● INTRODUCTION
Understanding the spatial relationship and anatomy of the cardiac chambers is an essential prerequisite step to the ultrasound evaluation of the fetal heart. The cardiac chambers differ in their internal anatomy and have specific characteristics that allow for their ultrasound identification in normal and abnormal conditions. Given that an abnormal four-chamber view on ultrasound has a high association with the presence of congenital heart disease, the ability to recognize normal and abnormal anatomy of cardiac chambers is thus of paramount importance and is essential to the performance of the basic and detailed ultrasound evaluation of the fetal heart. In Chapter 5, we presented a detailed review of the anatomic features of the cardiac chambers. In this chapter, we present the ultrasound characteristics of the four-chamber and short-axis views of the fetal heart.
● THE FOUR-CHAMBER VIEW
The four-chamber view is considered one of the most important planes to be imaged during fetal cardiac scanning (Fig. 7.1). The four-chamber view was the first plane to be introduced to the sonographic assessment of the fetal heart (1), and it has consistently been shown to detect numerous cardiac defects (2). The four-chamber view on ultrasound is easy to obtain in all fetal positions, and it represents the starting plane for the basic and detailed evaluation of the fetal heart. Advantages of the four-chamber view include visualization of atria and ventricles, the atrioventricular valves, and the atrial and ventricular septa. The four-chamber view is one of the required planes for fetal cardiac screening guidelines (Chapter 2) (3, 4).
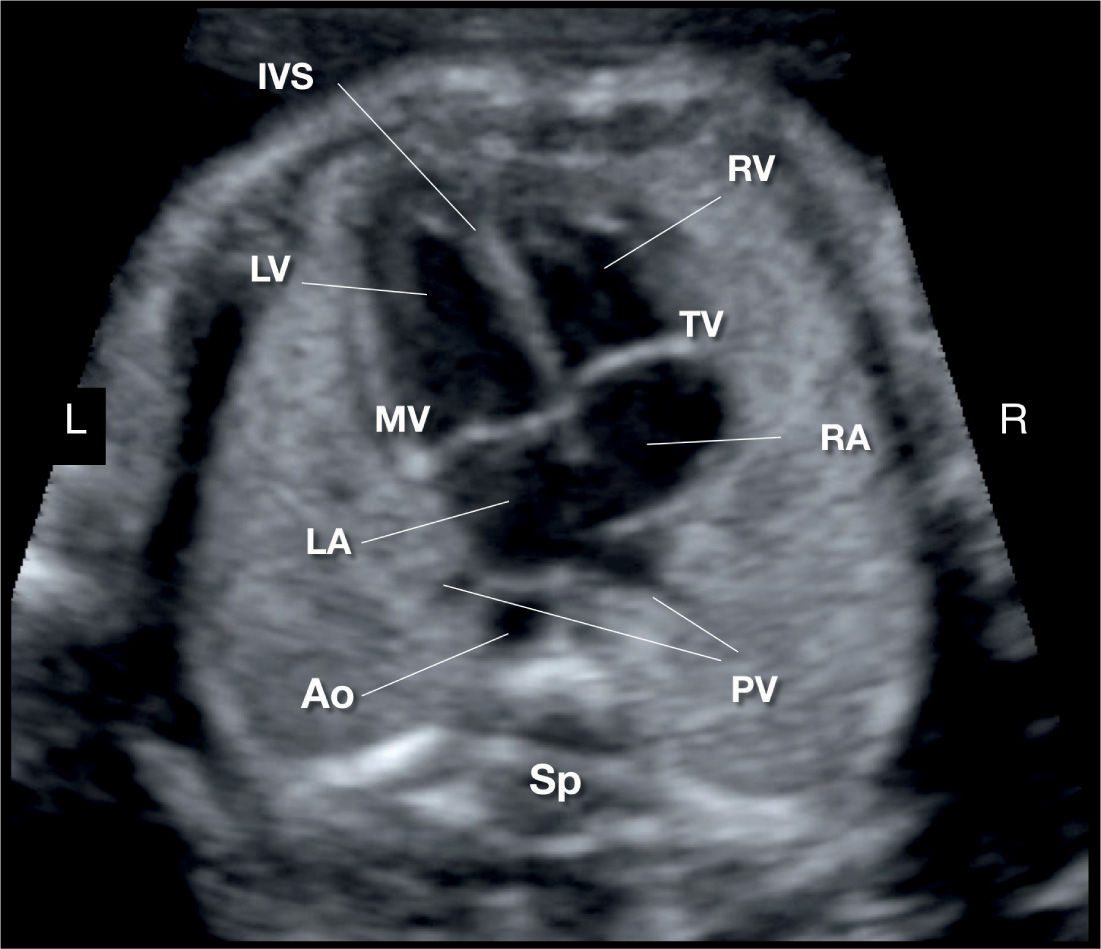
Figure 7.1: Apical four-chamber view of the fetal heart showing the right atrium (RA), left atrium (LA), right ventricle (RV), left ventricle (LV), and interventricular septum (IVS). Note the more apical insertion of the tricuspid valve (TV) in relation to the mitral valve (MV). The right and left (inferior) pulmonary veins (PV) are seen entering the left atrium posteriorly on either side of the descending aorta (AO). Sp, spine; L, left; R, right.
Scanning Technique
1. Determine the fetal situs, as previously described in Chapter 6.
2. Obtain a transverse plane of the fetal abdomen. In a perfect transverse plane of the fetal abdomen, a complete fetal rib is imaged along each of the two lateral abdominal walls (Fig. 7.2). When multiple ribs are imaged along the two lateral abdominal walls, an oblique rather than a transverse plane is obtained (Fig. 7.2).
3. From a transverse plane of the fetal abdomen, slide the transducer toward the fetal chest, maintaining the transverse plane, until the four-chamber view is imaged. The optimum plane for the visualization of the four-chamber view requires the following anatomic markers: one complete (or near complete) rib on each side of the fetal lateral chest wall, the two inferior pulmonary veins noted along the posterior wall of the left atrium, and the apex of the heart. Table 7.1 lists the anatomic characteristics of the normal four-chamber view.
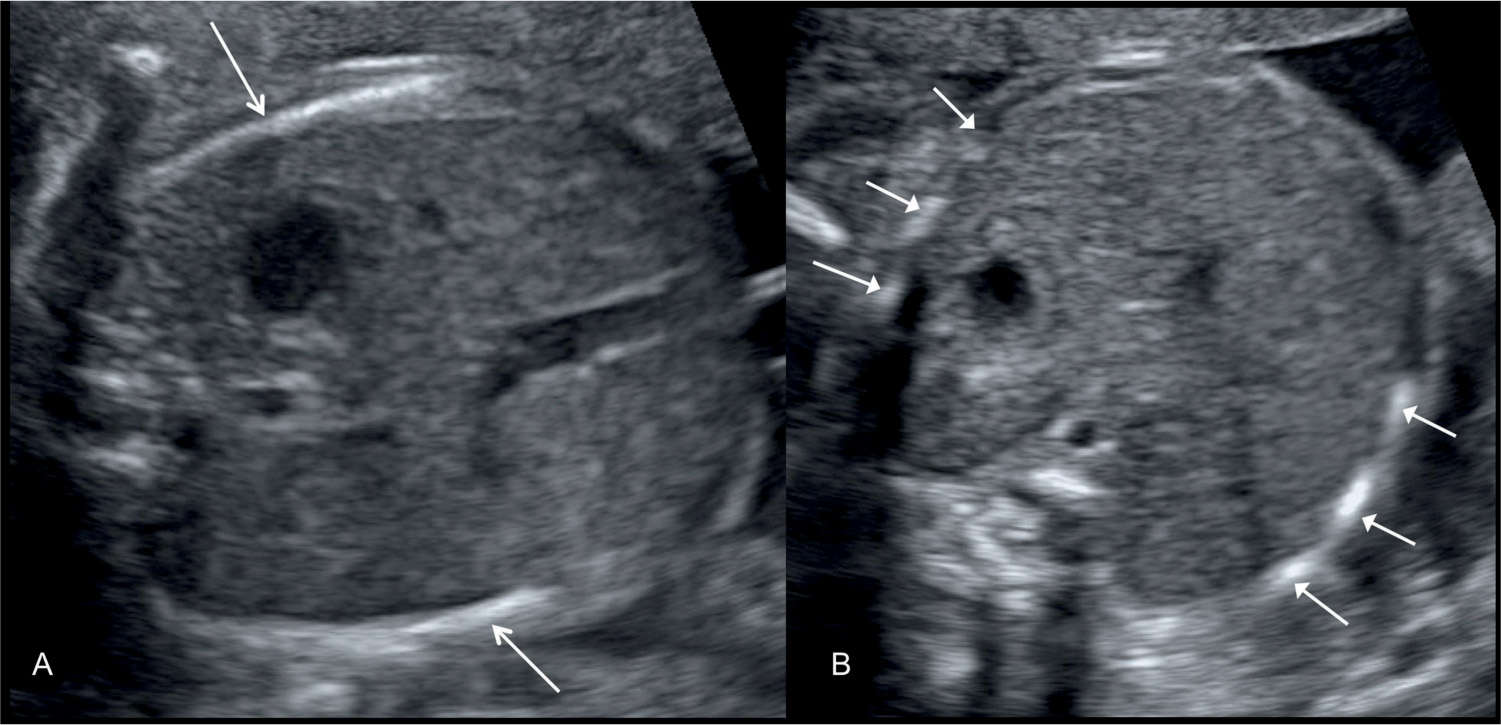
Figure 7.2: A: Transverse view of the fetal abdomen at the level of the stomach. Note the presence of a significant portion of one rib at each lateral abdominal wall (arrows). This ensures a near-perfect transverse plane of the abdomen. B: Oblique view of the fetal abdomen at the level of the stomach. Note the presence of multiple segments of ribs at each lateral abdominal wall (arrows).
• Normal-size heart in chest • Transverse plane of fetal chest with one complete rib on each side of fetal lateral chest wall • Descending aorta in front and to the left of the fetal spine • Apex of fetal heart pointing to the left upper chest at about a 45-degree angle • Atria equal in size • Foramen ovale in midsection of atrial septum with leaflet of foramen ovale in left atrium • Two inferior pulmonary veins, seen as slit-like opening in posterior wall of left atrium • Patent atrioventricular valves • Tricuspid valve septal leaflet more apically inserted on the septum than mitral valve • Ventricles equal in size and contractility • Intact ventricular septum • Moderator band in right ventricular apex |
Evaluation of the Four-Chamber View
Orientation
The fetal heart lies almost horizontally in the thorax with the four-chamber view plane obtained in almost the same plane as a transverse plane of the chest. In postnatal life, the cardiac apex swings inferiorly and the heart is thus positioned more vertically in the thoracic cavity. The fetal rib corresponding to a four-chamber view plane of the fetal heart is the fourth thoracic rib (5).
As stated, a significant advantage of the four-chamber view is that it can be fairly easily obtained in all fetal positions. Based on the position and fetal lie in the uterus, four types of four-chamber views of the fetal heart can be obtained (Fig. 7.3):
1. When the fetal anterior chest wall is closest to the transducer, an apical four-chamber view is obtained (Fig. 7.3A). In this fetal position, the ultrasound beam is nearly parallel to the ventricular septum, and it insonates the apical portion of the fetal heart first.
2. When the fetal right posterior chest wall is closest to the transducer, a basal four-chamber view is obtained (Fig. 7.3D). In this fetal position, the ultrasound beam enters the fetal chest inferior to the right shoulder; nearly parallel to the ventricular septum and it insonates the base of the fetal heart first.
3. When the fetal spine is neither anterior nor posterior but closer to the right or left lateral uterine walls, a lateral four-chamber view (axial) is obtained either from the left (Fig. 7.3C) or from the right (Fig. 7.3B). In this fetal position, the ultrasound beam is nearly perpendicular to the ventricular septum.
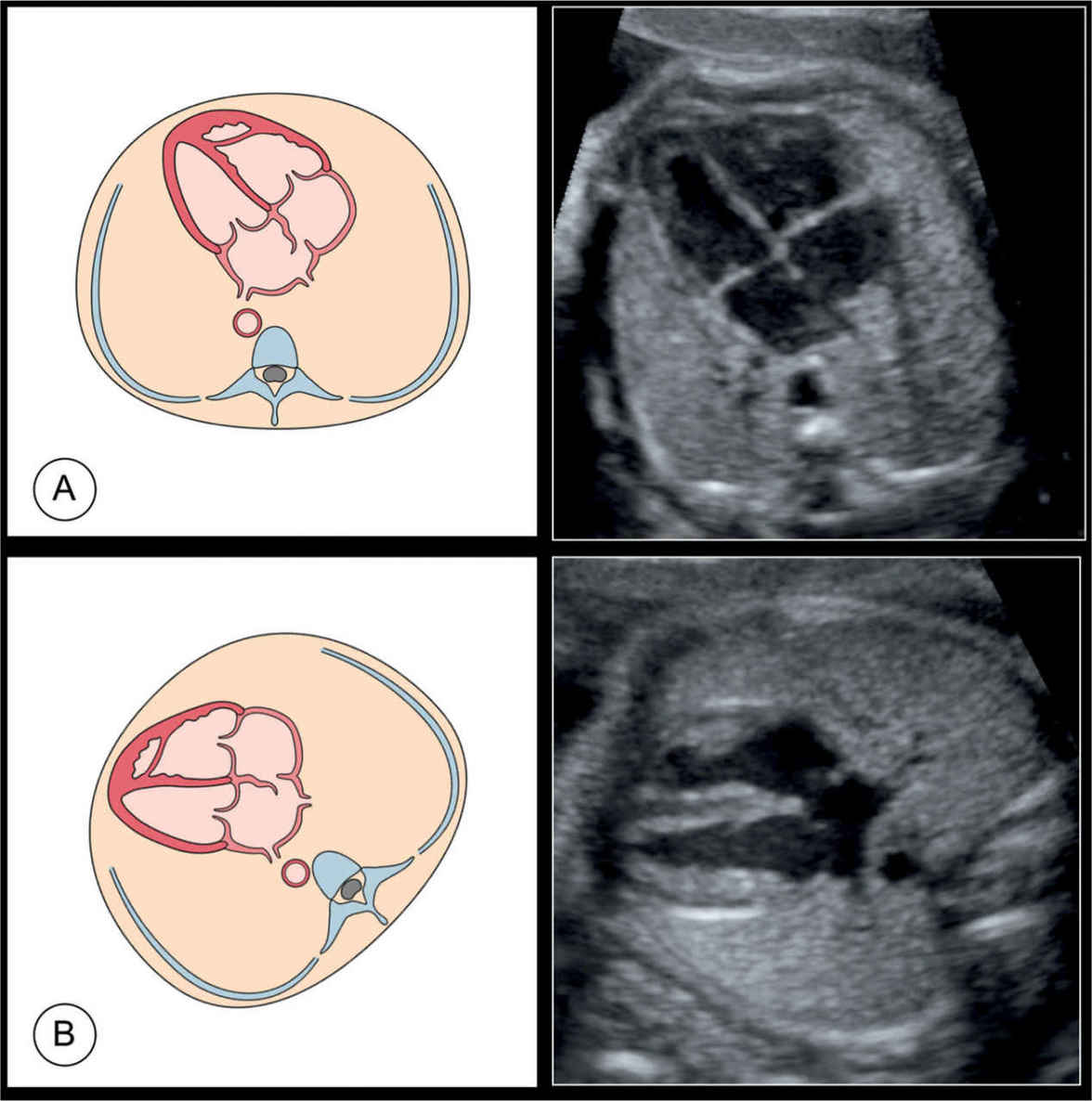
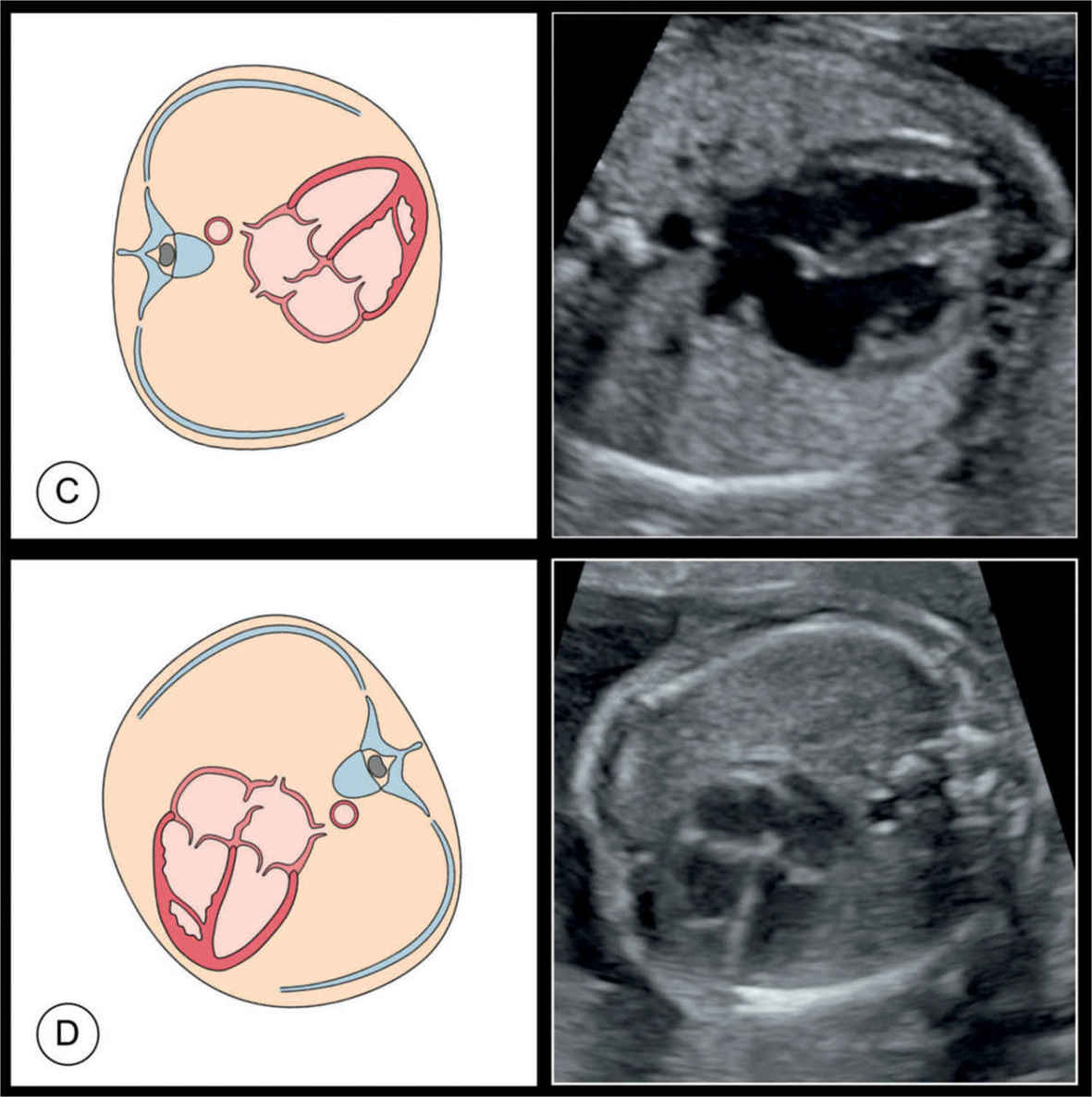
Figure 7.3: Schematic drawings and corresponding ultrasound images of four-chamber views in four fetuses: fetus A with a posterior spine position, fetus B with a right lateral spine position, fetus C with a left lateral spine position, and fetus D with an anterior spine position. Advantage of the four-chamber view is that it can be obtained from various positions of the fetus in utero.
Evaluation of all the anatomic details that the four-chamber view provides often requires examination of more than one type of four-chamber view. This is usually accomplished by insonating the fetal heart from opposite sides of the maternal abdomen. The apical view allows optimal visualization of the apex of the heart, the ventricles, the atrioventricular valves, and longitudinal atrial and ventricular dimensions. The primum area of the atrial and ventricular septa, however, is usually inadequately imaged by the apical view. This is due to the longitudinal orientation of the ultrasound beam to the septa in the apical view, making it appear thinner than it actually is with the potential for false diagnosis. The basal view allows adequate visualization of the atria and the atrioventricular valves. The lateral (axial) views allow adequate visualization of the atrial and ventricular septa, atrial and ventricular walls, ventricular contractility, and septal thickness. Valvular attachments are not adequately assessed in the lateral views.
Heart Position and Axis
By drawing a line from the spine posteriorly to the sternum anteriorly that bisects the chest into two equal halves (Fig. 7.4A), the heart is divided into two parts: one part is in the right chest and has about one-third of the heart mass, and a second part is in the left chest and has about two-thirds of the heart mass. The normal cardiac axis points to the left with an angle of about 45 degrees (Fig. 7.4A). For further details on the thoracic situs, cardiac position, and axis, see Chapter 6.
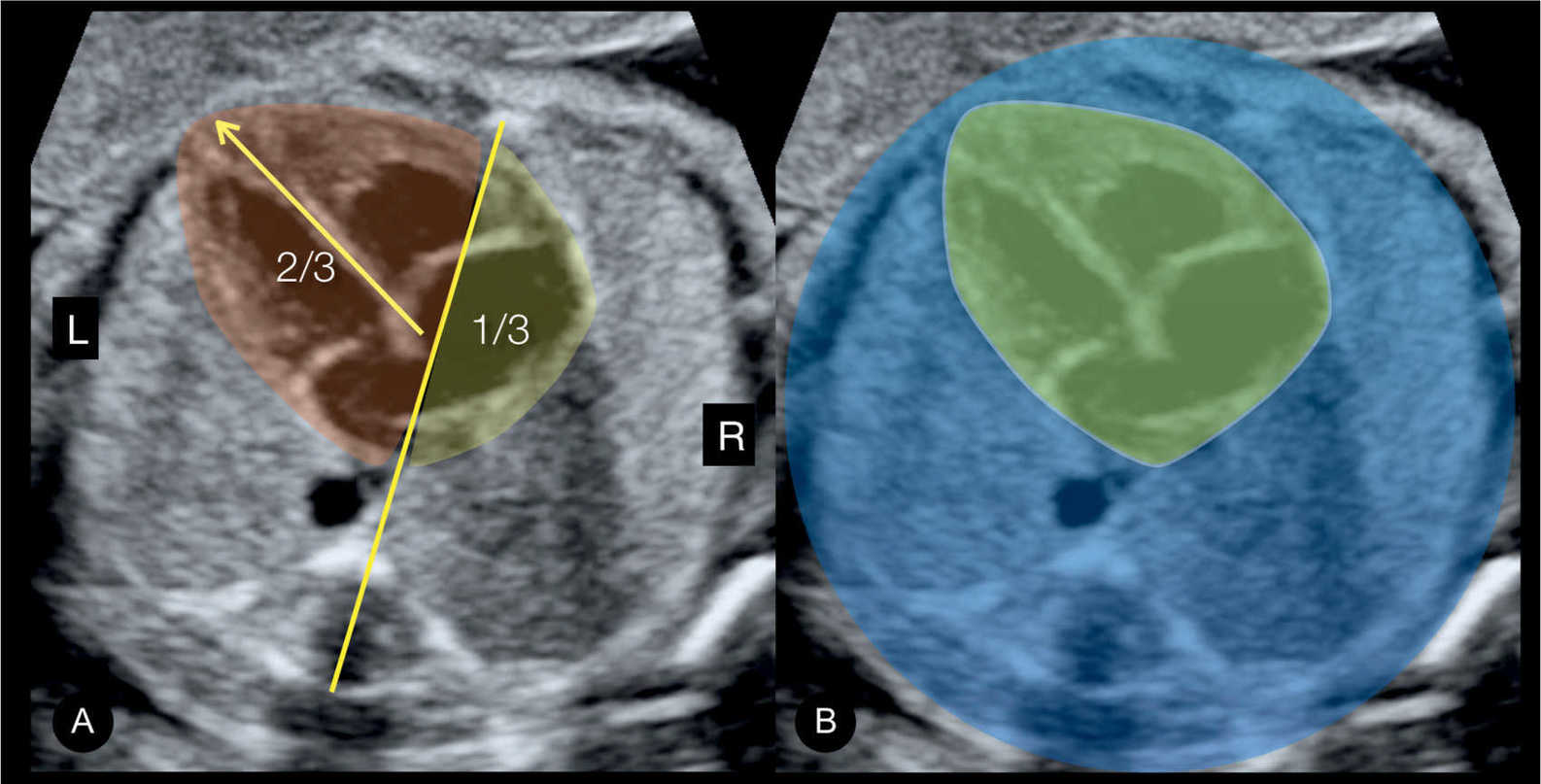
Figure 7.4: Four-chamber view in gray scale in A and B (same fetus) showing the anatomic position of the heart in the chest. In A, an imaginary line is drawn from the spine posteriorly to the sternum anteriorly, dividing the thorax in two equal parts: left (L) and right (R). Note in A the anatomic location of the normal heart (shaded), with one-third in the right chest and two-thirds in the left chest. The cardiac axis (arrow in A) points to the left side (compare with Figure 6.4). In B, the heart is shaded in green and the remainder of the chest in blue. Note that the area of the heart occupies about one-third of the chest area.
Heart Size
The heart size, assessed as surface area and circumference, is about one-third to one-half that of the thoracic cavity in transverse view (Fig. 7.4B). The width of the heart, at the level of the atrioventricular valves, corresponds approximately to gestational age in weeks (see also Chapter 17). Fetal cardiac dimensions can be easily assessed by measuring the ratio of cardiac circumference or area to the chest circumference or area obtained at the level of the four-chamber view. The cardiothoracic (C/T) circumference is fairly constant throughout gestation, with a mean value of 0.45 at 17 weeks and 0.50 at term (6). The mean C/T circumference in the first half of pregnancy increases slightly with gestational age, from 0.38 at 11 weeks to 0.45 at 20 weeks, with all values at less than 0.50 in normal fetuses (7). The C/T area is an alternate method for assessing cardiac dimensions, and normal values are fairly constant throughout gestation, with a mean value between 0.25 and 0.35 (8). Fetal cardiomegaly, defined as C/T area greater than two standard deviations in one series, encompasses heterogeneous etiologies, including cardiac and extracardiac abnormalities (8). Holosystolic tricuspid regurgitation with right atrial enlargement is a common feature and is seen in almost 90% of fetal cardiomegaly cases (8). Table 7.2 lists common causes of fetal cardiomegaly.
An increased C/T circumference can also be observed in the presence of reduced chest volume rather than an enlarged heart, and thus, it is important to compare the measured chest circumference to gestational age nomograms as part of this evaluation. Reduced chest circumference can result from some forms of lethal skeletal dysplasias or in the presence of severe pulmonary hypoplasia. Reduced chest circumference is typically associated with a poor outcome.
Heart Contractility
Assessing chamber contractility in real-time ultrasound is part of the evaluation of the four-chamber view. In the normal fetal heart, left and right ventricular contractility should be equal without any paradoxical movements of the interventricular septum.
ETIOLOGY |
|
Cardiac | Ebstein anomaly Tricuspid valve dysplasia Atrioventricular septal defect Sustained fetal arrhythmia (heart block) Dilative cardiomyopathy Premature constriction of ductus arteriosus |
Extracardiac | Arteriovenous malformations as sacrococcygeal teratoma, aneurysm of vein of Galen, and placental chorioangioma Recipient in twin–twin transfusion syndrome Severe fetal anemia Uncontrolled maternal diabetes |
Heart Rhythm
Fetal cardiac rhythm should be evaluated and noted to be regular with no extra beats as in ectopic beats or other irregularities. The normal range of cardiac rhythm in the fetus is between 120 and 160 beats per minute. Ranges between 110 and 180 beats per minute are commonly associated with a normal status.
The Right and Left Atria and the Interatrial Septum
The left atrium is the most posterior cardiac chamber and is recognized by the drainage of the pulmonary veins and the leaflet of the foramen ovale (Fig. 7.5). The leaflet of the foramen ovale (flap) is the moving part of the septum primum and it flaps into the left atrium during atrial filling with a right-to-left shunt. The leaflet of the foramen ovale has a wide variation in size and shape as it flaps into the left atrium. It typically appears as a semilunar reflective membrane and is best seen using the lateral (axial) four-chamber view. The left atrium is anterior and to the left side of the thoracic descending aorta (Fig. 7.5 and see anatomic correlate in Fig. 5-2). The right atrium is on the right side of the left atrium and communicates with the left atrium via the foramen ovale (i.e., the ostium secundum). By slightly angling the transducer cranially or caudally, the superior or inferior vena cava can be seen, respectively. Rotating the transducer about 90 degrees will display both the superior and inferior venae cavae entering the right atrium in the bicaval plane. Both atria are nearly equal in size and are best recognized by their respective venous connections.
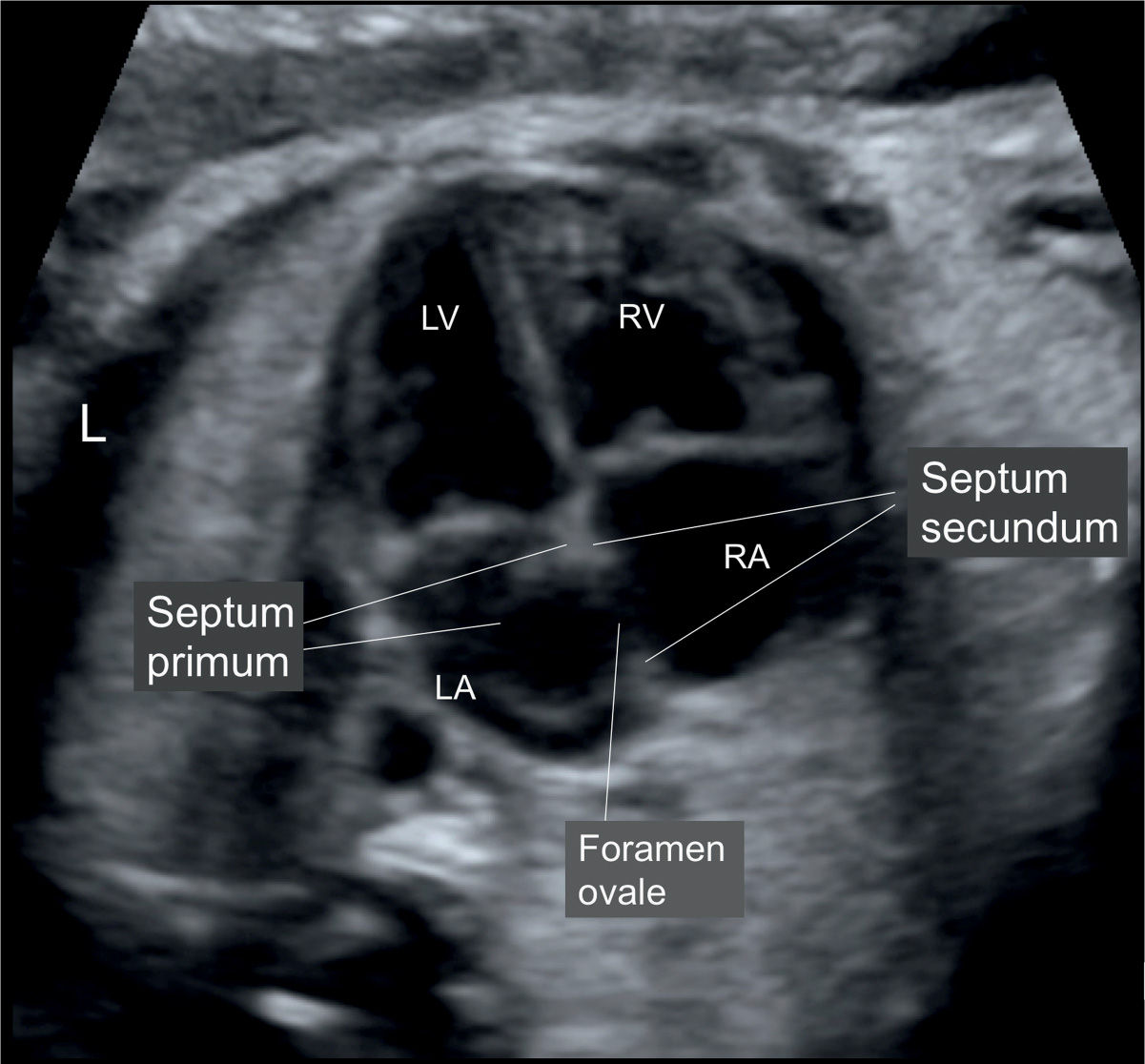
Figure 7.5: Apical four-chamber view of the fetal heart in gray scale. The apical view is preferred for the evaluation of the atria and interatrial septum. Note the clear visualization of the right (RA) and left (LA) atrium. The interatrial septum, noted between the RA and LA, is formed by the septum primum and secundum. The foramen ovale (FO) is an opening in the midportion of the septum secundum, and its flap is formed by the septum primum. L, left; RV, right ventricle; LV, left ventricle. (Compare with anatomic specimen in Figure 5.2.)
On occasions, the Eustachian valve can be imaged in a four-chamber view plane that is posterior to the optimal plane, where it can be mistaken for the flap of the foramen ovale. The coronary sinus, which delivers venous return from the heart, runs across the atrioventricular groove posteriorly and enters the right atrium inferiorly in proximity to the atrial septum (1) (see Chapter 10).
Visualization of the atrial appendages can help in differentiating the right from left atrium in normal and abnormal conditions. The left atrial appendage is finger-like and has a narrow base, whereas the right atrial appendage is pyramidal in shape with a broad base. The appendages can be imaged in a plane slightly cranial to the four-chamber view, but their visualization in this plane is technically challenging and limited under many conditions. The right atrial appendage is more easily displayed in the bicaval view. The clinical usefulness of the atrial appendages imaging is discussed in more detail in Chapter 30.
The Right and Left Ventricles
The right ventricle is the most anterior cardiac chamber as it lies directly behind the sternum (Fig. 7.6). The left ventricle is adjacent and posterior to the right ventricle, and is the most left-sided cardiac chamber (Fig. 7.6). As discussed in Chapter 5, many anatomic features allow the differentiation of the right and the left ventricles (Fig. 7.6). At the four-chamber view plane, the right ventricle appears trabeculated with a somewhat irregular cavity, whereas the left ventricular walls are smooth (Fig. 7.6). The lumen of the left ventricle appears longer than that of the right ventricle primarily due to the moderator band (septomarginal trabeculum) within the right ventricle. The moderator band courses from the interventricular septum to the lower free wall of the right ventricle. The apex of the fetal heart is primarily formed by the left ventricle.
The ventricles can also be recognized through their corresponding atrioventricular valves: the mitral valve in the left ventricle and the tricuspid valve in the right ventricle. The septal leaflet of the tricuspid valve inserts more apically on the interventricular septum than the mitral valve (Fig. 7.6). This represents a very important anatomic feature that is typically absent in atrioventricular septal defects (AVSDs). Three papillary muscles with chordae tendineae attachments help to anchor the tricuspid valve. Some tricuspid valve chordae tendineae insert directly into the septal free wall, a differentiating feature that is only found in the right ventricle, and can be best recognized in the lateral view to the heart (Fig. 7.7). In the left ventricle, all the chordae tendineae from the two mitral valve leaflets insert into two—anterolateral and posteromedial—papillary muscles, with no chordae tendineae attachment to the free wall (Fig 7.7).
We encourage the use of the cine-loop function in the ultrasound equipment while imaging the atrioventricular valves (Fig. 7.8). Appearance and motion of valve leaflets during diastole and systole can thus be visualized more clearly.
The Interventricular Septum
The interventricular septum (septum) separates the right from left ventricle. The septum is wide at the apex of the heart, and thins out as it reaches the level of the atrioventricular valves (Fig. 7.7). This is related to the anatomic features of the septum, as it is muscular at its lower two-thirds and membranous at its upper one-third, at the junction of the atrioventricular and semilunar valves (see anatomic correlate in Fig. 5-12). Before 20 weeks of gestation, the thin membranous part of the septum is not optimally visualized by an apical four-chamber view (Fig. 7.9). This is primarily due to echo dropout, which may lead to a false-positive diagnosis of septal defects (Fig. 7.9). When a septal defect is suspected on apical views, confirmation should be obtained in lateral views, which allow for better visualization of the septum (Fig. 7.9). The presence of an echogenic line (T-line), at the level of the septal defect in apical views, may also help to confirm the diagnosis (see Chapter 18). A lateral four-chamber view should be used to measure the thickness of the septum (normal range between 2 and 4 mm) and measurement should be performed at the thickest portion of the septum.
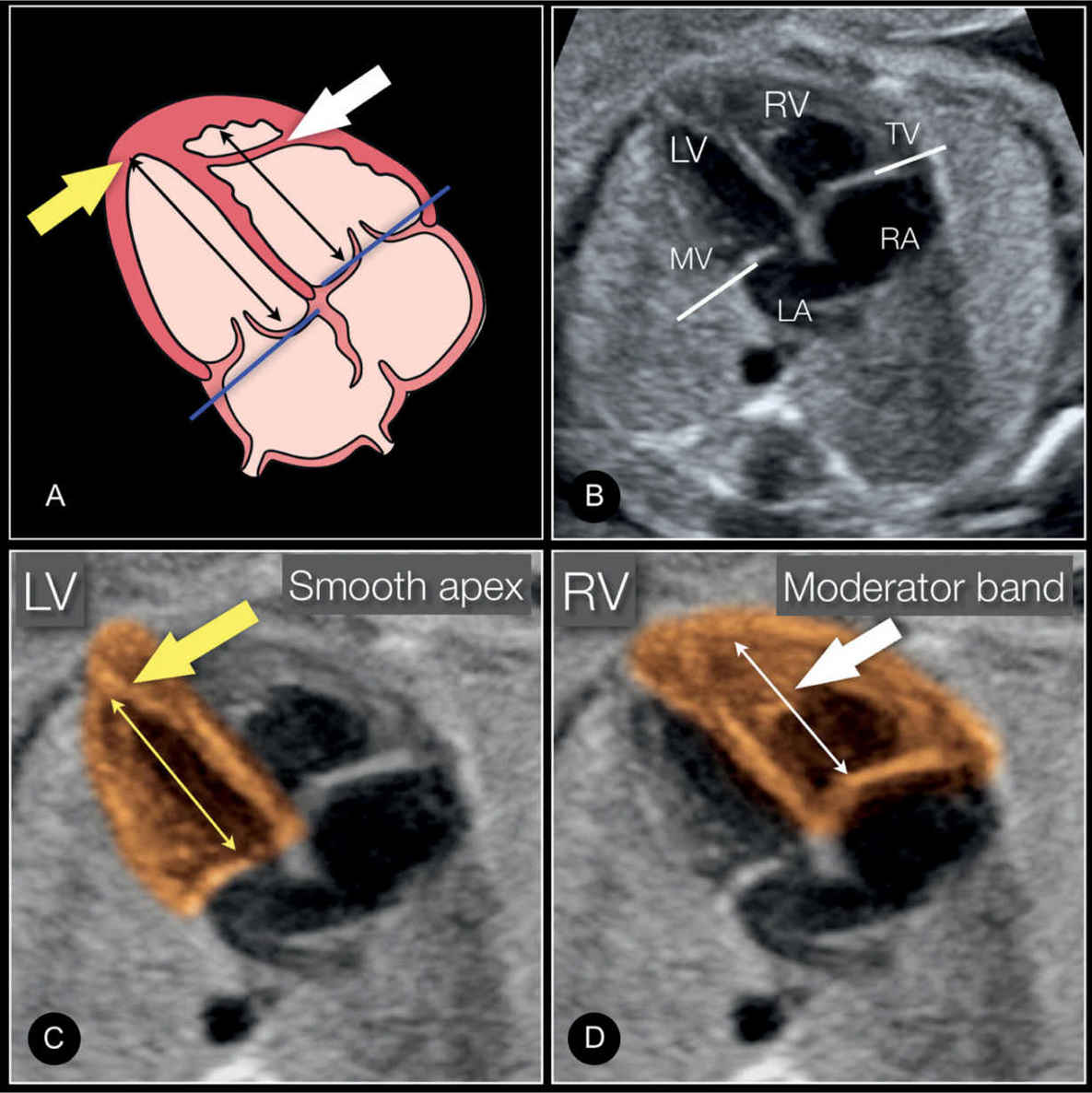
Figure 7.6: Schematic drawing (A) and apical four-chamber view (B) with a highlight of the left ventricle (LV) (C) and right ventricle (RV) (D) in a normal fetus, showing the differentiating features of the LV and RV. The LV is longer than the RV (double-sided arrows), is smooth, and forms the apex of the heart (yellow arrow). The RV is coarse and has the typical moderator band (white arrow) in its apex. The tricuspid valve (TV) is shown to insert more apically on the septum than the mitral valve (MV). See text for more details.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


