Burns
Robert L. Sheridan
Ronald G. Tompkins
Shriners Hospital for Children, Boston, Massachusetts 02114.
Department of Surgery, Harvard Medical School, Shriners Hospital for Children, Boston, Massachusetts 02114.
Burn care has undergone major technical and organizational changes since the mid-1980s, and outcomes have correspondingly improved (1). This chapter reviews the clinical management of the seriously burned child and relates progress in the field to growing understanding of the pathophysiology of burn injury.
EPIDEMIOLOGY AND NATURAL HISTORY
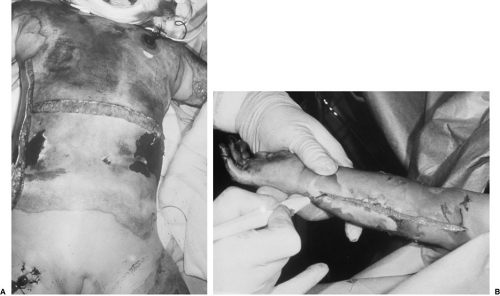
In the developed world, approximately 75% of pediatric burn patients are injured by hot liquid, typically in bathing or cooking accidents. The remaining 25% have suffered flame, contact, chemical, electric, or tar injuries (2). Although the life-threatening nature of large injuries is often emphasized, the potentially devastating impact of poorly managed smaller burns should not be neglected (Fig. 31-1).
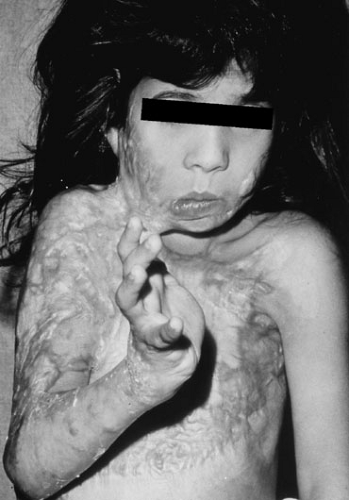 FIGURE 31-1. Suboptimal management of small burns can have major adverse functional and cosmetic implications. |
Extensive efforts have been made to diminish the incidence of pediatric burn injury through public education, with mixed effect. Legislation that requires lower temperatures for hot water heaters has been more successful (3). Such successes, although only locally effective, have been associated with a decreased incidence of hot water injuries in children. Approximately 15% of pediatric burn injuries are attributed to abuse or neglect, and an awareness of this important issue facilitates the prevention of repeated injuries (4).
Our survival depends on the vapor and bacterial barriers provided by normal skin. The epidermal layer provides these two essential functions, whereas the dermis provides the flexibility and strength of the skin. In addition, dermal appendages prevent desiccation of the skin by producing oils, and the reactive dermal microvasculature is responsible for heat dissipation and conservation, allowing us to adapt to changes in environmental temperature. The unique epidermal-dermal bond is also essential, as demonstrated by morbidity and mortality that occurs when it is deranged, such as in toxic epidermolysis or epidermolysis bullosa (5,6).
An understanding of the natural history of any disease process facilitates an understanding of the success of intervention. A burn wound is initially clean, but is rapidly colonized by endogenous bacteria. As bacteria multiply in the avascular eschar over the succeeding days, proteases liquefy the eschar, which then separates, leaving a bed of granulation tissue or healing burn, depending on the depth of the original injury. If wounds are small— less than 20% of the total body surface— this local infectious challenge is usually tolerated by the child. However, when injuries are larger, systemic infection results, explaining the rare survival of patients with burns in excess of 40% of the body surface in whom this natural history is permitted to unfold.
Children with burns in excess of 20% of the body surface frequently respond to this physiologic challenge with an initial decrease in cardiac output and metabolic rate (7). Effected by a complex cascade of mediators whose interactions are incompletely understood, a hypermetabolic response follows a few hours later, with a near doubling of cardiac output and resting energy expenditure over the subsequent 24 to 48 hours in those who are successfully resuscitated (8). The magnitude of this response peaks in those with injuries of 60% or more of the body surface at as high as twice the normal basal metabolic rate. The associated increase in substrate requirements has major implications for the support of burn patients. The etiology of the hypermetabolic response is not entirely understood, but probably involves a combination of factors, including a change in hypothalamic function with coincident rises in glucagon, cortisol, and catecholamines; deficient gastrointestinal barrier function with translocation of bacteria and their by-products; bacterial contamination of the burn wound with systemic release of similar products from this source; and some element of enhanced heat loss
by transeschar evaporation of fluid. The hypermetabolic response probably has survival value because it is conserved so broadly over numerous species.
by transeschar evaporation of fluid. The hypermetabolic response probably has survival value because it is conserved so broadly over numerous species.
An important element of successful management of children who have sustained large injuries is support of the hypermetabolic response through the provision of adequate quantity and quality of substrate. Modification of the response is of unknown value, but is being explored in the form of beta-blockade (9), insulin-like growth factor-1 (10), growth hormone (11), anabolic steroids (12), and other agents (13). This is a fast-moving and exciting area of investigation likely to have significant impact on burn care over coming decades, as the basic biology is unraveled.
MANAGEMENT PHILOSOPHY
Highlights of the initial approach to serious burns in children include (1) an individualized resuscitation of virtually all children regardless of injury severity, (2) early excision and biologic closure of deep wounds, (3) continuous rehabilitation, (4) judicious use of broad-spectrum antibiotics with early detection and specific treatment of septic foci, (5) intensive patient and family psychosocial support, and (6) comprehensive long-term follow-up with coordinated rehabilitation and reconstructive surgery. The acute hospitalization is organized into four phases: (1) initial evaluation and resuscitation, (2) initial wound excision and biologic closure, (3) definitive wound closure, and (4) graded increase in a continuous rehabilitation effort. With this approach, survival with good quality of life can be expected for burn-injured children without anoxic brain injury, almost regardless of injury size (14).
INITIAL EVALUATION
An organized approach to serious injuries facilitates achieving the optimal outcome and begins with a systematic initial evaluation, which includes a primary survey, effective airway control, and vascular access, followed by a systematic secondary survey (1). Because many burned children have sustained concurrent injuries, the initial evaluation should be approached as in any multiple-trauma patient (15). After evaluating and securing the airway while maintaining control of the cervical spine, breathing mechanics are assessed, a rough estimate is made of the circulating volume, the level of consciousness is documented, and the child is completely undressed. This should be performed in a warm environment to avoid hypothermia.
Secure airway and vascular access are crucial and should be obtained early in the evaluation. A badly burned face makes tape ineffective to secure the endotracheal tube, and umbilical tape ties should be used. In seriously burned patients, secure venous access is best obtained centrally, although two peripheral intravenous lines are a reasonable option. For venous access in the less severely burned child, peripheral intravenous access is appropriate. Venous access should be obtained through nonburned areas, if possible. In the hypovolemic child, intraosseous resuscitation can be lifesaving, although it should be replaced promptly with venous cannulae as soon as practical. All patients should have a nasogastric tube in place, particularly if transported by air, because the child with a gas-filled stomach may vomit and aspirate (Fig. 31-2). A bladder catheter facilitates a smooth fluid resuscitation. Continuous temperature monitoring with rectal, esophageal, or bladder probes and arterial access are helpful in selected patients.
 FIGURE 31-2. Nasogastric tube function, as well as physical presence, must be regularly verified to minimize the possibility of gastric distention and subsequent aspiration during burn resuscitation. |
The burn-specific secondary survey (Table 31-1) includes a complete history, vital signs, a detailed physical examination, and laboratory and radiographic studies appropriate for the mechanism of injury. The history, particularly details regarding the mechanism of injury, is important and is ideally obtained from witnesses, rescue personnel, and family members. The mechanism of injury often determines the need for special studies, such as computed tomograms of the head and abdomen, or radiographs of the cervical spine. Other important historical
points include past medical and surgical history, time of the last meal, tetanus status, medications and allergies, tap water temperature in hot liquid injuries, and extrication time in closed-space injuries. Vital signs are determined during the secondary survey, and age-specific norms should be known (Table 31-2). It is important to document and maintain a normal body temperature because burned children are especially prone to hypothermia. A complete physical examination should proceed in an organized fashion, not allowing the presence of the burn to distract the examiner from performing a complete assessment.
points include past medical and surgical history, time of the last meal, tetanus status, medications and allergies, tap water temperature in hot liquid injuries, and extrication time in closed-space injuries. Vital signs are determined during the secondary survey, and age-specific norms should be known (Table 31-2). It is important to document and maintain a normal body temperature because burned children are especially prone to hypothermia. A complete physical examination should proceed in an organized fashion, not allowing the presence of the burn to distract the examiner from performing a complete assessment.
TABLE 31-1 Important Aspects of the Burn-specific Secondary Survey. | ||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 31-2 Age-specific Resuscitation End Points. | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
The patient’s neurologic status should be carefully documented early during the evaluation because many patients become progressively obtunded secondary to the administration of analgesics and sedatives as well as intravascular volume depletion. If injury mechanism is consistent with a head injury, computed tomography (CT) should be performed.
Trauma to the head, face, and neck is determined by inspection and palpation. The corneal epithelium and globes should be examined before the development of adnexal edema, which renders the examination more difficult. Major corneal epithelial burns are obvious by the opaque corneal appearance that results. More subtle defects are apparent after staining with topical fluorescein. Upper airway injuries are suspected in the presence of a hoarse voice, burns of the lips or tongue, singed facial and nasal hair, or carbonaceous sputum. Hot liquid aspiration may complicate facial scald burns in small children and should be suspected if there is blistering in or around the mouth. If upper airway compromise is imminent, a clinical judgment based on the suggestion of significant upper airway edema, then endotracheal intubation is mandatory. This is particularly important before committing the child to a long transport. Verification of endotracheal tube security is an important part of the head and neck examination.
The torso should be assessed for compliance, and if ventilation is restricted by overlying circumferential eschar, torso escharotomies should be performed promptly with coagulating electrocautery to minimize blood loss. Incisions are typically made axially along the flanks and are connected by one or more horizontal incisions (Fig. 31-3A). The abdomen should be assessed for tenderness or distention. If the mechanism of injury suggests an abdominal injury, CT or peritoneal lavage is appropriate, particularly in the presence of an inappropriate resuscitative volume requirement. Gastric distention is common in distressed children, and nasogastric decompression is routinely recommended during the initial evaluation and transport. Proper nasogastric tube function should be verified regularly. All burned children should receive immediate ulcer prophylaxis with intraluminal antacids and intravenous histamine receptor blockers because the incidence of stress ulceration is unacceptably high if this precaution is not taken. The presence of genital burns should be noted. If the patient is not circumcised, the foreskin should be reduced after placement of the bladder catheter to avoid paraphimosis secondary to progressive edema.
Regular assessment and documentation of peripheral perfusion is crucial during the first postinjury days (16). Blood flow can be compromised by constricting circumferential eschar as subeschar tissues become progressively edematous, or by progressive intracompartmental edema in patients with electric or deep thermal burns. Both are detected by the development of a progressive increase in the extremity’s firmness and a decrease in its distal temperature. Pulsatile Doppler signals in the lower-pressure distal vasculature, such as the palmar arch and digital vessels, should be documented hourly. The loss of pulsatile Doppler signals is consistent with increasing tissue pressure if intravascular volume is adequate. Constricting circumferential eschar can be divided at the bedside with the coagulating electrocautery using medial and lateral axial incisions (see Fig. 31-3B). If the burn is full thickness, it is insensate and no sedation is required. If the burn is partial thickness in depth, light sedation is used. It is important to maintain hemostasis during the procedure and to verify that the procedure has enhanced distal blood flow. Hand escharotomies are often not required once the more proximal upper extremity has been adequately decompressed.
If decompression of the arm to the level of the metacarpophalangeal joints has not resulted in adequate digital blood flow, axial digital incisions are made between the extensors and the neurovascular bundles. Ideally, a single incision on the radial aspect of the thumb and the ulnar aspect of the digits suffices. The incisions on the central digits of the hand can be extended proximally between the metacarpals.
If decompression of the arm to the level of the metacarpophalangeal joints has not resulted in adequate digital blood flow, axial digital incisions are made between the extensors and the neurovascular bundles. Ideally, a single incision on the radial aspect of the thumb and the ulnar aspect of the digits suffices. The incisions on the central digits of the hand can be extended proximally between the metacarpals.
Weakness of intracompartmental muscle groups or pain with their passive stretch supports the suspicion of elevated intracompartmental pressures, although such signs can be obscured in many burn patients (17). The diagnosis of an evolving compartment syndrome in the acutely burned child can be an exceptionally difficult one to make early, and the clinician should decompress such extremities based on clinical suspicion. Compartment pressure measurements can be a useful adjunct in equivocal situations, but clinical judgment should suffice in most cases. If missed, compartment syndromes lead to intracompartmental sepsis or functional deficits later in the patient’s course.
Evaluation of the child’s wound is deferred until higher-priority evaluations are complete. Important to the initial evaluation are an assessment of the wound depth, size, and circumferential components. Early burn depth estimates are accurate in very deep or very superficial wounds. However, many burns (particularly scald injuries in children) are of indeterminate depth on initial examination. Significant effort has been applied to develop technical aids that accurately gauge burn depth during the initial evaluation (18), with little clinical success. Fortunately, an accurate determination of depth is not necessary to proceed with initial wound management or fluid resuscitation. In contrast, an accurate assessment of burn size can be made early and is important to initial management because resuscitative fluid administration is primarily determined by overall burn size. Burn size in children is best estimated with an age-specific chart (Fig. 31-4) because the child’s body proportions change with growth. The major anthropometric change involves the head and legs. The infant head represents 18% of the total body surface and the legs 14%. In older adolescents and adults, the head represents 9% of the body surface and the legs 18%. It is important to identify circumferential components of the wound because these areas need to be closely monitored for compromise of peripheral perfusion in extremity or neck burns and compromise of ventilation in torso injuries.
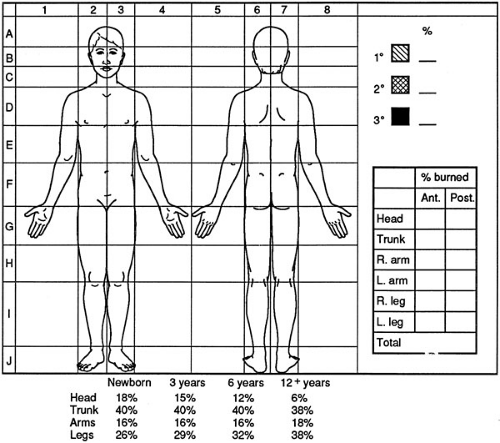 FIGURE 31-4. An age-specific chart facilitates accurate estimation of burn size over a broad range of ages. |
Limited laboratory studies are of value during the initial evaluation. Patients with a history of exposure to noxious fumes should have the arterial PaO2, PaCO2, pH, and carboxyhemoglobin percentage determined. However,
because the half-life of carboxyhemoglobin is 30 to 45 minutes when patients are ventilated with high concentrations of oxygen, a normal carboxyhemoglobin of less than 5% does not preclude significant exposures when patients have been well ventilated with high concentrations of oxygen during transport. Patients with electric or very deep thermal injuries may require blood products during the initial resuscitation, and in such patients, a blood bank specimen should be sent. Routine hematology and chemistry profiles are of limited usefulness initially, but do establish a baseline. Urinalysis for occult blood is helpful in patients with electric or very deep thermal burns if gross pigmenturia has been cleared with crystalloid administration. Radiographs useful during the initial evaluation are determined by the mechanism of injury and the need to evaluate placement of vascular access devices.
because the half-life of carboxyhemoglobin is 30 to 45 minutes when patients are ventilated with high concentrations of oxygen, a normal carboxyhemoglobin of less than 5% does not preclude significant exposures when patients have been well ventilated with high concentrations of oxygen during transport. Patients with electric or very deep thermal injuries may require blood products during the initial resuscitation, and in such patients, a blood bank specimen should be sent. Routine hematology and chemistry profiles are of limited usefulness initially, but do establish a baseline. Urinalysis for occult blood is helpful in patients with electric or very deep thermal burns if gross pigmenturia has been cleared with crystalloid administration. Radiographs useful during the initial evaluation are determined by the mechanism of injury and the need to evaluate placement of vascular access devices.
The initial evaluation of patients with electric, chemical, or tar injuries is the same as in those patients with thermal injuries; however, a few additional points require emphasis. Also, children with toxic epidermal necrolysis, purpura fulminans, or major soft tissue injuries are well managed in burn units (19).
Electric
Patients exposed to high voltage (greater than 1,000 V) present a combination of deep tissue injury secondary to the passage of current, locally destructive entrance and exit wounds, deep wounds where current arcs across flexed joints, flame burns secondary to clothing ignition, flash burns, axial spine fractures secondary to tetanic contraction of paravertebral muscles, and other injuries related to the fall or blast that so commonly accompanies high-voltage injury (20,21,22). Such patients require a complete trauma evaluation, cardiac monitoring, a bladder catheter to evaluate the urine for pigment, serial monitoring of compartments at risk for pressure elevation, and spine immobilization pending radiographic clearance of the axial spine.
Compartment pressure elevation, secondary to edema of injured muscle, can result in additional ischemic injury if compartments are not promptly released (23).
Chemical
Patients suffering chemical burns are first managed by at least 30 minutes of copious tap water irrigation (24).
Ocular injuries are irrigated with saline. Topical ophthalmic anesthetics facilitate relief of the blepharospasm that often interferes with effective irrigation of the globe. Life-threatening hypocalcemia can develop in patients exposed to concentrated hydrofluoric acid. This should be anticipated and managed with subeschar injection of 10% calcium gluconate with monitoring and support of the serum ionized calcium before urgent excision of selected extensive wounds (25). The more common limited exposures to dilute hydrofluoric acid are managed with irrigation and topical calcium gluconate gel.
Ocular injuries are irrigated with saline. Topical ophthalmic anesthetics facilitate relief of the blepharospasm that often interferes with effective irrigation of the globe. Life-threatening hypocalcemia can develop in patients exposed to concentrated hydrofluoric acid. This should be anticipated and managed with subeschar injection of 10% calcium gluconate with monitoring and support of the serum ionized calcium before urgent excision of selected extensive wounds (25). The more common limited exposures to dilute hydrofluoric acid are managed with irrigation and topical calcium gluconate gel.
Tar
Tar is often heated to more than 400°F and commonly causes a deep burn. Tar is initially cooled by tap water irrigation to limit the progression of the injury and is later removed with a lipophilic solvent. After initial irrigation, chemical and tar burns are managed surgically as indicated by depth, which is frequently underestimated on initial examination.
Abuse
All burned children should be evaluated for abuse or neglect. It is an ethical and legal mandate that suspect injuries be filed with the appropriate state agency (26). Important historical points include tap water temperature, duration of contact, caregivers involved, conflicting reports from involved caregivers, delay in seeking treatment, and prior injuries. Important points of examination (Fig. 31-5) include uniformity of burn depth, absence of splash marks, sharply defined wound margins, porcelain contact sparing, flexor sparing, stocking or glove patterns, dorsal location of contact burns of the hand, and localized very deep contact burns (27). All such children should be admitted to the hospital regardless of burn size. Suspect cases should be referred to the appropriate state authorities. Radiographic screening of the head and long bones should be considered.
FLUID RESUSCITATION
There are many formulas for burn resuscitation, but no formula accurately predicts fluid requirements in every child. No formula can replace a bedside presence repeatedly evaluating the child’s physiology throughout resuscitation. The Modified Brooke formula (Table 31-3) is commonly used as a starting point and serves as the basis for this discussion. However, regardless of the formula chosen to
initiate resuscitation, subsequent fluid administration is best guided by regular reassessment of resuscitation end points, rather than the prediction of any formula.
initiate resuscitation, subsequent fluid administration is best guided by regular reassessment of resuscitation end points, rather than the prediction of any formula.
TABLE 31-3 Modified Brooke Formula.a | |||
|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree