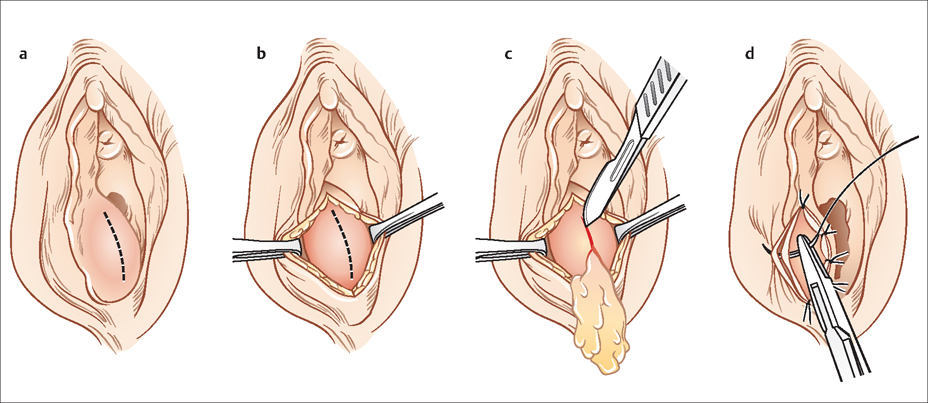
47 Vulvar and Vaginal Lesions Robert L. Barbieri Common, palpable, nonpigmented lesions of the vulvavagina include Bartholin Cyst, condylomata acuminata, skin tags (achrochordons), and vaginal wall cysts. The Bartholin glands are located at the 4-o’clock and 8-o’clock positions at the vulvovaginal junction. Normal Bartholin glands are about 0.5 cm in diameter with a duct that is about 2 cm in length. They secrete fluid and provide moisture to the vagina. When the Bartholin duct is blocked fluid may accumulate in the cyst causing a large swelling of the labia. If the fluid in the blocked gland becomes infected the cyst becomes an abscess and can be exceedingly painful and erythematosus. About 10% of Bartholin abscesses are associated with Neisseria gonorrhoea or Chlamydia trachomatis infections. The lifetime risk of developing a Bartholin cyst is about 1%. Asymptomatic Bartholin cysts do not need therapy. If a Bartholin cyst produces symptoms such as vulvar discomfort it may be treated by marsupialization (Fig. 47.1) or by placement of a balloon catheter into the cyst (Word catheter). The balloon catheter simultaneously drains the cyst and helps to create a new duct to prevent recurrence of the cyst. If an abscess is present, a typical antibiotic regimen includes ceftriaxone 250 mg intramuscular injection in a single dose (to cover for Escherichia coli and N. gonorrhoea) plus metronidazole 500 mg orally twice daily for 7 days. If C. trachomatis is present, azithromycin 1 g orally as a single dose is recommended. Very rarely the Bartholin gland may be the site of origin for an adenocarcinoma or squamous cell carcinoma. Bartholin cysts and abscesses are typically fluid-filled. A solid tumor of the Bartholin glands should raise suspicion of a cancer. Women over the age of 40 years with a Bartholin cyst, abscess, or solid tumor should undergo resection of the gland to allow for definitive histological diagnosis to ensure that cancer is not present. Fig. 47.1 Surgical approach to the marsupialization of a Bartholin cyst Anogenital warts are caused by infection with human papilloma virus, most commonly subtypes HPV-6 and HPV-11. Endogenous immune surveillance helps to prevent condylomata from growing to a large size in immune competent women. Immunosuppressed women, such as those with HIV disease or organ transplant recipients, are at increased risk of developing large condylomata. For example, in a study of over 700 women, condylomata were present in 7% of women with HIV and 1% of women who were HIV-negative. When condylomata grow into large exophytic masses they can interfere with vaginal intercourse and vaginal delivery. Condylomata lata, a dermatological manifestation of secondary syphilis, are fatter than condylomata acuminata. A skin tag or achrochordons is a flesh-colored, pedunculated outgrowth of normal skin on a stalk or wide base. Skin tags usually occur in sites of friction such as the inguinal area, axilla, or neck. They are associated with insulin resistance, which occurs in obesity, polycystic ovary syndrome, and diabetes. Vaginal wall cysts, which are typically located in the lateral or posterior walls of the vagina, may be caused by embryonic remnants of the man or wolfan ducts (Gartner duct cyst) or from epidermal inclusion cysts. Endometriosis cysts occasionally involve the vaginal wall. Imaging studies such as magnetic resonance imaging may be helpful in identifying whether the cysts are simple fluid-filled structures or contain solid components. Imaging is also helpful in detecting additional small cysts that could not be detected by physical examination. Asymptomatic vaginal wall simple cysts do not need to be drained or excised. If symptoms are presents, such as pressure or pain symptoms, urinary incontinence, or pain with intercourse, the cysts can be excised or marsupialized, or drained. Anterior vaginal wall cysts near the introitus may be urethral diverticulum. Molluscum is caused by a poxvirus and results in raised, dome-shaped skin lesions with an umbilicated center. Crural folds are a common site for molluscum lesions along with the axilla, and antecubital and popliteal fossae. Molluscum is spread by skin-to-skin contact. Molluscum occurs commonly in children. Molluscum is uncommon in adults unless they are immunosuppressed due to HIV infection, chemotherapy, or chronic glucocorticoid treatment. Genital lesions should be treated to prevent spread by genital contact. Standard treatment involves removal of the lesions with cryotherapy, electrosurgery, or laser. Small studies have reported that topical application of cantharidin or concentrated potassium hydroxide may be successful in eradicating the lesions. Acanthosis nigricans (AN) is a velvety, mossy, verrucuous hyperpigmented skin change which usually presents in the nape of the neck, in the axillae, beneath the breasts, and on the inner thighs. The salient histological features are papillomatosis, hyperkeratosis, and hyperpigmentation. Achrochordons are often present in association with AN. The majority of cases of AN are caused by insulin resistance and friction in the intertrigonous areas. Occasionally, AN is a manifestation of an occult adenocarcinoma of the gastrointestinal tract or lung. In women, AN is often associated with polycystic ovary syndrome and diabetes, and it may be present in women with endometrial hyperplasia or endometrial cancer. Melanocytic nevi are a benign proliferation of a type of melanocyte, the nevus cell. Women with lightly pigmented skin and women with intense sun exposure are more likely to develop melanocytic nevi. Atypical nevi are benign proliferations of nevus cells that share some of the features of melanoma. Women with multiple atypical nevi are at increased risk for melanoma. Melanoma is the sixth most common cancer in young women. Less than 1% of melanomas arise on the vulva or vagina. In contrast to common melanomas in sun-exposed areas that occur in young women, most vulvar melanomas occur in women of 50–70 years of age. However, melanoma is a cause of up 10% of malignant tumors involving the vulva. Vaginal melanoma is extremely rare. Common clinical features of melanoma may be recalled using the mnemonic A, B, C, D, E: Asymmetry, irregular Borders, Color variability, Diameter greater than 6 mm, and Enlargement or Evolution of the color, size, or borders of the lesion. If clinical examination raises the possibility of atypical nevi or melanoma, a skin biopsy is recommended. Lesions due to lichen sclerosus, lichen planus, and lichen simplex chronicus are discussed in Chapter 30. Skin abscesses are collections of pus within the dermis and deeper tissues. A furuncle (“boil”) is an abscess of a hair follicle that extends into the subcutaneous tissue underlying the dermis. A carbuncle is a coalescence of multiple abscesses of hair follicles with multiple sites of drainage. Up to 50% of cases of skin abscesses are caused by Staphylococcus aureus infection (either methicillin-sensitive or methicillin-resistant). For small furuncles, treatment with warm compresses may be effective. For larger abscesses, incision and drainage is a preferred approach.
Types of Lesion
Palpable Lesions
Bartholin Cyst and Abscess
Condylomata Acuminata
Skin Tag
Vaginal Wall Cysts
Molluscum Contagiosum
Pigmented lesions
Acanthosis Nigricans
Melanocytic Nevi
Atypical Nevi and Melanoma
White Plaques or Patches
Pustules and Vesicles
Skin Abscess
Hidradenitis Suppurativa
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


