● COMMON ARTERIAL TRUNK
Definition, Spectrum of Disease, and Incidence
Common arterial trunk (CAT), also referred to as persistent truncus arteriosus, truncus arteriosus communis, and aorticopulmonary trunk, is characterized by a single arterial trunk that arises from the base of the heart and gives origin to the systemic, coronary, and pulmonary circulations (Fig. 26.1). A large ventricular septal defect (VSD) is almost always present in this anomaly, resulting from the nearly absence of the infundibular septum (1). CAT results from failure of the truncus swellings, which normally divide the truncus arteriosus into the aorta and pulmonary arteries during embryogenesis, to fuse, resulting in a persistent common trunk (2) (see Chapter 3). The spectrum of the disease is wide and is mainly related to the anatomic origin of the right and left pulmonary arteries, which may arise from a pulmonary trunk (Fig. 26.1A,B) or as direct branches from the CAT or the descending aorta. CAT is classified into four types by Collett and Edwards, based on the anatomic origin of the pulmonary arteries (3). In type 1, a short pulmonary trunk arises from the CAT and divides into right and left pulmonary arteries (Fig. 26.1A). In types 2 and 3, both pulmonary arteries arise separately, as individual branches, from the CAT and they are either close anatomically (type 2) or at some distance from one another (type 3). In type 4, which is now reclassified as pulmonary atresia with VSD (see Chapter 25) rather than CAT, the pulmonary arteries arise from the aortic arch or the descending aorta. Another classification, type A1 through A4, was proposed by Van Praagh and Van Praagh (4). In this classification, type A1 is similar to type 1 of Collett and Edwards’s classification, type A2 combines types 2 and 3, type A3 describes a single pulmonary artery origin from the CAT with either a ductus or collateral circulation supplying the contralateral lung, and type A4 refers to abnormalities of the aortic arch, including complete interruption (Fig. 26.1B). The root of the CAT is large and has a biventricular origin in most cases (overrides the septal defect). In up to a third of CAT cases, however, the root appears to arise entirely from the right ventricle and, in rare cases, entirely from the left ventricle. The CAT valve has three leaflets (tricuspid) in about 69% of cases, four leaflets (quadricuspid) in 22% of cases, two leaflets (bicuspid) in 9% of cases, and, on very rare occasions, one, five, or more leaflets (5). The two most commonly diagnosed types of CAT in the fetus are type 1/type A1 and type A4. Figure 26.2 shows an anatomic specimen of CAT type 1.
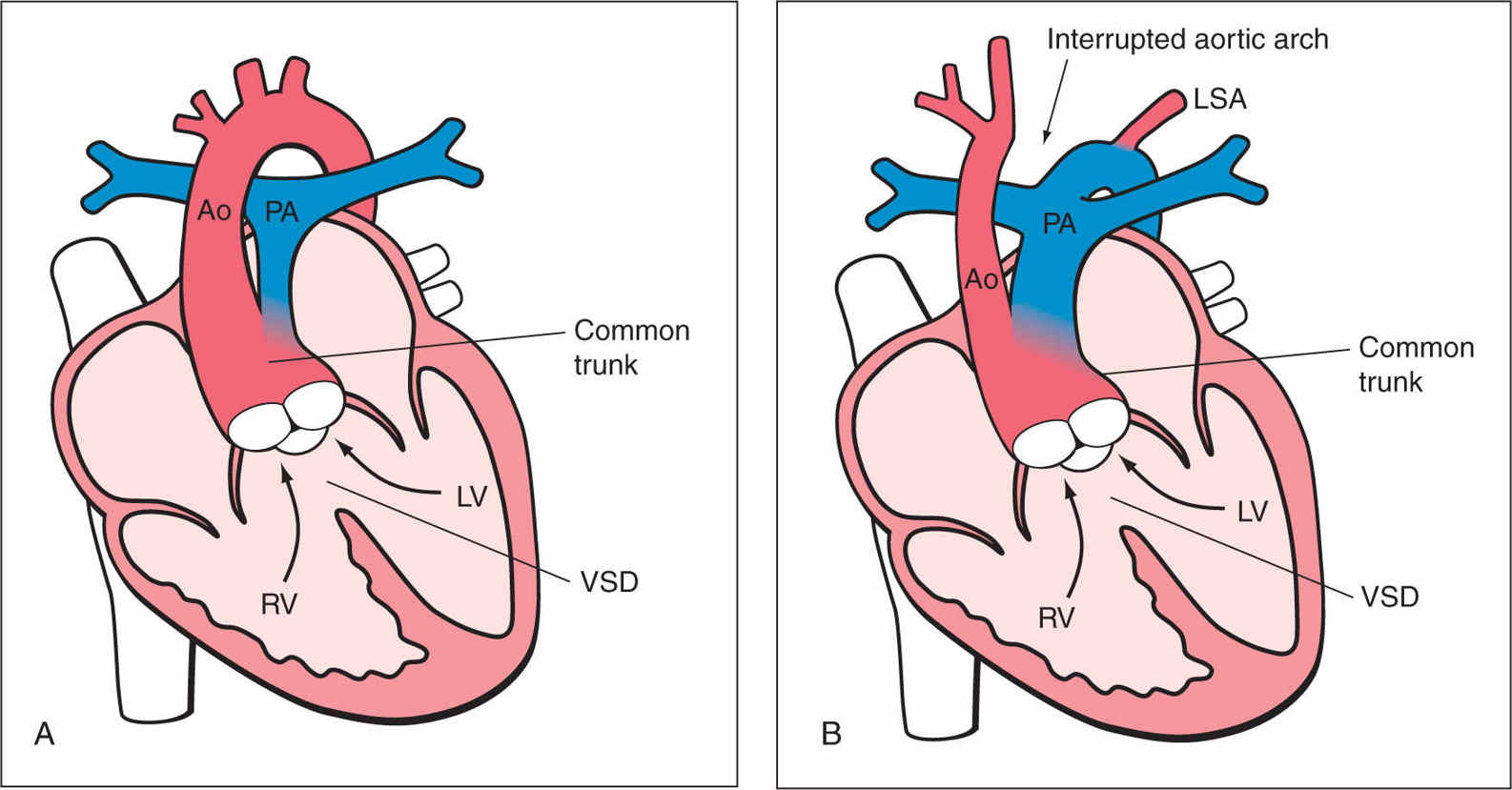
Figure 26.1: Schematic drawing of common arterial trunk (CAT) type 1 (A) and type A4 (B). See text for details. LV, left ventricle; RV, right ventricle; PA, pulmonary artery; Ao, aorta; LSA, left subclavian artery; VSD, ventricular septal defect.
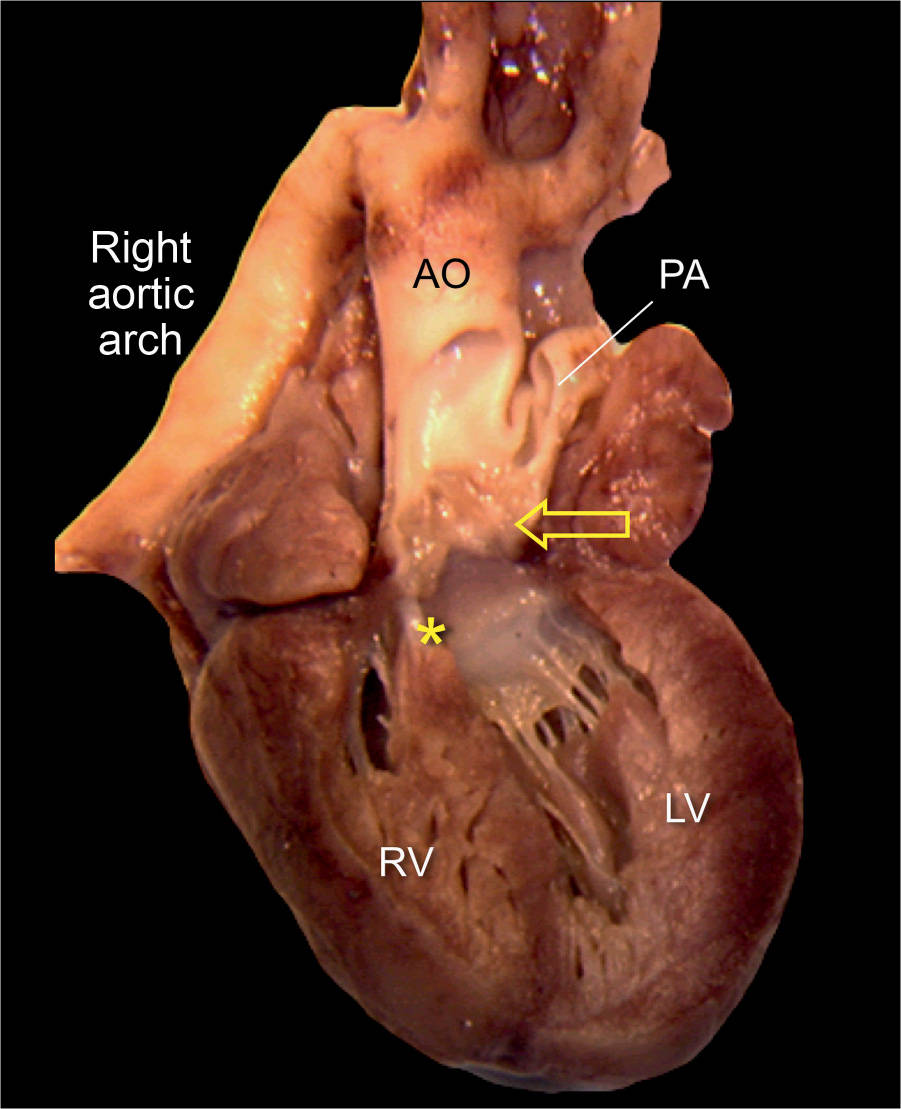
Figure 26.2: Anatomic specimen of common arterial trunk type 1 (compare to Fig. 26.1A). The common trunk (arrow) is open to demonstrate the dysplastic truncal valve and the bifurcation into the pulmonary artery (PA) and the aorta (AO). The ductus arteriosus is absent and a right aortic arch is noted. The asterisk shows a ventricular septal defect. RV, right ventricle; LV, left ventricle.
CAT is found in 1.6% of all newborns with congenital heart disease (6), is reported to occur in about 1.07 of 10,000 births (7), and is found more commonly in offspring of diabetic mothers (8). CAT occurs equally in boys and girls and is more commonly prevalent in fetal series (9). Associated chromosomal anomalies, mainly deletion 22q11, are common (10).
Ultrasound Findings
Gray Scale
The four-chamber view appears often normal in CAT (Figs. 26.3A and 26.4A) unless the VSD is large and visible in this plane, and a levorotation of the heart or a right aortic arch is present. The diagnosis is best achieved by detecting a malaligned VSD with an overriding large vessel on the five-chamber view (Fig. 26.4B) and an absence of a separate pulmonary artery and valve arising from the right ventricle. Confirming the diagnosis is usually made by identifying the pulmonary trunk (or arteries) arising directly from the overriding large vessel (Figs. 26.3B, 26.4B, and 26.5). In the five-chamber view, the root of the CAT is large and the valve leaflets are thickened (dysplastic) with lack of proper excursion (Fig. 26.5). Short-axis view may demonstrate an abnormal number of valve leaflets (Fig. 26.6). Identifying a short main pulmonary artery in the five-chamber view that arises from the large common trunk and courses to the left confirms the CAT diagnosis (type 1) and differentiates this abnormality from tetralogy of Fallot. In CAT type 1, the aorta is large and the pulmonary artery is narrow. In the CAT types 2 and 3, there is no pulmonary trunk, and the pulmonary arteries arise either posteriorly (type 2) or laterally (type 3) from the common trunk. Differentiating various CAT types is difficult and unreliable prenatally, especially in the second trimester (11). Differentiating a CAT type A4 with an interrupted aortic arch is, however, feasible by examining the size (Fig. 26.4) and the course of the great arteries. The three-vessel-trachea view is very helpful in the diagnosis (see also Chapter 9) as it will show a single large dilated vessel, representing the aortic arch, as the ductus arteriosus is not developed in more than 50% of cases (Fig. 26.7) (9) and the absence of continuity of the aortic isthmus when an interrupted aortic arch is present. In 70% of the cases, the aortic arch on the three-vessel-trachea view will be to the left of the trachea and in 30% to the right of the trachea, representing a right aortic arch. The thymus gland, which is also seen in the three-vessel-trachea view between the transverse aortic arch and the anterior thorax wall, is small or absent in about one-third of cases, a sign of a possible association with a microdeletion 22q11 (Fig. 26.7) (10, 12, 13).
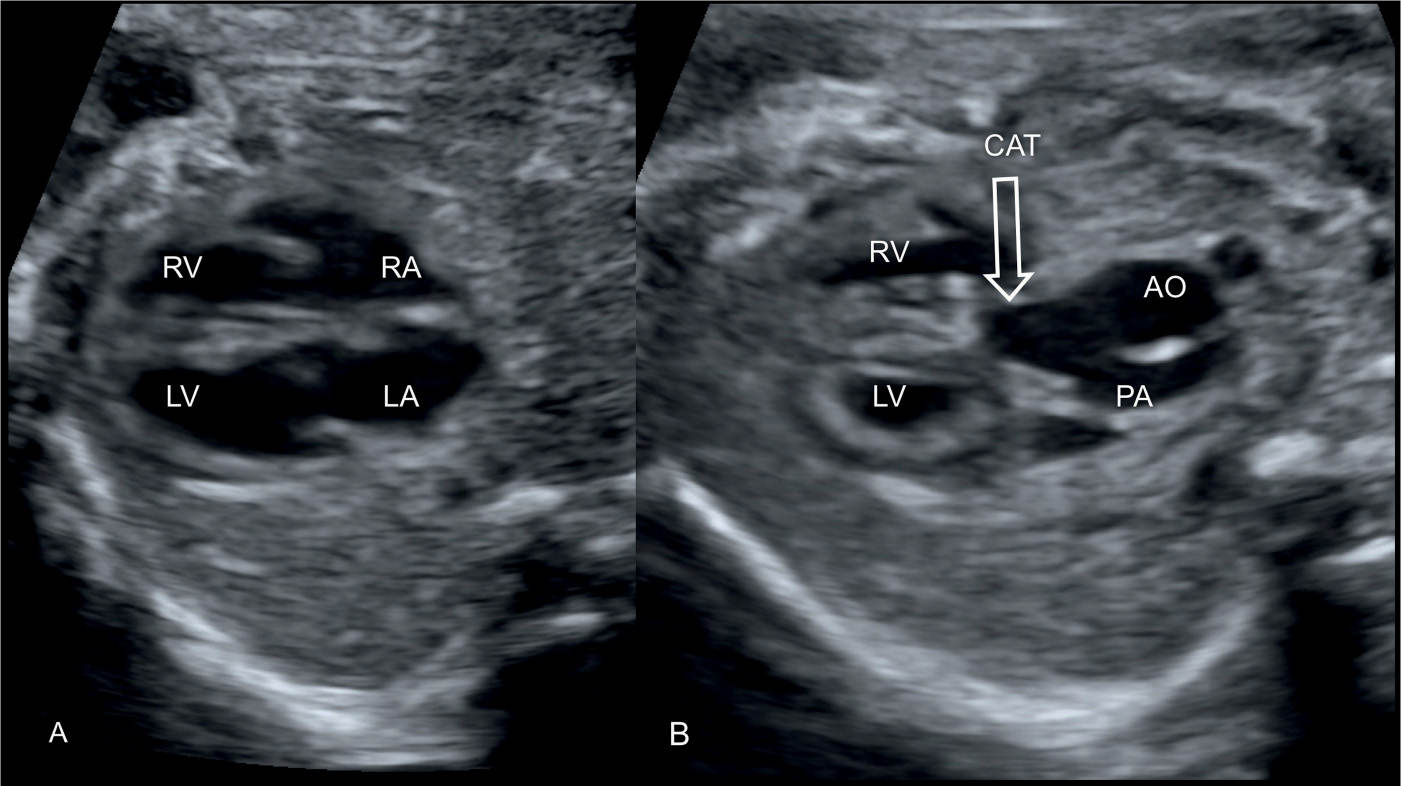
Figure 26.3: Transverse four-chamber (A) and five-chamber (B) views of a fetus with common arterial trunk (CAT). Note the normal appearing four-chamber view in A. In B, a CAT (arrow) is shown, giving origin to the aorta (AO) and pulmonary artery (PA). The narrow pulmonary artery in B suggests the presence of CAT type 1. LA, left atrium; RA, right atrium; LV, left ventricle; RV, right ventricle.
