Use of Pulse Oximetry
Ronnie S. Fuerst
Introduction
The pulse oximeter, an electronic monitor used to noninvasively measure arterial oxygen saturation, is standard equipment in the emergency department (ED) and other places, such as the operating room, the intensive care unit, and outpatient settings, where the information would be valuable for patient care. An understanding of its applicability, interpretation, and limitations is essential in the modern practice of emergency medicine.
The origin of this technology lies in the 1930s, when the first in vivo device to measure oxygen saturation by transillumination was developed. The 1970s heralded two important developments. The first was the discovery of arterial pulsations in the microvasculature, and the second was the use of light-emitting diodes (LEDs) as a light source and photodiodes as light detectors. These latter findings assisted greatly in overcoming the size and weight problems associated with previous devices. In the early 1980s, microprocessors were added for self-calibration and improved accuracy through the use of algorithms (1).
The pulse oximeter has distinct advantages over other measures of oxygenation. First, it is at most an uncomfortable attachment to an extremity but can measure both absolute SaO2 and trends in patients requiring monitoring for acute medical and traumatic illness in an emergency setting. Second, it can be a stand-alone monitor or be integrated into more complex monitoring of a patient’s vital functions. Its only disadvantage is that it is unable to to distinguish other molecules attached to the hemoglobin moiety, such as carboxyhemoglobin and methemoglobin. It may read a normal value in their presence. Improvements in microprocessor performance in the past 10 years have vastly improved the performance of pulse oximeters overall and, in particular, when there is patient movement, when oxygen saturation drops below 80%, in low-perfusion states, and when monitoring sites are vasoconstricted (2). Pulse oximeter readings under these conditions should still be viewed with a cautious eye and correlated with other clinical information.
Anatomy and Physiology
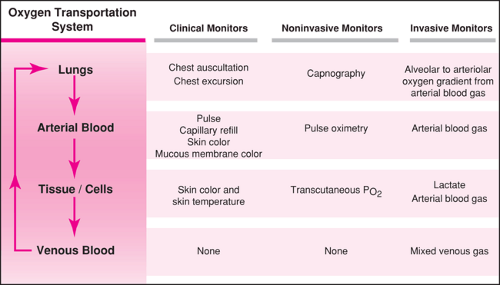
Pulse oximetry is a measure of the percent saturation of hemoglobin by the oxygen molecule. This is only one part of the oxygen transport system (Fig. 75.1), and other methods of observation and monitoring are required to evaluate other aspects of oxygen delivery (2). The remainder of this section presents a review of the physiology of hemoglobin saturation and the oxyhemoglobin dissociation curve, followed by a review of the mechanism of the equipment.
The hemoglobin molecule is almost entirely responsible for oxygen transport when oxygen is within the cardiovascular system. Only 1.5% of oxygen is dissolved in plasma. Hemoglobin saturation (SaO2) is the amount of oxygenated hemoglobin (O2Hb) compared with the total amount of hemoglobin
available for oxygenation, expressed as a percentage (3):
available for oxygenation, expressed as a percentage (3):
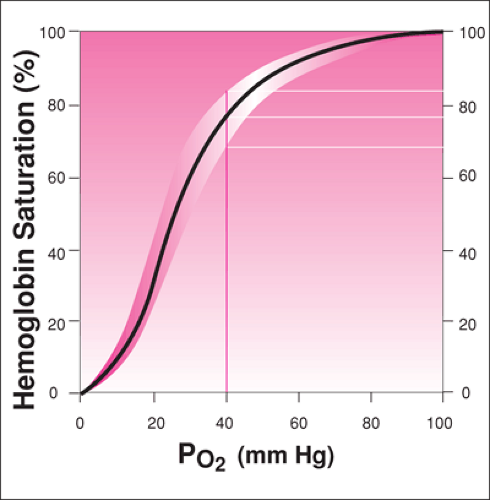
The oxyhemoglobin dissociation curve (Fig. 75.2) demonstrates the nonlinear relationship between hemoglobin saturation and the partial pressure of oxygen in plasma (PO2). Normal Sao2 is between 95% to 100%, and hypoxemia is defined as PO2 less than 70 mm Hg (SaO2 below 90%). Small changes in the SaO2 in the upper, flat part of the oxyhemoglobin dissociation curve result in larger changes in PO2. In the steep part (lower and middle part of the curve), large changes in the SaO2 result in small changes in PO2. Under normal physiologic conditions, the body operates at the upper portion of the curve, as depicted in Figure 75.2. Changes in the oxyhemoglobin dissociation curve either to the left or to the right change the relationship of SaO2 to PO2. The factors that shift the oxyhemoglobin curve to the left and increase the affinity of oxygen to hemoglobin at lower PO2 are increased pH, decreased temperature, decreased PCO2, and decreased 2,3-DPG. The 2,3-DPG levels are altered by a number of physiologic effects, and increases of 2,3-DPG are seen when anemia, chronic hypoxemia, high-altitude adaptation, chronic alkalosis, and hyperthyroidism are present.
