Ultrasound Evaluation of Potential Ectopic Pregnancy
Verena T. Valley
James R. Mateer
Introduction
More than one million ectopic pregnancies were estimated to have occurred among women in the United States from 1970 to 1989, with teenagers having the highest mortality rate (1). This hospital-based estimate may be falsely low due to the impact of medical advancement in diagnosis and treatment and a concurrent shift from inpatient treatment to multiple outpatient visits (2). Black adolescents and other minorities had the highest mortality rate for ectopic pregnancy—almost five times that for white teenagers (3). Furthermore, adolescent females and young women have the highest rate of Chlamydia trachomatis infection, which is a risk factor for subsequent ectopic pregnancy (4).
By definition, an ectopic pregnancy occurs when a fertilized ovum implants at a site other than the endometrial lining of the uterus. A heterotopic pregnancy is the combination of an ectopic pregnancy and an intrauterine pregnancy (IUP). This is believed to occur in only 1 in 30,000 pregnancies (5) but may have a higher incidence in patients taking fertility drugs or patients with extensive tubal disease. Studies have shown that over 40% of ectopic pregnancies may be initially missed (6,7). Improved methods of early diagnosis for ectopic pregnancy are needed to reduce the morbidity and mortality associated with this condition.
Ultrasound is a rapid and effective diagnostic tool for evaluating ectopic pregnancy. The main value of ultrasound is to determine the presence and viability of an IUP. By proving the presence of an IUP, diagnosis of an ectopic pregnancy is essentially excluded. The lack of an IUP on ultrasound, however, suggests the possibility of an ectopic pregnancy, especially if associated with an adnexal mass or significant free pelvic fluid.
Ultrasonography using a portable unit can usually be performed without difficulty in standard emergency department (ED) pelvic examination rooms. The number of examinations required for clinical competence has not been extensively studied. Reports in the primary care literature, however, suggest that a physician can be trained to perform a limited obstetrical ultrasound examination with a program that includes 40 to 75 training scans (8,9).
Anatomy and Physiology
Normal Pelvic Anatomy
Ultrasonographic characteristics of the postpubertal adolescent female are not significantly different from those of an adult female (10). For transabdominal scanning, the full bladder is used to displace bowel gas and serves as an acoustic window to the pelvis. The normal shape of the distended bladder is rectangular on transverse views and is teardrop-shaped on longitudinal views.
In the immediate premenarcheal period, the ovaries and the uterus enlarge rapidly and attain a mean volume by menarche that approaches adult size (11). The maximum uterine size for nulliparous adults is 7 cm in length and approximately 4 × 5 cm in anteroposterior and transverse dimensions. For multiparous patients, these dimensions are increased by 1 to 2 cm in all planes. With an empty bladder, the normal anteverted uterus lies at about 90 degrees to the plane of the vagina, whereas a fully distended bladder can position the uterus almost parallel to the vagina. The cervix is usually midline; however, the fundus is commonly tilted slightly to the right or left of midline. The endometrium is visualized within the uterus as a central bright echo, called the “endometrial stripe.” The
sonographic size and appearance of the endometrial stripe vary during the menstrual cycle, with a normal width of 2 to 4 mm in the proliferative phase and 5 to 6 mm in the secretory phase. In addition, the endometrial stripe becomes more echogenic during the secretory phase. When searching for an early IUP, the entire endometrial stripe must be visualized. Uterine anomalies, including bicornuate and septate uteruses, are occasionally seen. These often are first noted in early pregnancy when the gestational sac forms in one horn of the uterus.
sonographic size and appearance of the endometrial stripe vary during the menstrual cycle, with a normal width of 2 to 4 mm in the proliferative phase and 5 to 6 mm in the secretory phase. In addition, the endometrial stripe becomes more echogenic during the secretory phase. When searching for an early IUP, the entire endometrial stripe must be visualized. Uterine anomalies, including bicornuate and septate uteruses, are occasionally seen. These often are first noted in early pregnancy when the gestational sac forms in one horn of the uterus.
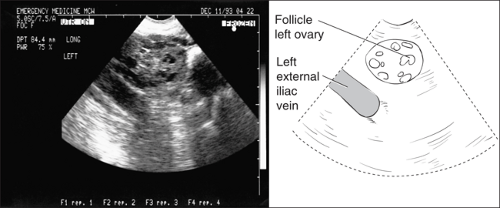 Figure 135.1 Longitudinal view of the left ovary demonstrating the characteristic follicular pattern. The ovary normally lies medial to the external iliac vein. |
The normal size of the ovary is 2 × 2 × 3 cm in young adults. Identification is facilitated when the characteristic multiple follicles (0.5 to 1.0 cm in diameter) are visualized around the periphery of the ovarian cortex (Fig. 135.1). When follicle size exceeds 2.5 cm, a physiologic cyst or other abnormality should be considered. The position of the ovaries is variable, but they are most commonly located near the posterior lateral pelvic wall, just anterior to the internal iliac vessels and medial to the external iliac vessels.
The vagina is a hypoechoic tubular structure caudad to the cervix and immediately posterior to the bladder on a transabdominal scan. This structure is recognized by a central echogenic stripe, which is formed by the opposing mucosal interface. The posterior fornix is closely related to the posterior cul-de-sac. The cul-de-sac is located posterior to the uterus and upper vagina. A small amount of fluid in the cul-de-sac is normal during midcycle.
Ultrasound Findings of Intrauterine Pregnancy
Recognizing an IUP is critical. The embryologic features of a normal IUP include (in chronological order of ultrasound appearance) the gestational sac, the yolk sac, the double decidual sac sign, the fetal pole, and fetal cardiac activity (Fig. 135.2 and Table 135.1).
In obstetrics, gestational age is traditionally defined based on the menstrual age—the time from the beginning of the last normal menses. Ultrasound imaging also follows this convention for references to gestational age. Gestational age can be determined by ultrasound as early as 5 weeks based on measurements of the internal diameter of the gestational sac. For more advanced early pregnancy (6 to 12 weeks’ gestation), a crown-rump length can be determined by measuring the maximal length of the embryo excluding extremities and the yolk sac. The crown-rump length of the embryo during the first trimester is the most accurate measurement of gestational age that can be obtained by ultrasound during a pregnancy.
Gestational Sac
The gestational sac is the first developmental marker that can be imaged and has been reported to be 5 mm by the fifth gestational week (12). It can be seen at 4.5 to 5 weeks’ gestation with endovaginal ultrasound and at 5.5 to 6 weeks’ gestation using the transabdominal approach. The ultrasonic appearance is that of a round, anechoic (echo-free or dark) sac measuring greater than 5 mm internal diameter, surrounded by a thick concentric echogenic ring, and located within the endometrial echo.
Yolk Sac
The yolk sac has a characteristic appearance consisting of a bright, ring-like structure with an anechoic center. It is
attached to the fetal umbilicus by a narrow stalk. It is the first structure that can be accurately identified within the gestational sac. It also is the earliest reliable sign of an IUP. Endovaginal ultrasound is the preferred method for evaluating an early or atypical intrauterine sac. The presence of a yolk sac is associated with a 62% incidence of a normal pregnancy (liveborn infant) (13). It can be seen at 5 to 5.5 weeks’ gestation on endovaginal ultrasound and at 6 to 6.5 weeks’ gestation on transabdominal ultrasound. It usually is not seen after 12 weeks gestational age.
attached to the fetal umbilicus by a narrow stalk. It is the first structure that can be accurately identified within the gestational sac. It also is the earliest reliable sign of an IUP. Endovaginal ultrasound is the preferred method for evaluating an early or atypical intrauterine sac. The presence of a yolk sac is associated with a 62% incidence of a normal pregnancy (liveborn infant) (13). It can be seen at 5 to 5.5 weeks’ gestation on endovaginal ultrasound and at 6 to 6.5 weeks’ gestation on transabdominal ultrasound. It usually is not seen after 12 weeks gestational age.
TABLE 135.1 Ultrasonographic Gestational Markers for Intrauterine Pregnancy | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 Figure 135.2 Transverse view of the uterus demonstrating features of an early intrauterine pregnancy. |
The presence of a yolk sac virtually eliminates the possibility that an intrauterine gestational sac represents a pseudogestational sac of ectopic pregnancy (14). A pseudogestational sac, or pseudosac of ectopic pregnancy, is a saclike structure inside the uterus of a patient with an ectopic pregnancy. It is related to endometrial hormonal stimulation with edema fluid or blood accumulation. It can be differentiated from an early IUP by its lack of embryonic contents, absence of a double decidual sac, and lack of a definite thick, brightly echogenic decidual reaction.
Double Decidual Sac Sign
The double decidual sac sign consists of two concentric echogenic rings surrounding the gestational sac. The inner ring represents the decidua capsularis, chorionic villi, and chorion surrounding an anechoic area. The outer ring represents the decidua vera or endometrium of the uterus. The ring between these layers is anechoic and is the remnant of the uterine cavity. The presence of a double decidual sac has been described as a sign of IUP; however, it is a less reliable sign for the diagnosis of a normally developing pregnancy (15). The presence of a double decidual sac sign is therefore suggestive of an IUP but is not by itself diagnostic.
Fetal Pole
The fetal or embryonic pole is recognized sonographically as a thickened area adjacent to the yolk sac and often can be seen when the embryo is 2 mm. It can be seen at 5.5 to 6 weeks’ gestation on endovaginal ultrasound and 7 weeks’ gestation on transabdominal ultrasound.
Fetal Cardiac Activity
A fetal heart beat always should be present in a normally developing embryo at about 6.5 weeks’ gestation and can generally be seen in a 2- or 3-mm fetus. Identification of cardiac activity is of particular importance, as 97% of embryos with cardiac activity have a normal outcome (liveborn infant) (15,16,17,18). Cardiac activity is reliably seen at 6 to 6.5 weeks’ gestation on endovaginal ultrasound and at 7 weeks’ gestation on transabdominal ultrasound but often can be identified as soon as an embryonic pole is visible.
Ultrasound Findings of Ectopic Pregnancy
Findings on an ultrasound examination that suggest an ectopic pregnancy include a definitive ectopic pregnancy or a positive HCG level and no definitive IUP.
Definitive Ectopic Pregnancy
A definitive ectopic pregnancy is defined as the presence of a sac larger than 5 mm (maximum internal diameter) with a thick, concentric echogenic ring visualized outside the endometrial echo and containing a definite yolk sac or an obvious fetal pole (with or without fetal pulsations).
No Definitive Intrauterine Pregnancy
Diagnosis of an ectopic pregnancy must be strongly considered in the face of a serum human chorionic gonadotropin (HCG) level above the discriminatory zone and no IUP noted on the ultrasound examination. Serum HCG levels correlate with the size and gestational age of the embryo. The discriminatory zone of HCG (i.e., the level above which a normal IUP is reliably visualized) was first described in 1981 (15). For transabdominal sonography, this level has been most
recently set at an HCG concentration of 3,600 mIU/mL using the first international reference preparation (IRP) (equals 1,800 mIU/mL via the second international standard [IS]), which correlates to a gestational age of approximately 6 weeks. With the advent of endovaginal sonography, the discriminatory zone of HCG is currently as low as 1,025 mIU/mL IRP (approximately 500 mIU/mL second IS), consistent with 5 weeks’ gestation. The absolute minimum value of HCG identifying the discriminatory zone depends on the equipment used and the sonographer’s technique. This value should ideally be established separately for each institution. The lack of an IUP when the HCG is above the discriminatory zone, therefore, represents either an ectopic pregnancy or a recent abortion. This category accounts for the majority of ectopic cases diagnosed in an ED setting (19).
recently set at an HCG concentration of 3,600 mIU/mL using the first international reference preparation (IRP) (equals 1,800 mIU/mL via the second international standard [IS]), which correlates to a gestational age of approximately 6 weeks. With the advent of endovaginal sonography, the discriminatory zone of HCG is currently as low as 1,025 mIU/mL IRP (approximately 500 mIU/mL second IS), consistent with 5 weeks’ gestation. The absolute minimum value of HCG identifying the discriminatory zone depends on the equipment used and the sonographer’s technique. This value should ideally be established separately for each institution. The lack of an IUP when the HCG is above the discriminatory zone, therefore, represents either an ectopic pregnancy or a recent abortion. This category accounts for the majority of ectopic cases diagnosed in an ED setting (19).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