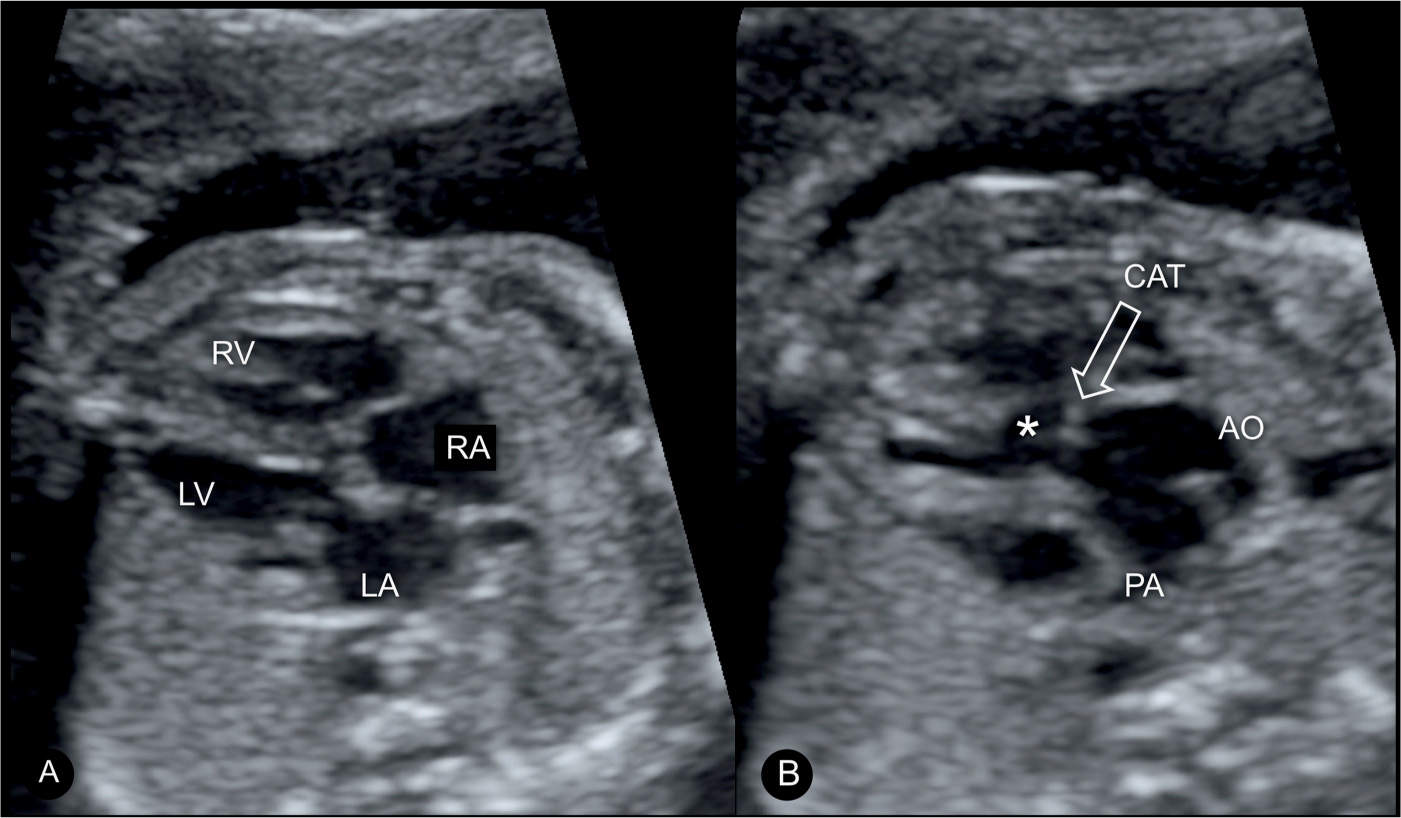
Figure 26.4: Transverse four-chamber (A) and five-chamber (B) views of a fetus with common arterial trunk (CAT). Note the normal appearing four-chamber view in A. In B, the ventricular septal defect (asterisk) and the large overriding CAT (arrow) are shown. The origin of a narrow aorta (AO) and a large pulmonary artery (PA), suggesting a CAT type A4 with an interrupted aortic arch, are shown. LA, left atrium; RA, right atrium; LV, left ventricle; RV, right ventricle.
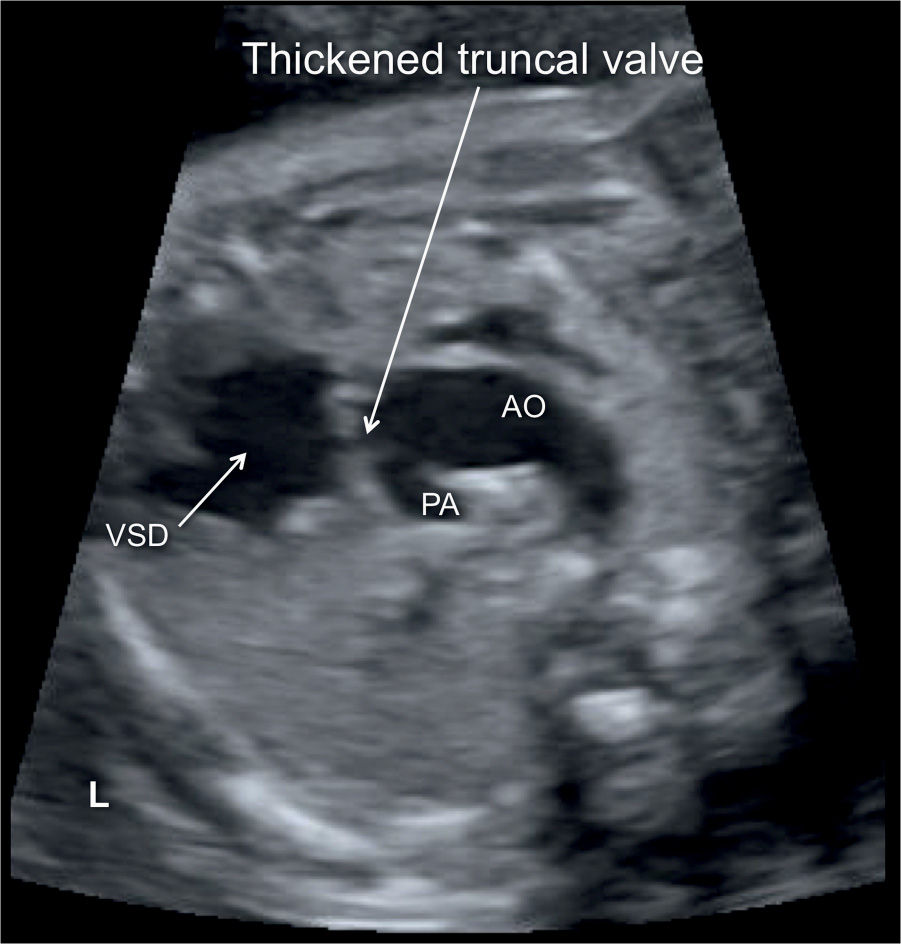
Figure 26.5: Transverse plane at the level of the five-chamber view demonstrating the large overriding common arterial trunk, bifurcating into the pulmonary artery (PA) and aorta (AO). Note the thickened and dysplastic truncal valve. VSD, ventricular septal defect; L, left.
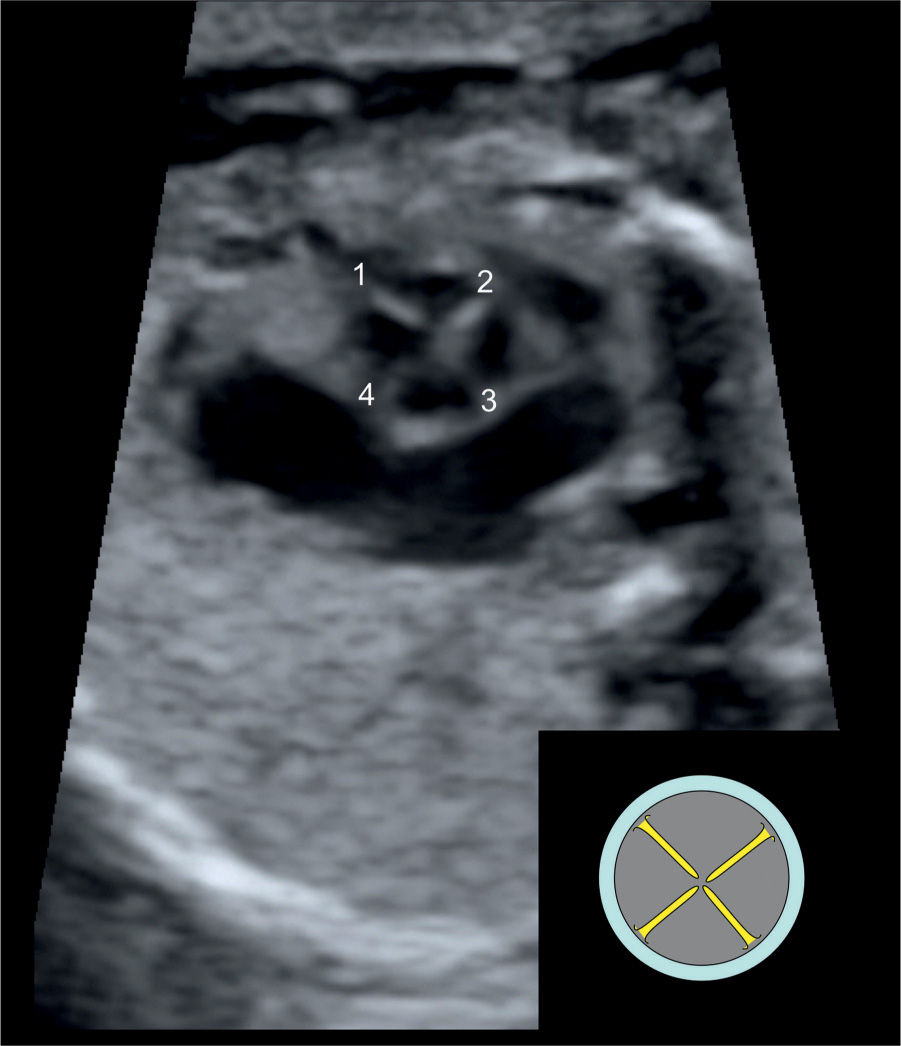
Figure 26.6: Short-axis view of the common truncal valve demonstrating the presence of a quadricuspid (four leaflets) valve (numbered 1–4).
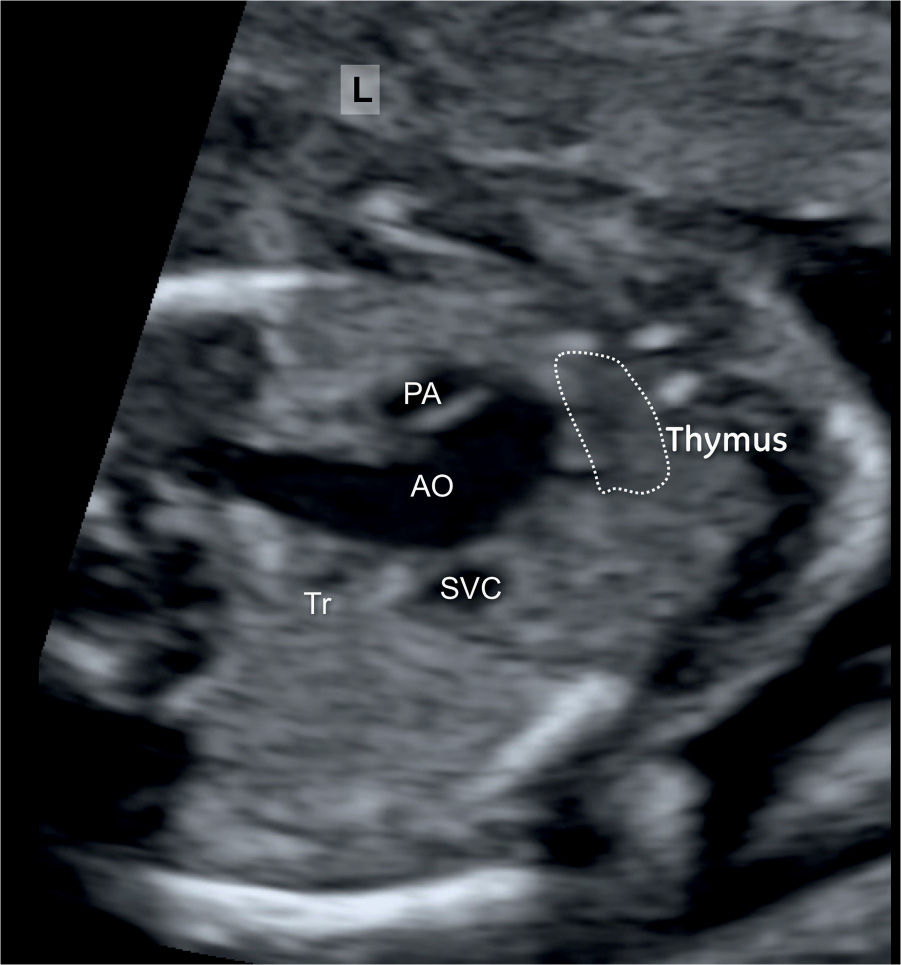
Figure 26.7: Three-vessel-trachea view in a fetus with common arterial trunk. Note the small pulmonary artery (PA) and the large aortic arch (AO). A hypoplastic thymus is shown as part of microdeletion 22q11 in this fetus. SVC, superior vena cava; Tr, trachea; L, left.
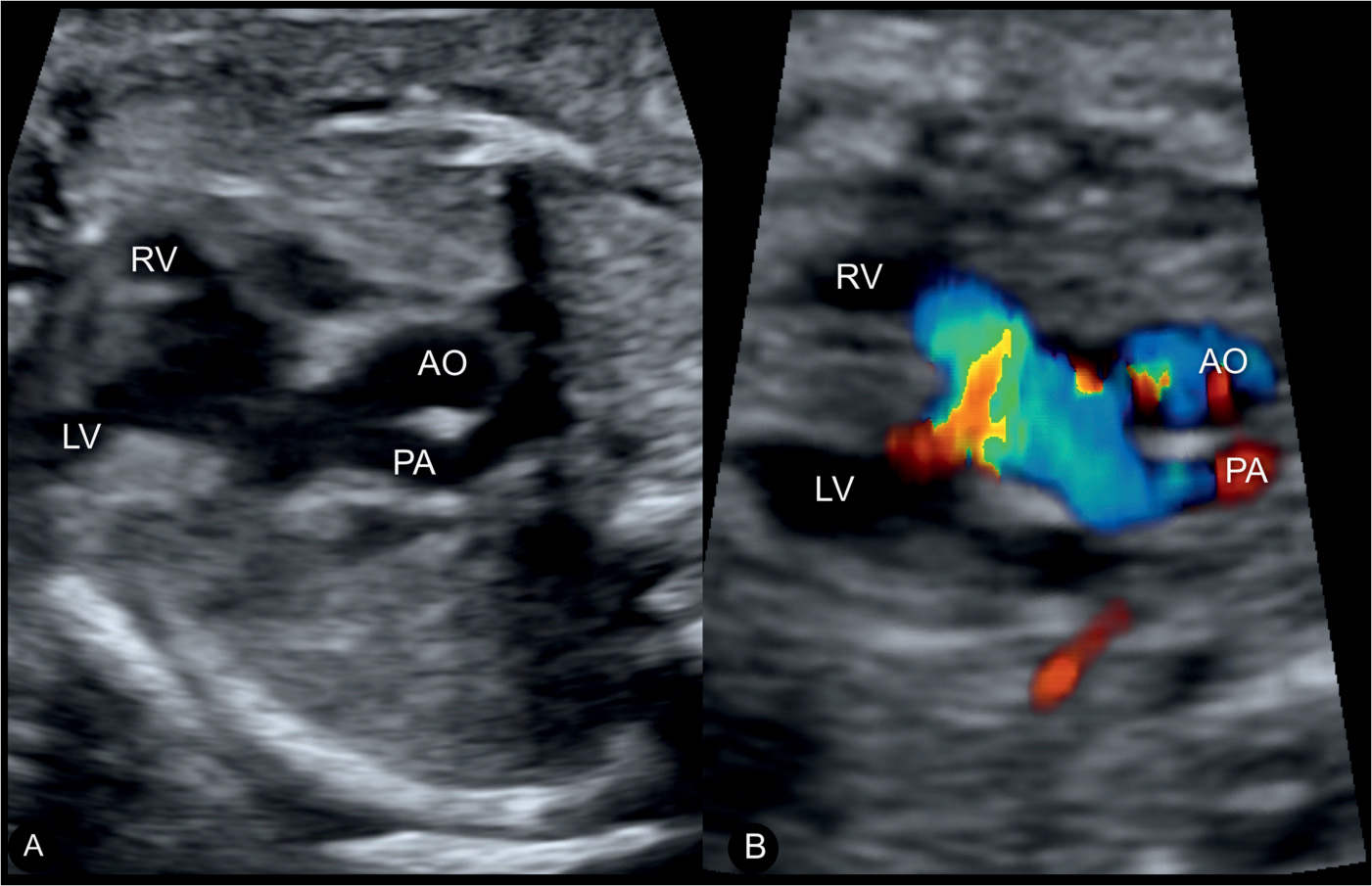
Figure 26.8: 2D (A) and color Doppler (B) of a common arterial trunk at the level of the five-chamber view. A shows a large overriding common arterial trunk bifurcating into the pulmonary artery (PA) and aorta (AO). B shows color aliasing at the valve level. RV, right ventricle; LV, left ventricle.
Color Doppler
Color Doppler may be helpful but is not necessary for the diagnosis of CAT. Color Doppler helps, however, in the demonstration of the shunt across the VSD and the high-velocity flow with color aliasing across the overriding CAT (Fig. 26.8). As a dysplastic truncal valve is a common finding in this anomaly, truncal valve regurgitation in diastole is often demonstrated in color Doppler (Figs. 26.9 to 26.12). The dysplastic truncal valve is, on occasions, stenotic and shows antegrade turbulent flow as well (Fig. 26.10). In CAT types 2 and 3, color Doppler helps to identify the origin and course of the right and left pulmonary arteries.
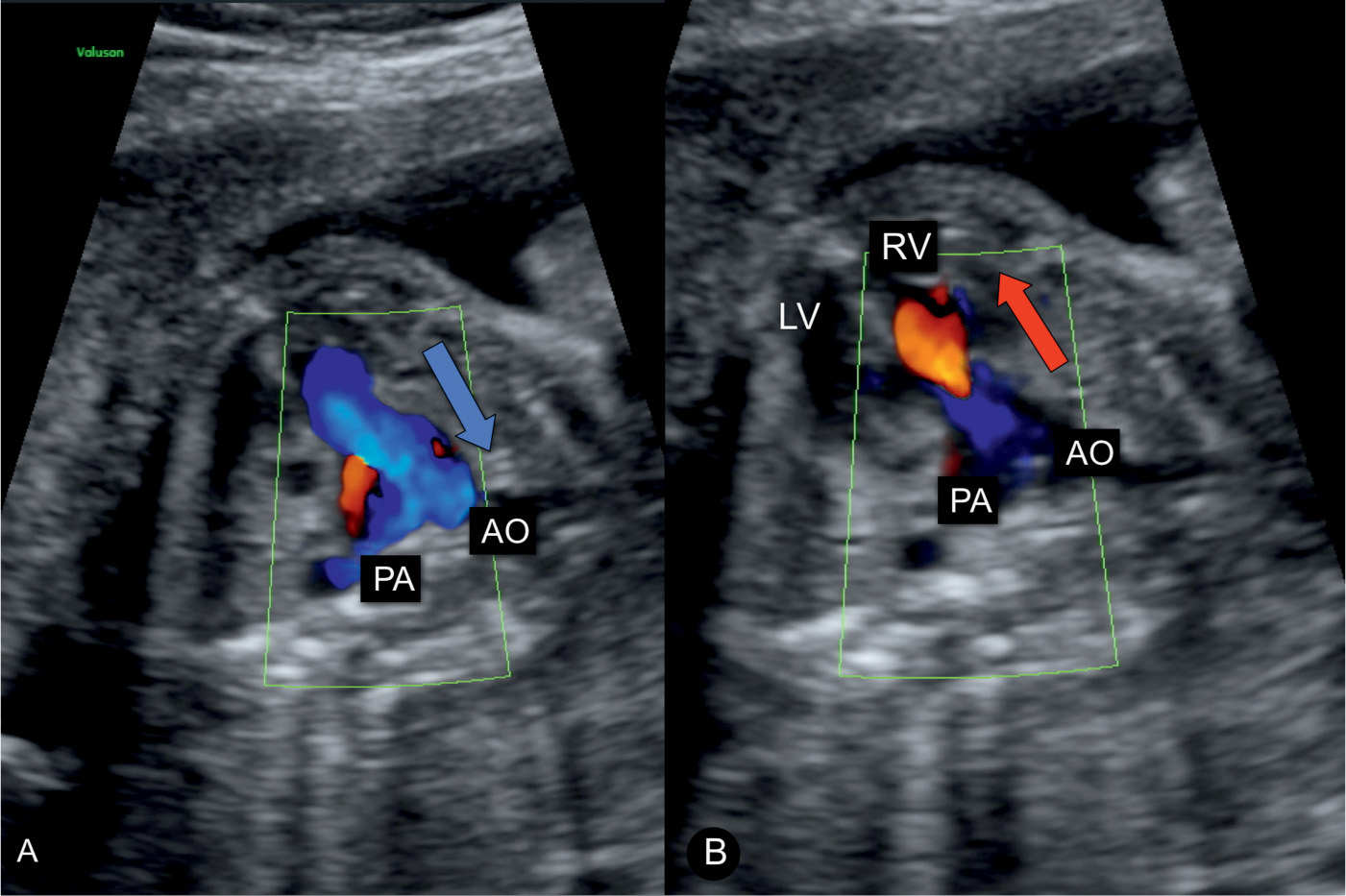
Figure 26.9: Color Doppler of a fetus with a common arterial trunk (CAT) in the apical five-chamber view with the typical dysplastic valve. A shows flow in systole (A) into the aorta (AO) and pulmonary artery (PA) (blue). In B, CAT valve regurgitation (red) into the right ventricle (RV) is noted during diastole. The presence of CAT valve regurgitation is due to the dysplastic nature of the valve. Compare with Figures 26.10 to 26.12. LV, left ventricle.
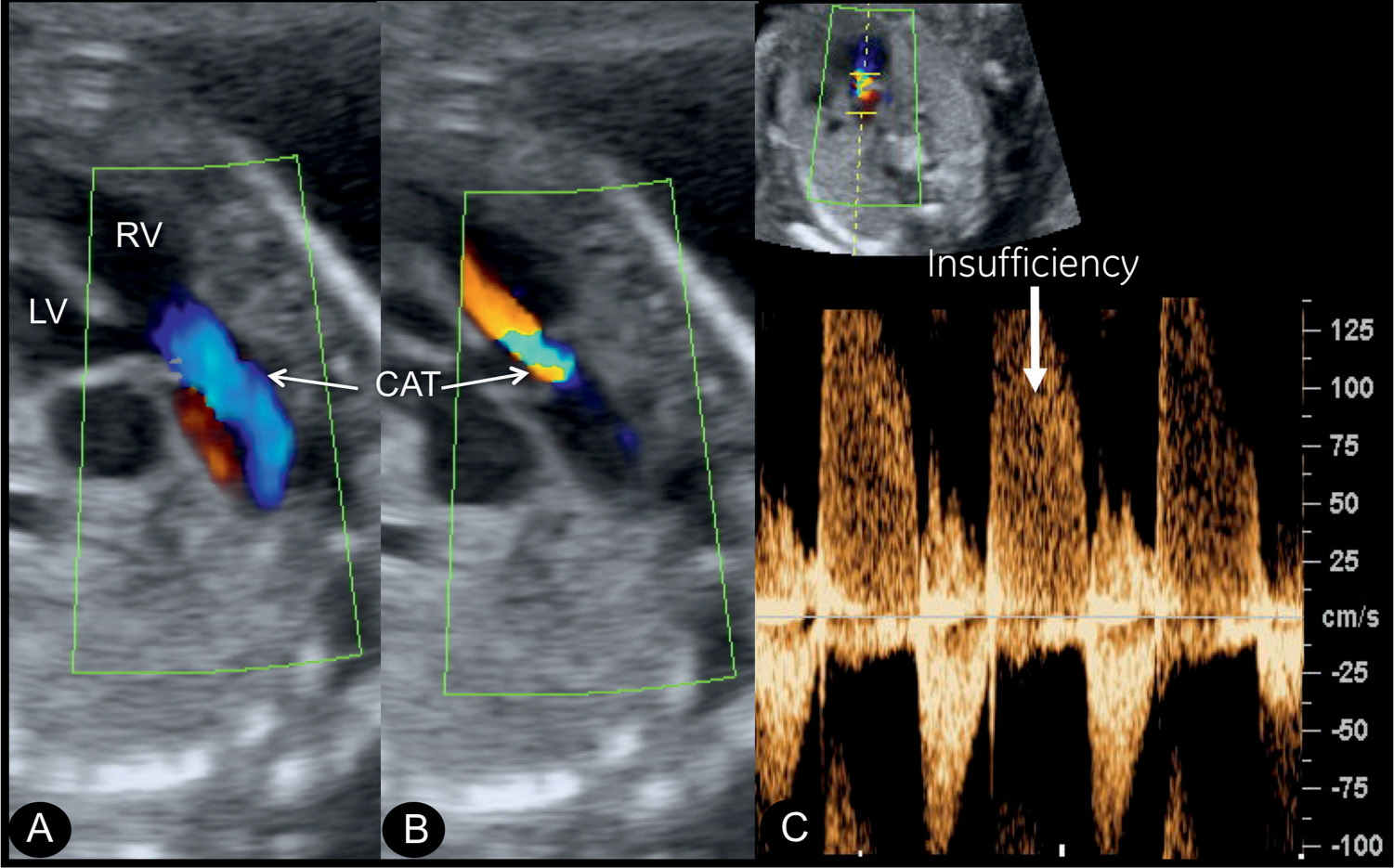
Figure 26.10: Color and spectral Doppler of the common arterial trunk (CAT) valve. A shows flow on color Doppler into the CAT during systole (blue). B demonstrates severe regurgitation on color Doppler during diastole (red). C shows holodiastolic severe regurgitation of blood on spectral Doppler (arrow) with valvular stenosis (peak velocity >100 cm/s). LV, left ventricle; RV, right ventricle.
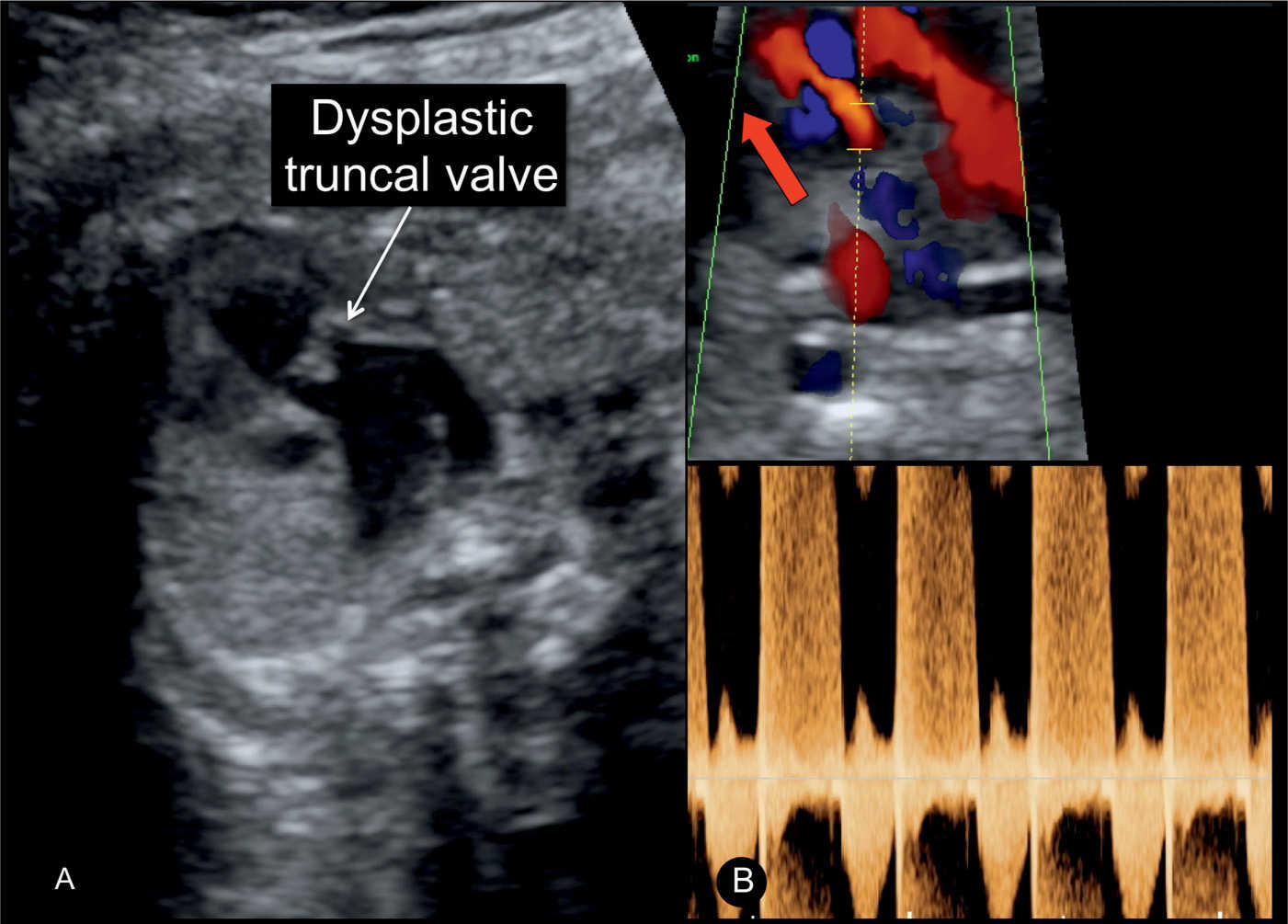
Figure 26.11: Gray scale (A) and color with spectral Doppler (B) of the five-chamber view in a fetus with common arterial trunk (CAT) with dysplastic valves (same fetus as in Fig. 26.4). A shows thickening of the valve leaflets (arrow). B demonstrates severe holodiastolic valve regurgitation on color (red) and spectral Doppler in diastole. Compare with Figure 26.10.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