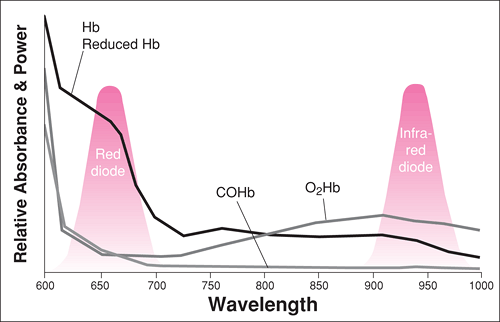
Pulse oximetry uses the principles of spectrophotometry and the Beer-Lambert law together with complex signal-processing algorithms and calibrations to calculate the percentage of oxyhemoglobin concentration. Four types of hemoglobin are clinically significant to pulse oximetry: oxygenated hemoglobin (O2Hb), reduced hemoglobin (Hb), carboxyhemoglobin (COHb), and methemoglobin (MetHb). For the purposes of pulse oximetry, both fetal hemoglobin and sickle hemoglobin are assumed to have the characteristics of adult hemoglobin. The oximeter emits two wavelengths of light—one in the red region (660 nm) and one in the infrared region (920 nm)—to differentiate the absorption of light by
the oxygenated and deoxygenated hemoglobin species in the microcirculation. Figure 75.3 shows the wavelength absorption of different hemoglobin moieties as they relate to this phenomenon.
the oxygenated and deoxygenated hemoglobin species in the microcirculation. Figure 75.3 shows the wavelength absorption of different hemoglobin moieties as they relate to this phenomenon.
Carboxyhemoglobin (COHb) behaves as O2Hb in regard to its absorption spectra, and so the oximeter misinterprets the CoHb and reads a falsely high SpO2. Methemoglobin (MetHb) absorbs light at both wavelengths emitted by the LED. Therefore, MetHb will always cause a falsely high SpO2, but as MetHb levels rise, the SpO2 level measured will be less because of the effects on both wavelengths where it causes interference. When the MetHb reaches 30%, the SpO2 will not be above 85% and will remain at that level regardless of increasing MetHb concentrations. Other dyshemoglobinemias may not reliably quantitate the actual oxyhemoglobin percentage. In patients suspected of MetHb or COHb, an arterial or venous blood gas should be sent with co-oximetry to assess their measured concentration in blood. The pulse oximeter also must measure absorption differences between the maximal and minimal arterial pulsations to enable it to separate the signals from arterial blood and exclude the background (i.e., venous blood and tissues). After obtaining the separate signals for bound and unbound hemoglobin, the formula above can be used to calculate the percentage saturation of hemoglobin in the circulation measured.
Pulse oximeters commonly used in the ED have been found to correlate with arterial blood gas oxygen saturation (SaO2) in patients with systolic blood pressures between 80 and 206 mm Hg, heart rates between 40 and 180 beats per minute, and hematocrits between 20% and 56% (4). The accuracy of pulse oximeters, as reported by manufacturers, is ±4% (with a 95% confidence interval) when the SpO2 is above 70%. There is much statistical variability when the SpO2 is below 70%. Thus, the trend of readings may be more accurate and useful than the individual SpO2 readout.
There are other important technical issues worthwhile to consider (5,6,7,8,9,10). Motion near the sensor site may mimic the pulsations of small arteries and affect the reading. In this instance, the pulse on the oximeter will not produce a normal curve and will not trace the patient’s actual heart rate. In low-flow states, the lack of blood flow in the vessels may not transmit sufficient change in light emittance for the monitor to read the saturation adequately. This may be demonstrated by the monitor indicating “pulse search.” During high venous pressure, the venous pulsation may transmit falsely low SpO2 to the monitor. In children, this rarely occurs in heart failure but may be present in traumatic venous obstruction or when a manometer cuff is inflated or a tourniquet is applied. Lastly, other ambient light sources, such as sunlight, warming lights, phototherapy, and bright fluorescent bulbs, may interfere with the reading by increasing the light to the photodetector. The patient ought to have the sensor shielded with a more light-resistant covering. Manufacturers have improved pulse oximeter performance by dealing with many of these confounding factors (2,11,12,13,14).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree