Arterial Disease
Philip C. Guzzetta Jr.
George Washington University School of Medicine, Children’s National Medical Center, Washington, District of Columbia 20010.
VASCULAR EMBRYOLOGY
The origin of the arterial vascular system has been extensively studied for more than a century. There is general agreement that the vessels are mesodermal derivatives that begin as cords of angioblast cells. These cords orient themselves into tubes and eventually develop along a capillary net formed by existing vessels that appear to have preferred paths of development. The development of paired aortic arches early in gestation reflects the human evolution from aquatic vertebrates, which use the aortic arches for blood flow through gills developed from the branchial clefts adjacent to the paired aortic arches. In humans, at the end of the first month of gestation, the six pairs of aortic arches have been formed.
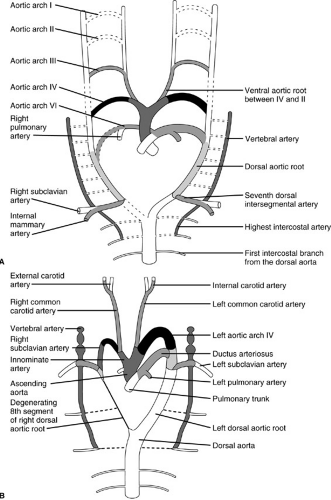
By gestational week 7, there is a single aorta posteriorly. Many of the paired aortic arches regress, and some persist as head and neck arterial branches. The left aortic arch IV develops into the aortic arch, and the left aortic arch VI becomes the ductus arteriosus. Aortic arch V is not shown and may not even exist in humans (Fig. 102-1). The location of the aortic arches during this stage of development is actually within the neck region, and the descent of the arch into the thorax occurs later with the development of the heart. Detailed discussion of cardiac development and its relation to various anomalies can be found in Embryology for Surgeons by Skandalakis and Gray (1).
TECHNIQUES TO DIAGNOSE ARTERIAL DISEASE IN CHILDREN
Any new technique for imaging the arterial system in children must be compared with transarterial angiography for safety, quality of image, need for sedation or general anesthesia, and cost.
Ultrasound
Real-time ultrasound, particularly when combined with color Doppler ultrasound, has the attractive features of being a safe, noninvasive, and inexpensive technique to image vessels. The images may not be attainable, however, if there is overlying bone or intestine that contains a great deal of gas, which seriously limits its use for the chest and abdomen. In addition, simultaneous viewing of vessels within a large area in different planes, such as the entire abdominal aorta and its branches, is not possible with ultrasound, which limits its use as a guide for the correction of problems in these vessels. For evaluation of a single vessel, such as the renal artery after repair, Doppler ultrasound has a definite role to ensure patency and flow, but has little place in the initial evaluation of children with suspected arterial disease. The echocardiogram and transesophageal echocardiogram (TEE) are used extensively to assess the ascending aorta, pulmonary arteries, pulmonary veins, inferior and superior vena cavae, and the heart.
Magnetic Resonance Imaging
The technology of magnetic resonance imaging (MRI) is developing rapidly, and many of its limitations for arterial evaluations may soon be overcome. MRI can be effective in assessing venous structures and is the technique of choice in assessing the patency of the large veins in children who have previously had multiple central venous catheters. The anatomy of vascular anomalies, such as double aortic arch or aberrant subclavian artery, can be visualized easily by MR angiography (MRA). For small visceral vessels, such as the renal artery, MRA does not allow adequate detail and should not be depended on solely in making operative decisions. As MRA progresses, it may replace transarterial angiography for diagnosing many diseases. MRI has
a role in the assessment of vascular anomalies of the extremities, for which it shows the relation of the vessels and the soft tissue. Motion artifact is a serious problem with MRI, and many children require heavy sedation or general anesthesia for the study.
a role in the assessment of vascular anomalies of the extremities, for which it shows the relation of the vessels and the soft tissue. Motion artifact is a serious problem with MRI, and many children require heavy sedation or general anesthesia for the study.
Transarterial Angiography
Transarterial angiography remains the gold standard for imaging the arteries of children. The ability to view whole segments of the arterial system at once, magnify the area of interest, and obtain excellent detail of the vascular lumen make this the modality of choice for assessing pediatric arterial disease. Improvements in interventional radiographic treatment of arterial diseases allow the transarterial approach to be therapeutic as well as diagnostic in some cases. Major risks of this approach include damage to the artery used to access the arterial system, potential allergic reactions to the contrast, radiation exposure, and the need for sedation. As the technology improves, MRA
may be most useful for screening patients for arterial disease, with the transarterial angiography used to confirm the problem in selected patients, especially those who can be treated by interventional radiographic techniques.
may be most useful for screening patients for arterial disease, with the transarterial angiography used to confirm the problem in selected patients, especially those who can be treated by interventional radiographic techniques.
ARTERIAL ANEURYSMS
Congenital Aneurysms
Arterial aneurysms have been diagnosed by prenatal ultrasound and have even been implicated in fetal death. Congenital aneurysms are almost always found in the abdominal aorta, contain all three layers of the involved artery, and show no sign of arteritis. They usually present in children younger than 5 years of age as painless abdominal masses without evidence of distal vascular disease or embolus. The form of the aneurysm may be saccular or fusiform. Treatment is resection of the aneurysm and reconstruction with autogenous tissue, if possible. Because many of these aneurysms involve the abdominal aorta, prosthetic graft replacement has been the most common technique, with expected growth of the normal vessel on either side of the graft to accommodate the longitudinal growth of the child (2).
Acquired Aneurysms
Acquired aneurysms can be separated into those due to an arteritis, syndromes causing medial degeneration, direct arterial infection, trauma (false aneurysms), and arterial dysplasia.
Aneurysms Due to an Arteritis
Arterial aneurysms may develop in children as the result of Kawasaki disease, giant cell arteritis, Takayasu disease, or polyarteritis nodosa. Kawasaki disease (also known as mucocutaneous lymph node syndrome) is a disease with a median age of onset of 3 years and is characterized by high fever, cervical adenopathy, conjunctivitis, stomatitis, and generalized erythema, which is frequently most intense on the soles and palms. Coronary artery aneurysms develop in up to 15% of children who are not treated with aspirin or IV γ-globulin. Rarely, aneurysms develop in locations other than the coronary arteries with Kawasaki disease. The coronary artery aneurysms frequently improve with medication, seldom rupture, and may require surgical resection only when they are giant aneurysms, defined as greater than 8 mm in diameter. Persistent giant aneurysms tend to cause stenosis or thrombosis of the involved coronary, leading to myocardial ischemia distal to the aneurysm, which requires surgical bypass of the diseased artery.
Giant cell arteritis most commonly involves the aorta, but it may also cause peripheral artery aneurysm formation. Takayasu arteritis and polyarteritis nodosa most often cause stenosis rather than aneurysm formation, although aneurysms may develop in the aorta or its main branches. When polyarteritis nodosa causes aneurysms of the small and medium-size renal arteries, renal impairment and hypertension commonly occur (3). Operative correction of an aneurysm due to an arteritis has a high complication rate. Unless the aneurysm is large or threatens to rupture, initial treatment of these patients should be with glucocorticoid therapy rather than surgery.
Aneurysms Due to Syndromes Causing Medial Degeneration
Type IV Ehlers-Danlos syndrome, characterized by an abnormal or absent type III collagen, is associated with medial degeneration of the large arteries with associated aneurysm formation or rupture. The aorta is the most common site of aneurysm formation, but any artery with substantial amounts of collagen is at risk for this problem (4). Marfan syndrome is an autosomal dominant disease characterized by cystic medial degeneration of the ascending aorta; thin, elongated extremities; chest wall deformities; and dislocation of the lens. The enlarging ascending aorta places the Marfan syndrome patient at significant risk for aneurysmal dissection and rupture or severe aortic valvular insufficiency due to dilation of the aortic root.
Other conditions that deposit abnormal substances into the media of the aorta, such as tuberous sclerosis, cystinosis, or mucopolysaccharide deposition (5) may predispose the aorta to aneurysm formation and rupture. Treatment of these children can be complicated by poor tissue integrity at the suture line when a prosthetic graft is placed, leading to false aneurysm formation. Children with some types of Ehlers-Danlos syndrome have abnormal bleeding times, making major surgical procedures hazardous. Nonetheless, the best chance for survival for a patient with one of these syndromes and an aneurysm is resection of the aneurysm and prosthetic graft placement.
Aneurysms Due to Direct Arterial Infection
Most aneurysms that are reported in children are caused by bacterial or fungal infection of a structurally normal arterial wall. An arterial wall, particularly that of the aorta, is generally resistant to bacterial seeding unless there is trauma to the intima or an abnormal flow pattern that potentially weakens the wall. Patients at greatest risk for aneurysm formation due to direct arterial infection are older children with thoracic aortic coarctation and infants with umbilical artery catheters in place.
Children with this type of aneurysm are usually very ill, with signs of bacteremia similar to those seen in patients with acute endocarditis. The most common organism causing this type of aneurysm is Staphylococcus aureus, although fungi and other bacteria have also been cultured
from infected aneurysms. Histologic examination of the aneurysm reveals inflammation of the arterial wall, with media disruption and aneurysm formation. These aneurysms must be resected because they are at high risk for rupture. Although arterial replacement with autogenous tissue would be ideal, most aortic reconstructions must be done with prosthetic grafts, accepting the potential of graft infection in the future. If the child is large enough to consider extraanatomic bypass of the aorta at the time of aneurysm resection, it should be recommended instead of suturing prosthetic material into a grossly infected area.
from infected aneurysms. Histologic examination of the aneurysm reveals inflammation of the arterial wall, with media disruption and aneurysm formation. These aneurysms must be resected because they are at high risk for rupture. Although arterial replacement with autogenous tissue would be ideal, most aortic reconstructions must be done with prosthetic grafts, accepting the potential of graft infection in the future. If the child is large enough to consider extraanatomic bypass of the aorta at the time of aneurysm resection, it should be recommended instead of suturing prosthetic material into a grossly infected area.
Aneurysms Due to Trauma (False Aneurysms)
Although they are probably the most common aneurysms in children, the true incidence of aneurysms due to trauma is unknown. These aneurysms are reported infrequently because they are often seen in the distal extremities and are easily cared for by vessel ligation. Most of these aneurysms are caused by penetrating trauma, particularly lacerations of the hands or feet (Fig. 102-2). The trend of nonoperative treatment of “minimal” vascular injuries with normal distal pulses (6) will likely increase the appearance of these in the future. Optimal treatment is aneurysm resection with ligation or repair of the artery, depending on the artery involved.
Aneurysms Due to Arterial Dysplasia
In children, aneurysms due to arterial dysplasia are found almost exclusively in the renal arteries, associated with renal artery stenosis and renovascular hypertension. Recognition of the aneurysm is usually made when the patient has an angiogram for hypertension. The aneurysms commonly occur at branch points of the renal artery (Fig. 102-3) and should be distinguished from the poststenotic dilation that is frequently seen in the main renal artery. Treatment of the aneurysm may include resection and suturing of the distal end of the bypass graft to the aneurysm site if the aneurysm is near the main renal artery. No treatment is employed if the aneurysm is small and peripheral. An excellent classification of aneurysms in children was developed by Sarkar and colleagues (7) (Table 102-1).
ARTERIAL OCCLUSIVE DISEASE DUE TO ARTERIOPATHY
Takayasu Arteritis
Takayasu arteritis is an inflammatory condition of unknown cause. It usually involves the aorta and its major branches and can lead to stenosis or occlusion of the involved vessels. The condition is most commonly seen in
adolescent girls, but can affect boys or girls at any age. The sites of involvement are usually the aortic arch vessels or the midabdominal aorta and its branches. Diffuse major arterial occlusion can develop, which has led to the name pulseless disease. The pulmonary artery is involved in more than one-half of patients. The diagnosis of Takayasu disease and follow-up of the disease’s response to treatment may be done effectively with MRA (8).
adolescent girls, but can affect boys or girls at any age. The sites of involvement are usually the aortic arch vessels or the midabdominal aorta and its branches. Diffuse major arterial occlusion can develop, which has led to the name pulseless disease. The pulmonary artery is involved in more than one-half of patients. The diagnosis of Takayasu disease and follow-up of the disease’s response to treatment may be done effectively with MRA (8).
 FIGURE 102-3. Aneurysm of a branch of the left renal artery associated with high-grade stenosis of the main renal artery. |
TABLE 102-1 Classification of Aneurysms in Children.a | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree