FIGURE 10-1 Clinical photograph of a Blauth type IIIA hypoplastic thumb. Note lack of IP joint skin crease and thenar muscle bulk.
CLINICAL QUESTIONS
- What are the characteristic clinical features of the hypoplastic thumb?
- What medical conditions and syndromes are associated with thumb hypoplasia?
- How is thumb hypoplasia classified?
- What are the treatment principles?
- What are the indications for surgical reconstruction?
- What types of operations are performed for the hypoplastic thumb? What factors determine which types of operations to perform?
- What is a pollex abductus?
- What is a chondrodesis?
- What are the expected outcomes and potential complications of surgical treatment?
THE FUNDAMENTALS
You don’t need thumbs…My best friend is my brother’s dog. He doesn’t have any thumbs and he’s doing fine.
—Pat Angerer, Iowa Hawkeyes offensive lineman
Etiology and Epidemiology
The upper limb develops during the fourth to seventh week of gestation (see Chapter 1). A number of signaling centers have been identified that contribute to upper limb morphogenesis, patterning, and differentiation. The apical ectodermal ridge (AER) is responsible for proximal-distal development, mediated by a number of fibroblast growth factors.1 The zone of polarizing activity (ZPA) has been implicated in anterior-posterior pattern formation, mediated in part by sonic hedgehog and homeobox (HOX) gene products. Finally, the WNT7a signaling center directs dorsalventral development. While the exact mechanisms are yet unknown, it is believed that abnormalities in the AER and/or ataxic insult on the ZPA may result in thumb hypoplasia, with or without radial longitudinal deficiency.2–4
Thumb hypoplasia represents approximately 5% to 15% of all congenital hand differences.5,6 Males and females are equally affected, and the right thumb is more commonly involved than the left.7,8 In over half of cases, there is bilateral, though often asymmetric, involvement.
In up to 40% of cases, thumb hypoplasia may present in association with known syndromes (Table 10.1).7–9 Awareness of syndromic associations is critical, as often the hand surgeon is the first medical care provider to evaluate the patient; in these situations, potentially life altering diagnoses and lifesaving interventions can be made. The VACTERL syndrome denotes combined abnormalities of the vertebrae, anus, cardiovascular tree, trachea, renal system, and limb buds. (The classic “VACTERRL” syndrome involves Vertebral anomalies, Anal atresia, Cardiac defects, Tracheo-Esophageal fistula, Renal, and Radial Limb anomalies.)10–12 Holt-Oram syndrome refers to thumb hypoplasia associated with congenital heart defects, typically atrial and ventricular septal defects. The genetic mutations for Holt-Oram syndrome have been identified as involving the TBX5 gene in over 70% of patients.13 Fanconi anemia also has an autosomal dominant inheritance pattern. In infancy, there are usually characteristic facial features (microphthalmos, strabismus, and hearing deficits).14 Pancytopenia often does not present until later in childhood. Fanconi anemia can be identified by a mitomycin C test, but it is now advocated that all infants with thumb hypoplasia and/or radial-sided defects be assessed early for Fanconi anemia with the diepoxybutane test, since a delay in diagnosis can have potentially life-threatening consequences.15 Thrombocytopenia with absent radius is also from autosomal recessive inheritance. While no causative genetic mutations have been identified, patients demonstrated deletions on the long arm of chromosome 116; both the c-mpl gene and the HOX genes have been implicated.17,18 The thrombocytopenia is present at birth. The platelet count usually improves with growth, and hand surgery should be delayed until it is safe.14–19
Table 10.1 Syndromes associated with thumb hypoplasia
Clinical Evaluation
Coaches have to watch for what they don’t want to see and listen to what they don’t want to hear.
—John Madden
Clinical evaluation begins with careful inspection and physical examination. To identify the underdeveloped thumb, one must understand what constitutes “normal.” In a previous study of 546 hands in 243 patients less than 18 years of age, it was determined that the tip of the adducted thumb reaches to 70% of the length of the index finger proximal phalanx, measured proximal to distal,20 and 32% of the length of the index finger from the metacarpophalangeal (MCP) joint to its tip. The widths of the thumb and thumb nail were found to be 133% and 105% that of the adjacent index finger, respectively. Interestingly, these comparisons between normal thumb and index digits remain relatively constant among patients of different ages.
Thumb hypoplasia is characterized by five distinct clinical features. First, the thumb is smaller, shorter, and narrower. Second, there may be interphalangeal (IP) joint stiffness with relative paucity of the flexion and extension creases, due to underdevelopment of the extrinsic muscles. Third, the MCP joint is typically unstable, due to ligamentous insufficiency. Fourth, the thenar muscles are underdeveloped and weak, resulting in absent palmar abduction of the thumb and a concavity of the normally prominent thenar eminence. Finally, there is often a first web-space narrowing, likely due to the imbalance between the robust adductor pollicis and weak or absent thenars. As there is a high frequency of bilateral involvement, comparison to the apparently normal contralateral thumb may often be misleading.
In situations in which there are absent or rudimentary flexion and extension creases of the IP joint, a pollex abductus should be suspected.5 Defined as an abnormal connection between the flexor pollicis longus and extensor pollicis longus tendons, a pollex abductus may be seen in up to 35% of cases and will cause the thumb to rigidly abduct when the extrinsic flexors or extensors are activated. Pre- or intraoperative identification of a pollex abductus is critical, as failure to address this anatomic abnormality may result in suboptimal surgical outcomes.
Classification systems of thumb hypoplasia assist in surgical decision making and reflect the evolution in the understanding of this condition. While Müller was among the first to categorize thumb hypoplasia, it is Blauth’s classification (and Buck-Gramcko’s modification thereof) that has withstood the test of time and is most commonly used today (Figure 10-2).21–23 A type I thumb is smaller and shorter than normal but still has all the elements that constitute a normal-functioning thumb. Type II thumbs have underdeveloped skeletal elements, MCP instability, first web-space narrowing, and intrinsic (thenar) hypoplasia. Type III thumbs have additional extrinsic deficiencies. The type IV thumb refers to the so-called pouce flottant, or floating thumb; in these situations, the rudimentary thumb is connected to the radial aspect of the hand by a narrow skin bridge without any meaningful musculature or bony connection. Type V denotes the complete absence of a thumb. Type V thumbs are thought to be most common, while type III are second most common.7,8
Two important modifications of the Blauth classification are worthy of note, as they guide surgical planning. Lister subdivided type II thumbs according to MCP joint stability; type IIA thumbs have uniaxial instability, whereas type IIB thumbs demonstrate global MCP joint instability.24 Furthermore, Manske and McCarroll subdivided type III thumbs into those with a stable carpometacarpal (CMC) joint (type IIIA) and those with unstable CMC joints (type IIIB).25 While the difference between type IIIA and IIIB thumbs is readily apparent in texts and schematic diagrams, the clinical distinction is often more challenging, particularly in the young child in whom there is incomplete ossification of the skeletal structures.
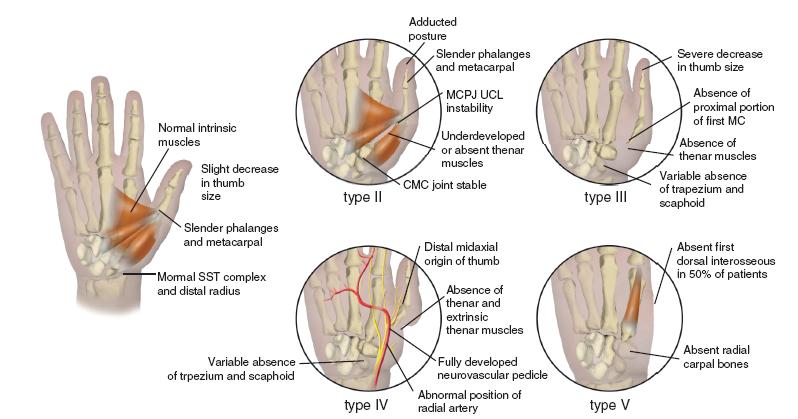
FIGURE 10-2 The modified Blauth classification.
Plain radiographs may assist in the diagnosis and guide appropriate classification, typically demonstrating hypoplastic thumb phalanges or metacarpal, often with a tapered or absent metacarpal base. Initial radiographic evaluation should include the wrist and forearm, given the high association with radial longitudinal dysplasia and radial carpal involvement.26
Given the common syndromic associations, genetic consultation with appropriate cardiac, renal, and hematologic testing are critical in the evaluation of any child with thumb hypoplasia. This includes chromosomal challenge (or chromosomal fragility) testing to rule out Fanconi anemia.27 Furthermore, thorough evaluation of the spine and lower extremities should be done to identify associated VACTERRL or other conditions.
Surgical Indications
Given the importance of the thumb in all aspects of hand function, surgical reconstruction is recommended in all but type I thumb hypoplasia.28–30 While the decision to proceed with surgery is easy for patients, families, and care providers alike, it is the type of operation to be performed that remains critical for success. In general, type II and IIIA thumbs are reconstructed, while type IIIB, I V, and V thumbs are treated with thumb ablation and index finger pollicization (see Chapter 11).
The principle of hypoplastic thumb reconstruction is simply to address each abnormal clinical element. The first web space should be deepened, the MCP joint stabilized, and opposition power restored. Little can generally be done to address size differences and thumb IP joint stiffness; for this reason, families should be counseled pre-operatively that the thumb may remain smaller in appearance and stiff at the IP joint, even with successful surgical reconstruction.
First web-space deepening is typically achieved with two- or four-part Z-plasties. Alternatively, the Brand rotation flap can be utilized (Figure 10-3).31 While pedicle or random pattern rotation or advancement flaps have been described, these are rarely needed.32,33 Opponensplasties typically utilize either the abductor digiti quinti (ADQ) (Huber opponensplasty)34–36 or the flexor digitorum superficialis (FDS) to the ring finger (see Coach’s Corner).37–40 In cases of uniaxial MCP joint instability (type IIA), the ulnar collateral ligament may be reconstructed with free tendon graft, excess FDS tendon from the opponensplasty, or local fascial tissue from the adductor pollicis. In global MCP instability, chondrodesis of the thumb metacarpal and proximal phalanx is performed and may provide the most reliable and functional outcome (Figure 10-4).41
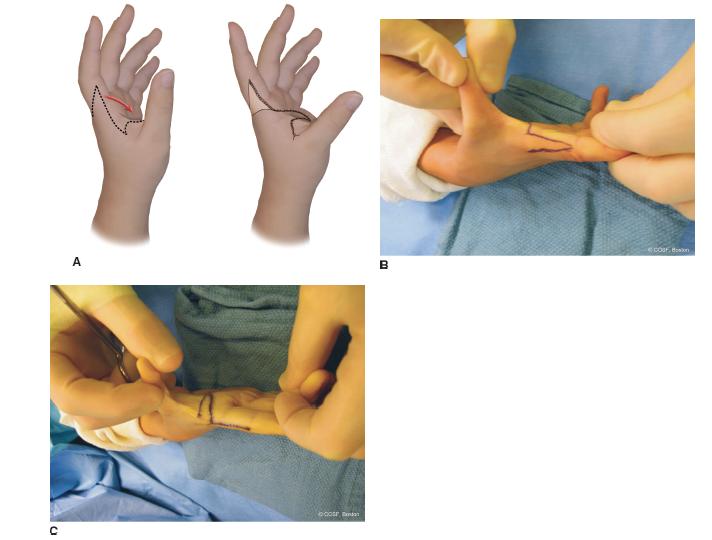
FIGURE 10-3 The Brand flap. A: Schematic diagram. B: Clinical photograph of incisions used in Brand rotation flap. C: Intraoperative appearance after rotation completed.
The optimal timing for surgery remains unclear. Surgery at or shortly before 12 months of age seems to be ideal, as the anatomic structures are large enough for easy surgical manipulation and fine motor development, and cortical representation of the thumb has not yet become ingrained.42,43
SURGICAL PROCEDURES
 Reconstruction of the Type II Thumb (First Web-Space Z-Plasty, FDS Opponensplasty, and MCP Stabilization)
Reconstruction of the Type II Thumb (First Web-Space Z-Plasty, FDS Opponensplasty, and MCP Stabilization)
Under general anesthesia and tourniquet control, the limb is exsanguinated with an Esmarch bandage and tourniquet inflated to 250 mm Hg. Z-plasty incisions are created in the first web space with the dorsal limb along the dorsoulnar aspect of the thumb. Incisions are designed in this way to facilitate later exposure to the ulnar collateral ligament of the thumb MCP joint. Care is made to incise the dermis only, to avoid iatrogenic injury to the dominant vascular pedicle to the thumb. The vessels may be reliably protected by incising the dorsal and volar incisions first, followed by gentle spreading of the tenotomy scissors to elevate the adipocutaneous flaps. The scissors may then be used to protect the underlying structures as the transverse incision is made in the web commissure. The first dorsal interosseous and adductor pollicis may then be easily identified. To maximize first web-space deepening, the fascia overlying the intrinsics is then released. If local tissue is to be used to stabilize the MCP joint, the proximal or distal origin of the fascia may be preserved to allow for subsequent ulnar collateral ligament reconstruction or reinforcement.
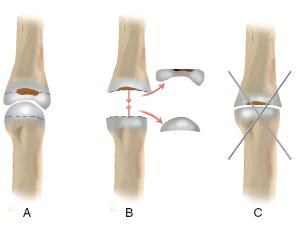
FIGURE 10-4 Schematic diagram depicting chondrodesis.
Following this, opponensplasty is performed (Figure 10-5).44 An oblique or zigzag incision is created at the level of the distal palmar crease overlying the A1 pulley to the ring finger. Longitudinal spreading is performed and the flexor tendon sheath identified. The A1 pulley is incised and the FDS isolated. Proximal traction on the tendon will allow for visualization of the FDS decussation, which is transected proximal to its rejoining at Camper chiasm and insertion on the middle phalanx in efforts to avoid secondary hyperextension deformity. A second longitudinal incision is then created radial to the flexor carpi ulnaris (FCU) and proximal to the wrist flexion crease. The FCU and FDS tendons are identified, with care made to avoid injury to the ulnar neurovascular bundle. Once the FDS to the ring finger is identified, proximal traction will allow for delivery of the distal stump into the more proximal forearm wound. The oblique/zigzag incision at the base of the ring finger is then closed with interrupted absorbable 5-0 suture (Chromic, Ethicon, Inc., Somerville, NJ). The distal radial half of the FCU tendon is then incised longitudinally, with care being made to preserve its distal attachment to the pisiform. A transverse cut is made radially, creating a free limb of FCU. The proximal end of this limb is then sutured back to the pisiform or distal FCU using nonabsorbable braided polyester sutures (Ethibond, Ethicon, Inc., Somerville, NJ) creating a pulley. The FDS is then passed through the FCU pulley. A traction suture is then passed through the FDS stump in preindenttion for transfer.
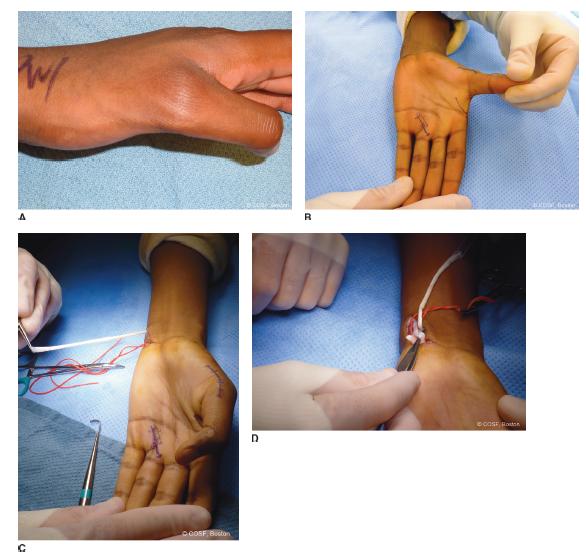
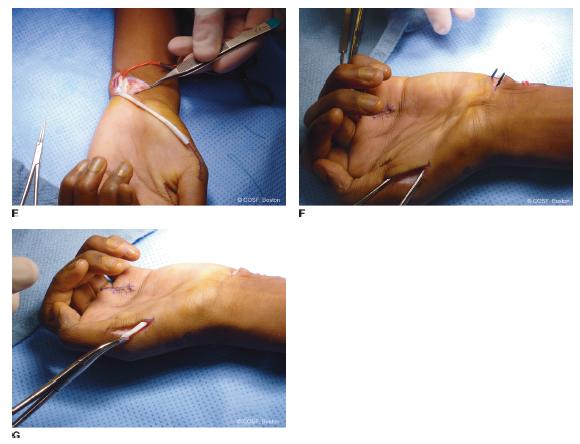
FIGURE 10-5 Surgical reconstruction of a type IIIA hypoplastic thumb using the FDS opponensplasty. A: Preoperative appearance of the hypoplastic thumb, illustrating the-nar absence. B: Surgical incisions allowing for access to the FCU and FDS in the distal forearm, FDS to the ring finger, APB insertion over the radial aspect of the thumb MCP joint, and first web-space deepening via Z-plasty. C: The FDS to the ring finger has been harvested and withdrawn into the forearm wound, allowing closure of the ring finger wound. D: A pulley is created using a distally based strip of FCU tendon sewn to itself. E: The FDS tendon is passed through the FCU pulley, and there is always adequate length for transfer and ligament stabilization. F: Using the radial incision over the thumb MCP joint, a subcutaneous tunnel may be created proximally and ulnarly to the distal forearm wound along the path of the anticipated transfer. G: The FDS tendon is brought into the radial thumb wound and sewn into the base of the proximal phalanx and APB insertion, completing the transfer. If ulnar collateral ligament reconstruction is needed for thumb stability, one slip of the FDS may be used for tendon transfer and the other slip passed to the ulnar side of the thumb for ligament reconstruction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


