Indications
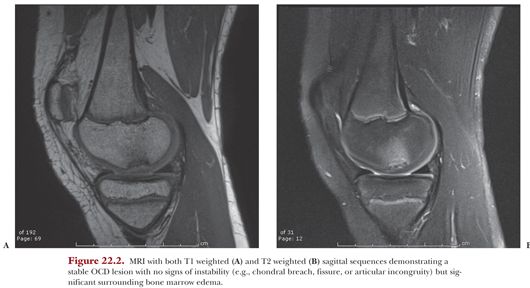
Patients with stable OCD lesions of the knee and open physes should be initially managed nonoperatively. Conservative modalities may range from simple activity modification (i.e., avoiding offending activities such as running, competitive sports, or impact activities) to protected weight bearing with crutches, bracing, and/or immobilization. Although the traditional approach of immobilization through casting is rarely pursued today, use of a locked hinged knee brace or knee immobilizer may be a reasonable substitute. Alternatively, valgus unloader bracing has the advantage of allowing knee motion while still decreasing loads on the affected medial femoral condyle. Incomplete, transient, or lack of radiographic or MRI-based healing after approximately 3 to 6 months of nonoperative treatment is generally an indication for surgical intervention.2
Drilling of the OCD lesion is considered the gold standard of surgical treatment of stable OCD in skeletally immature knees. Drilling is thought to disrupt the sclerotic margin of the lesion and consequently promote healing via growth factors released from healthy underlying cancellous bone. There are two primary methods of drilling knee OCD lesions: transarticular (or retrograde) and retroarticular (also referred to as anterograde).
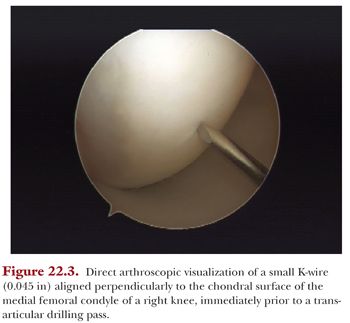
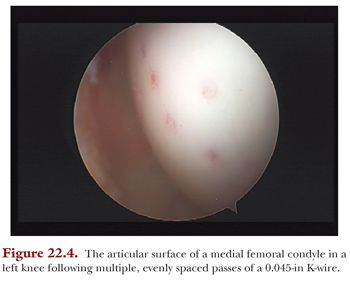
Transarticular drilling involves perforation of the articular cartilage under direct visualization of the OCD lesion, whereas retroarticular drilling through the affected condyle spares the articular cartilage and used intraoperative fluoroscopy to perforate the OCD from the backside of the lesion. Theoretical advantages of the transarticular drilling technique include relative technical simplicity and direct visualization and assessment of the OCD lesion and K-wire entry sites during drilling (Fig. 22.3). Consequently, drilling passes can be optimally spaced relative to the lesion’s borders and relative to each other (Fig. 22.4). Finally, intraoperative fluoroscopy is rarely required to localize lesion (in contrast to retroarticular drilling). The theoretical disadvantage of transarticular drilling is the direct articular surface perforation and uncertain long-term implications of these perforations. Also, from a practical standpoint, far posterior condylar lesions may be difficult to access from transarticular approach due to required knee hyperflexion.
Although high-quality studies comparing transarticular and retroarticular drilling are lacking, a recent systematic review concluded no difference in patient outcomes or radiographic healing for skeletally immature patients with stable knee OCD lesions treated with these techniques. In total, 12 studies were included which demonstrated a 91% radiographic healing rate in average of 4.5 months for transarticular drilling versus 86% in average of 5.6 months for retroarticular drilling with no differences in clinical response.3
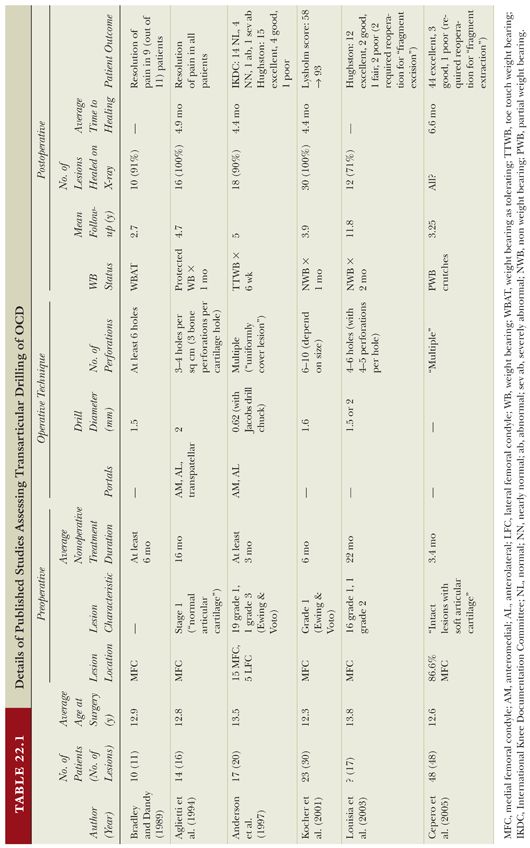
A summary of the currently published literature on transarticular drilling in isolation for the treatment of juvenile knee OCD lesions is summarized in Table 22.1.4–9 Across all studies, there is agreement on the indications for drilling, in that almost every patient had a stable OCD lesion which had failed at least 3 months of nonoperative management. The clinical and radiographic outcomes reported are excellent overall. Significant variability exists in terms of intraoperative drilling technique and postoperative rehabilitation.