical techniques nor conservative medical management with collars, bracing, and/or exercise has been subjected to valid scientific scrutiny. In the absence of evidence to the contrary, any attempt by governing bodies to limit therapies without adequate trial runs counter to the patient’s right to choose.
Informed consent should be obtained from all patients (or a suitable guardian) with a specific explanation of the patient’s current condition and options for management.
Denying a patient access to chiropractic services may lead to increased lifetime spinal distortions, scoliosis, and other disorders linked to the axial locomotor system. Doctors who are unfamiliar with the management of these disorders should consult with others who are more experienced in this field. Complex lesions are better evaluated with advanced imaging.
Surgery is an invasive procedure and the effects usually are irreversible. Because there is evidence
that delaying certain surgical procedures when there is no neurological deterioration does not result in a more unfavorable prognosis, conservative procedures, including chiropractic, can be applied initially if there is an indication for subluxation reduction.
that delaying certain surgical procedures when there is no neurological deterioration does not result in a more unfavorable prognosis, conservative procedures, including chiropractic, can be applied initially if there is an indication for subluxation reduction.
It is unfortunate, but some chiropractic patients likely are treated in the absence of proper identification of a spinal fracture. Neural arch fractures and compression injuries are the most likely fractures that are missed without the proper imaging examination, although missed cervical spine dislocations have been reported (4).
FREQUENCY OF INJURIES IN CHIROPRACTIC PRACTICE
Winterstein (18), in his review of stable acute compression fractures, mostly among older women with signs of osteoporosis, has described a role for chiropractic intervention in these patients. He advises light adjusting/mobilization above and below the fracture site. He also acknowledges that there is some controversy in this area of chiropractic management. In Winterstein’s (18) article, it was reported that up to 9% of patients presenting to a chiropractic clinic may have compression fractures.
There has been no systematic study of the frequency at which patients with spinal fractures and dislocations present for chiropractic evaluation. The greater the trauma (e.g., sports, automobile accidents) encountered by the patients in the practice will determine how frequent these injuries occur. If radiographs are not customarily obtained, both old and sometimes acute injuries can go unnoticed (see the section “Missed Fractures”). Because of misdiagnosis, many of these lesions may remain hidden and are treated both inadvertently and inappropriately.
CHIROPRACTIC EDUCATION
The chiropractic management of spinal fractures and dislocations has received little attention in chiropractic colleges. The authors are aware of only one current postgraduate education program that teaches management procedures in this area (19), although the subject likely has been presented in other venues in the past.
The subject has been taught at chiropractic colleges, but the content usually is dependent on the particular clinical experience of the practitioner teaching the course. Some of this material may be presented in trauma management courses during the student’s final year of chiropractic college, if it is presented at all. Unfortunately, this unevenness in instruction has led to some graduates not having sufficient education to recognize that limited expert consultation is available in some regions of the country, and patients with these conditions deserve to be evaluated and possibly treated by some chiropractors. Practitioner fear may also be present because of generalized confusion regarding scope of practice (if may not be legal in one state but it may be in another) and reimbursement issues, as well as simple ignorance about handling patients with acute trauma. It is advised that individuals who have less experience handling these injuries work closely with at least one other chiropractor who has more experience in the area of interest.
SOCIETY COSTS FOR SPINAL CORD INJURY
Cervical spinal cord injuries are a major cause of death and disability in the United States. Injuries from motor vehicle accidents result in 500 to 650 quadriplegics per year (20). The approximate cost to society for each new cervical spinal cord injury in the United States each year is $400,000 (21). Approximately 10,000 to 11,000 new cases of spinal cord injury (from all causes) occur each year, costing more than $4 billion annually (21,22).
Cotler et al. (23) studied the medical and economic impact of closed cervical spine dislocations. Patients who had initial nonoperative treatment but later needed to undergo surgery had higher overall costs. The nonoperative group’s mean hospital charge per case was $61,351.14. The operative group’s mean charge per case was $42,944.00.
These costs are similar per case to that seen by Roye et al. (24) in a survey of 71 patients with cervical spine fracture who were admitted to a medical center over a 2-year period. Twenty-two patients had neurological injuries. Six patients died in the intensive care unit. The average hospital stay for survivors was 45 days. The average hospital charges were $50,370.00.
PREVENTION OF SPINAL FRACTURES AND DISLOCATIONS
Reath et al. (25) studied the injury prevalence and costs of restrained versus victims who were unrestrained during motor vehicle crashes. Hospitalization after a crash was more frequently required for unrestrained victims. Mandatory seatbelt laws have increased seatbelt usage two- to fourfold in New York. This has resulted in reduced serious and fatal casualties and insurance claims (26).
Because children are often passengers in the rear seat of a vehicle, they are more vulnerable to a Chance
fracture because of the presence of lap seat belts. All seats in a vehicle should have, as a minimum, both lap and shoulder restraining devices. Lap seat belts, in addition to causing another type of spinal injury (i.e., Chance fracture), can also cause severe trauma to the abdominal organs (27) (See Chapter 20).
fracture because of the presence of lap seat belts. All seats in a vehicle should have, as a minimum, both lap and shoulder restraining devices. Lap seat belts, in addition to causing another type of spinal injury (i.e., Chance fracture), can also cause severe trauma to the abdominal organs (27) (See Chapter 20).
When improperly used, any restraint may accentuate the trauma (27,28,29). Wang et al. (27) present a case of a 2-year-old patient who was involved in a car accident while sitting in the front seat on her mother’s lap, facing the mother, with a three-point harness wrapped around both individuals (27). The 2-year-old did not lose consciousness after the accident and there were no visible lesions. Five hours later the patient began projectile vomiting. Computerized tomography of the abdomen disclosed a fractured left pedicle of L2. Part of the jejunum was interposed between the left kidney and the vertebral body of L2. The patient was then transferred to another hospital. A plain film taken of the abdomen disclosed the fracture of the left pedicle. A radiographic series of the upper gastrointestinal tract demonstrated obstruction of the proximal jejunum at the level of the spinal fracture. Resection and end-to-end anastomosis of the perforated segment of jejunum was performed. The patient was discharged from the hospital 20 days later in stable condition.
The greater availability of airbags should also help to prevent some injuries. Safety harnesses over both shoulders (to avoid the roll-out phenomenon), similar to that seen in racing cars, may also be an alternative for automobile manufacturers to consider (7).
Scher (30,31) advises that individuals who are engaged in contact sports, such as rugby, undergo a limited radiographic examination (lateral cervical radiograph) before participation in these activities. Analysis then can be made for congenitally small spinal canals and congenital fusions that may predispose the individual to neurological injury should he or she receive trauma to the cervical spine.
SURGICAL AND NONOPERATIVE METHODS
There is ample evidence that many types of fractures and fracture-dislocations can be managed through non-operative methods (32,33,34), such as bracing and bed rest. It is of concern to some researchers in the arena of fracture care that there is a lack of long-term follow-up studies on patients undergoing fusion surgery. In the case of thoracolumbar fractures and fracture-dislocations, fusion surgery for a fracture at one vertebra will require stabilization instrumentation for five to seven vertebral levels (32). There is literature that suggests that occupational limitation may also result from surgical fusion procedures (32,35).
Hanley and Eskay (36) reviewed the records of 57 patients who suffered fractures and fracture-dislocations of the thoracic spine who presented for medical evaluation over a 10-year period. In no case was there a patient who had a complete neurological deficit that exhibited improvement after surgical stabilization. In a review of tetraplegic cases by Burke and Berryman (37), no patient who had a complete lesion made a satisfactory recovery after closed medical manipulation under anesthesia, traction, or surgical reduction with fusion. In a study of 18 patients who had lower thoracic and lumbar fractures combined with neurological deficits, only nine showed some neurological improvement (38). The patients had an average improvement of 1.125 Frankel’s grade.
Jacobs et al. (39) compared the results of surgical treatment with laminectomy and Harrington rods versus bed rest accompanied with bracing. The laminectomy group fared much worse, as has been confirmed in other studies. No patients that had Frankel grade A function improved. Jacobs et al.’s (39) remark about the presence of an alignment abnormality of the spine that usually was present and caused the neurological injury may be of interest to chiropractors. If such a deformity was not present, then a burst fracture with resultant fracture pieces encroaching upon the spinal canal was assumed.
Traction and closed reduction methods versus surgery were compared in a survey of 68 patients over a 12-year period by Hadley et al. (40). The patients ranged in age from 14 to 63 years. Neither group showed a difference in neurological outcome because of treatment, but when there was a difference in the timing of the reduction, patients undergoing early reduction had better neurological improvement.
Remarkably, research into which method of surgical fusion is necessary continues. This therapeutic approach is based mostly upon enlarging and immobilizing the spinal canal when there is no correlation between neurological recovery and the amount of canal decompression, the initial canal compromise, or the nature of the neurologic lesion (41). Small groups of patients with widely different lesions have been evaluated retrospectively with no randomization and without blinding of assessments or control groups for comparison. From these types of studies, broad statements are made regarding the efficacy and appropriateness of different surgical procedures (42). Only through well-conducted randomized studies (or large prospective cohorts) can differentiation be made between the myriad therapies currently available. Conservative methods, including specific spinal adjustments and bracing, need to be compared in trials, both by themselves and with surgical procedures. Further research will only yield more benefits to patients suffering with these afflictions.
Although hypotheses abound, some surgeons acknowledge that there is no proof for their methods (43). This situation is probably a sign of the dearth of scientifically valid medical research in general (44). Of particular note is a tendency for surgeons studying the issue to focus on outcomes in terms of surgical constructs rather than on patient-oriented functional measures (45).
The authors stress the need for comparison research between chiropractic, medical, and surgical methods. Combined approaches also may prove to be of some benefit, especially when severe neurological injury has occurred. Rehabilitative physical therapists also need to work more closely within an interdisciplinary setting.
The contradictions between the medical and chiropractic approaches to spine trauma are illustrated by a report from Jacobs et al. (39). They stress that, when the patient is moved into a position of extension, direct pressure at the fracture site is always avoided. This advice is contrary to that provided by chiropractors who are familiar with fracture management. The fracture site often is where the majority of high- or low-velocity load(s) or thrust(s) would be applied. This is especially true with flexion trauma when there is a tendency for this injury to cause the motion segment to be translated posterior. In these cases, posterior to anterior-directed forces will help to diminish the tendency toward progressive flexion deformity.
Frankel’s grading (42):
A indicates no sensory or motor function below the level of the injury.
B indicates sensory sparing but no distal motor function.
C indicates that there is lower extremity motor function present, but it is functionally useless.
D indicates that there is functionally useful motor sparing.
E indicates normal sensory and motor function, although hyperreflexia may be present.
Surgery should be questioned as a general panacea because of the lack of good evidence demonstrating its efficacy, but particularly when there is incomplete neurologic injury or no neurologic deficits (32). Gaines and Humphreys (32) advise orthopedists to manage fractures that do not have large neurologic deficits nonoperatively for 2 to 4 months. If canal decompression is needed after this time period, then surgery can be performed (46), preferably at only one level. Similarly, Bohlman et al. (47) report on 45 patients who had spinal surgery an average of 4.5 years after the initial trauma. These patients had continued pain or paralysis that had not responded to conservative measures (not including chiropractic treatment). Surgery in these patients resulted in favorable outcomes (e.g., reduced pain) despite the delay in treatment.
In the case of traumatic spinal cord injury with paraplegia, certain medical methods are necessary to prevent the development of chronic instability, spinal deformity, and complications from other body systems affected by the injury (48). Complications after spinal cord injury include bowel and bladder dysfunction and other organ system trauma, pulmonary emboli, etc.
Donovan and Dwyer (48) state that indications for surgery that are not controversial include correction for an unacceptable deformity or instability. They advise medical management (bracing, rest, observation) and not surgical treatments for most cases of traumatic paraplegia.
Place et al. (49) studied the impact of surgical stabilization on initial rehabilitation and complications among patients with traumatic paraplegia. One hundred thirteen patients’ records were reviewed in the retrospective analysis. Each patient had a minimum of 5 years of follow-up. The review demonstrated that patients who received surgical stabilization versus those who were treated nonoperatively showed a statistically significant increase in complications. Neurologic recovery also was not significantly altered through surgical intervention.
Vlach and Bayer (50) studied laminectomy surgery in patients with fractures of the thoracolumbar spine. The majority of patients undergoing laminectomy had a more severe kyphotic deformity when compared with a conservatively treated group. The kyphotic deformity in the surgical patients was also more frequently progressive.
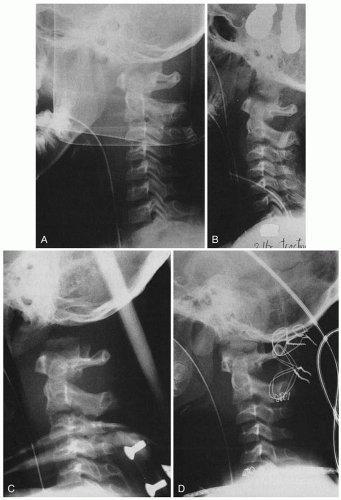
Burke and Berryman (37) advise the use of gentle closed manipulation under anesthesia to reduce dislocations of the cervical spine. In a report of 425 patients with spinal column injury and neurological lesions covering a 7-year period, cervical spine dislocations were discovered in 76 individuals. Closed gentle manipulation to reduce the dislocation combined with mild skeletal traction resulted in a good result in most patients. However, traction applied to certain kinds of patients in whom ligamentous sprain and rupture are present will complicate the injury. Overdistraction can cause further dislocation and/or movement of fracture or disk fragments (Fig. 23-1).
Surgery should be reserved for those patients who exhibit continued or deteriorating neurological instability (37). The advice of Knight et al. (33) is particularly poignant: “Physicians who care for patients with traumatic spinal deformities should resist the temptation to be technicians and not apply metal to every fracture seen.”
BIOMECHANICS OF BONE
Cook et al. (51) studied the association of bone mineral density and pediatric fractures. They concluded that reduced bone density is unlikely to play a significant
role in acute traumatic pediatric fractures. Chan et al. (52) also concluded that pediatric fractures are a result of the particular activities the child engages in rather than any intrinsic bony susceptibility.
role in acute traumatic pediatric fractures. Chan et al. (52) also concluded that pediatric fractures are a result of the particular activities the child engages in rather than any intrinsic bony susceptibility.
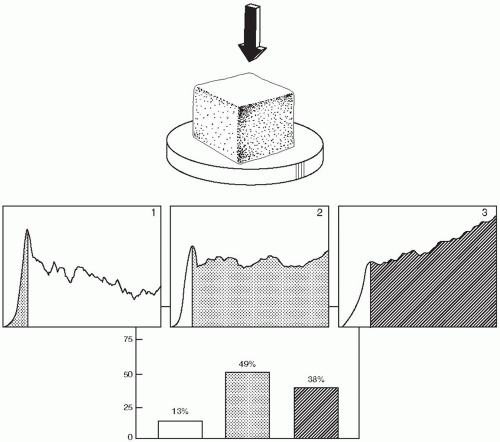
In the case of cancellous bone, as collapse occurs there may or may not be a loss in compressive strength (53). Because the vast majority of compression fractures do not result in a loss of compressive strength, instability should not be assumed from isolated compressive deformity alone. The biomechanical properties of spongy bone are depicted in Figure 23-2.
MAJOR INJURING VECTOR
Throughout this chapter the authors will refer to the major injuring vector (MIV) of each fracture or dislocation case. This terminology reflects the primary force causing the presenting injury. It is helpful to understand the biomechanics of injury so that the treatment procedures (e.g., the adjustment or advice about preferred patient posture) do not reproduce the mechanisms of injury. Often the adjustive intervention should be directed in a line of drive precisely
opposite that of the MIV or opposite the “net effect” of the MIV.
opposite that of the MIV or opposite the “net effect” of the MIV.
SPINAL STABILITY
White and Panjabi (53) define spinal stability as that situation in which a spine placed under normal physiological load is able to resist further positional deformation, neurological damage, and irritation. It is important for the chiropractor to understand the biomechanics of stable and unstable injuries. Each clinical scenario will mandate different approaches to treatment, affect the prognosis of the patient, and will help delineate those cases that may require more aggressive stabilization procedures (e.g., bracing and surgery).
Three-Column Model of Spinal Stability
Denis (54,55) has put forth the three-column concept of spinal stability. He divides the spine into three columns: anterior, posterior, and middle. Through a review of biomechanical studies, Denis determined that instability would not occur if only posterior ligamentous structures were damaged. He found that instability occurred only when there was disruption of the middle column combined with posterior column damage and was the first to recognize the independent importance of the middle column. Denis (55) suggests that spinal instability can only occur when there is damage to two of the three columns, one of which has to be the middle column. Dislocations usually result in disruption of all three columns.
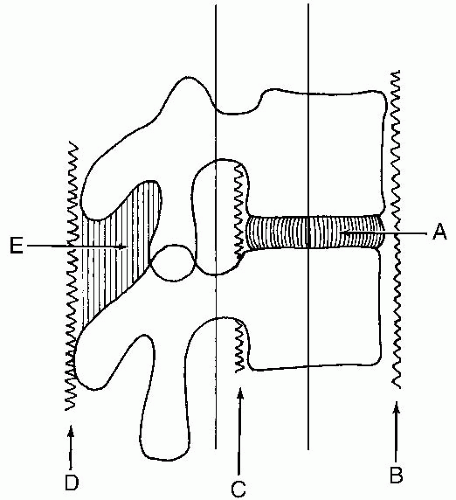
Ferguson and Allen (56) have concurred with Denis on the inadequacy of two-column model descriptions of spinal injury. However, they prefer the term elements instead of columns because the tissues involved do not resemble columns in terms of their anatomy and do not behave as columns in the biomechanical sense (57). Ferguson and Allen’s (56) description of the three elements or columns differs slightly from the Denis model in that the anterior column consists of the anterior longitudinal ligament (ALL), the anterior two-thirds of the vertebral body, and the anterior two-thirds of the intervertebral disc. The middle element consists of the posterior one-third of the vertebral body and intervertebral disk as well as the posterior longitudinal ligament. The posterior element comprises the posterior bony complex (pedicles, lamia, articular processes, and spinous process) and the posterior ligamentous complex (57). The slight difference in this description from the Denis model is that the latter divided the anterior column from the middle at the midpoint of the intervertebral disc. The three element model is depicted in Figure 23-3 (57).
James et al. (58) further refine the Denis model by presenting a unique situation that is a clear example of a two-column injury that does not involve the middle column but does produce instability. The example is a burst fracture that compresses the anterior column and causes distraction injury to the posterior column.
In this chapter, the authors will classify fractures or dislocations as unstable if any two of the three columns or elements are damaged to the degree that they could potentially lead to further mechanical deformity or to increased neurological damage or irritation when placed under normal physiological loading (7).
The Fourth Column
The rib cage is an integral biomechanical component of the spinal column. There are several important mechanical functions of the rib cage, including (53,59):
To stiffen and strengthen the spine. Resistance to displacement is provided by two mechanisms:
The costovertebral joint provides additional ligamentous structures and attachments that contribute
to spinal stiffness and strength. Mobility is also reduced.
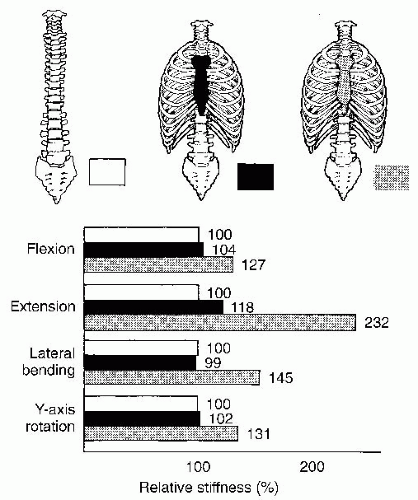
An increased moment of inertia of the thoracic spine. Moment of inertia is a measure of the distribution of a material about its centroid. This distribution determines the strength during bending and torsion. The addition of the rib cage to the thoracic spine effectively increases its cross-sectional area and mass. The increased moment of inertia stiffens the spine when it is subjected to lateral bending and axial torsion. The added stiffness of the spine provided by the rib cage has been well described by Andriacchi et al. (59,60) (Fig. 23-4). It is evident that the results of sternum removal have as devastating an effect as removal of the entire rib cage.
To add energy-absorbing capacity to the spine structure during trauma.
To serve as a protective barrier against lateral or anterior impacts.
For the thoracic spine, fractures in this area can also involve the sternal-rib complex. A proposed fourth column to the Denis three-column spinal model has been made by Berg (61). Two cases of combined sternal and spine fractures are presented: one of which was managed conservatively and one surgically. Berg (61) notes that overriding, displaced sternal fracture is a marker for a severe flexion-distraction thoracic spine injury with a propensity for instability and further deformity.
ETIOLOGY OF FRACTURES, DISLOCATIONS AND SUBLUXATION
Birth Injuries and Neonatal Deaths
The spinal cord can undergo tremendous traction forces during acceleration-deceleration and distraction types of injuries. This is because the cord can only deform approximately 10% of its original length (62). Flexible behavior transforms to stiff resistance when an attempt is made to deform the cord further (62). The spinal column, in contrast, can stretch much more because of the elasticity of the spinal ligaments and discs. As such, the mechanical properties of the joints may be preserved (few signs of subluxation and no signs of fracture or dislocation) with pronounced trauma to the spinal cord and/or nerve roots.
Towbin (63) performed autopsies of infants during the neonatal period. They were victims of crib death, now called sudden infant death syndrome (SIDS). A total of eight infants were autopsied, and in seven were there spinal epidural hematomas (63). The brain stem resides in the cervical cranial junction, and disruption in this area can have a major impact on the breathing centers. Excessive torsion of the upper cervical spine also may cause compression or stretch to spinal cord in the upper cervical region. It is fortunate that now US pediatricians are recommending that infants be placed on their back to sleep. Other countries and chiropractors for many years have recommended this practice. Foreign countries correlate reduced incidence of SIDS with this practice. It is acknowledged that there are also other factors involved with SIDS, such as secondhand smoke. The supine position avoids the increased rotation of the upper neck, which is necessary for proper respiration while in the prone position.
There is good evidence that some birthing methods involve excessive rotation and lateral flexion of the head and neck. The use of forceps and the difficulties encountered with breech deliveries can lead to spinal column or cord injury (64,65). Severe hyperextension of the cervical spine during childbirth can also cause cord injury or death (66).
Shulman et al. (67) has reported the rare complication of transection of the spinal cord during cephalic
delivery. The authors note that mild injury seems to be very frequent. An injury less than cord transection or dislocation may have sufficient force to cause spinal subluxation.
delivery. The authors note that mild injury seems to be very frequent. An injury less than cord transection or dislocation may have sufficient force to cause spinal subluxation.
A cross-species presentation of the possible trauma that can be involved in some birthing practices has been presented by Agerholm et al. (68). They confined their analysis to the incidence of vertebral fractures among newborn calves. A major problem in the cattle industry is the high frequency of stillborn calves and calves dying during the neonatal period. In a study of 100 cases involving stillbirth, death during the neonatal period, or a locomotor disturbance, it was discovered that approximately 7% had sustained vertebral fractures. Anatomical, radiographic, and microbiological techniques were used to analyze the calves. Of interest was the determination that traction forces applied manually during delivery seemed to be a contributing factor to the injuries. Most fractures were epiphyseal separations in nature and were confined to the thoracolumbar junction.
Motor Vehicle Accidents
Motor vehicle accidents are a cause of many of the spinal cord injuries among adolescents and are the precipitating etiology in the majority of the case studies presented in this chapter (see Chapter 20). As in adults, many of these injuries are preventable with the use of proper safety belts and other devices (e.g., air bags). Unfortunately, the unrestrained head and cervical spine may encounter high acceleration/deceleration forces despite the proper use of lap and shoulder restraint belts.
Recreational and Sports Injuries
Reid and Saboe (69) reviewed 1,447 spine fractures over a 7-year period. Two hundred and two (n = 145) were related to sports or recreation. Of these, nearly half (42%) were associated with paralysis. The high incidence of catastrophic injury from recreational and sports injuries is second only to motor vehicle accidents. Approximately 25% of these injuries were caused by the following activities: snowmobiling (10%), snow skiing (5%), tobogganing (5%), and ice hockey (3%).
Physical Abuse
Spine and spinal cord trauma may be present among battered children (70) (see Chapter 16). Violent shaking can produce a cervical lesion much like that seen in a whiplash type of injury. Uncomplicated vertebral fractures can also be asymptomatic (70), leading to avoidance of x-raying the spine.
Ahmann et al. (71) present two cases of spinal cord infarction caused by physical trauma. One patient, a 4-year-old girl, fell when she was pushed out of a swing by another child. The other patient, a 22-month-old boy, was cuffed (a blow with the palm of the hand) at the jaw and face and fell to the floor. The first child died 48 days after the trauma and the other died 6 months later after respiratory arrest. The pattern of infarction was thought to be related to spasm of the distal branches of the central sulcal arteries in a terminal arterial bed (71).
The number of new cases of nonaccidental head injury does not seem to be reducing despite public information campaigns (69). Child abuse does not occur within any one racial, religious, or political group, nor is it confined to the socially disadvantaged. Physical abuse remains a major concern as a preventable cause of death and disability in childhood (72). It is important for clinicians to be alert to the signs that may indicate physical abuse and/or central nervous system injury. The cardinal findings include (73) (see Chapter 16):
An uncertain history or one that seems to be at odds with the physical findings
New onset of seizures in association with retinal hemorrhages (74)
Intradural surface hemorrhages on computed tomography (CT) scan or magnetic resonance imaging (MRI)
Infants showing the above signs may have suffered a nonaccidental injury.
FRACTURE SUBLUXATION
The major types of injuries encountered by the spine include fractures, dislocations, or subluxations (75), and fractures with subluxation or dislocation (12). Fracture at one spinal level combined with injury (e.g., subluxation) at neighboring or distant motion segments can lead to an overall complex biomechanical disorder.
A fracture-subluxation is present when signs of subluxation (75) (see Chapter 3) are also present at the fracture site (i.e., the involved motion segment). The presence of a spinal fracture alone does not necessarily indicate that a subluxation is present at the involved level. A systematic examination of the area will bring forth information necessary to make the proper determination.
In instances of severe trauma or when the index of suspicion for a spinal fracture or dislocation is very high, the practitioner must always keep in mind that a complete subluxation examination (e.g., motion palpation) before the radiologic examination may possibly not be performed.
Static Palpation
Probably one of the more prevalent findings that should be weighed heavily with the multiparameter examination is the presence of a soft edematous area over the spinous process. Palpation with the pads of the fingertips should be used to determine the presence of edema.
The examination for tenderness should be performed by palpating with the tip of the finger or thumb slightly underneath the involved spinous process. Repetitive comparisons of tenderness of spinal levels above, at, and below the fracture site should be performed. The patient should be in a slightly flexed posture to aid the examination. The presence of tenderness should be weighed heavily in the multiparameter examination for signs of subluxation.
Skin Temperature Instrumentation
Skin temperature instrumentation (76,77) may or may not demonstrate positive findings. In cases of acute trauma the presence of generalized skin inflammation caused by marked trauma in the area may not provide the examiner with specific readings at one spinal level, as is commonly found in patients who have less severe injuries. The absence of instrumentation findings does not necessarily rule out the presence of subluxation at the involved level.
Motion Palpation
Patient-assisted motion palpation of the fracture site will generally provide little information beyond assessing the patient’s functional capabilities before receiving a specific adjustment in a slightly stressed position. However, because of the acute nature of the lesion and the presence of prominent inflammation and pain, the patient generally cannot tolerate the adjustment in anything more than predominantly neutral spinal postural positions. For this reason, motion palpation is of little use in providing clinically useful information in these cases. That moderate spinal movements may either reproduce the mechanism of injury or otherwise aggravate the site of the fracture or dislocation illustrates why this procedure should not be performed before a thorough radiological examination.
Plain Film Radiography
Plain film radiographic examination is essential during the evaluation of trauma to the pediatric patient (see Chapter 4




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree