FIGURE 38-1 The anatomy of the FDS and FDP tendons.
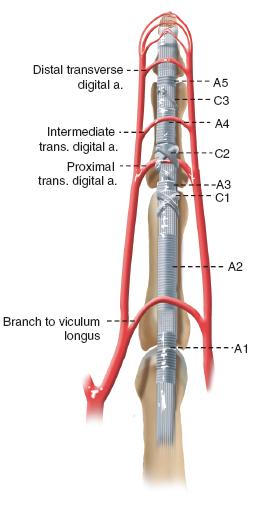
FIGURE 38-2 Schematic diagram of the annular and cruciate pulley system.
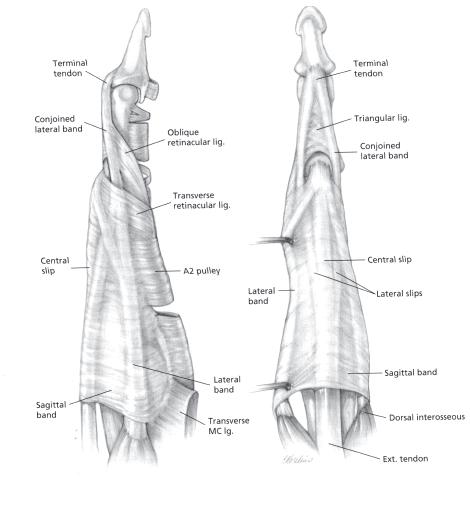
The extensor apparatus is more complex and elegant in its anatomic design (Figure 38-3). Again, the reader is referred to other sources for details regarding anatomy and basic science.1,2 The basic anatomic principles hold true for children and adults.
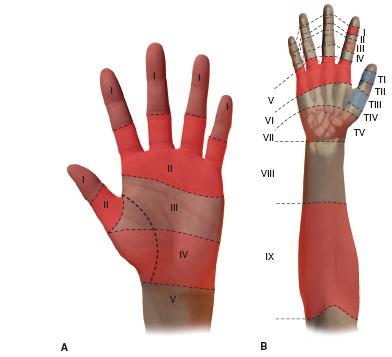
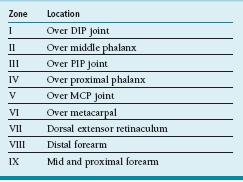
In general, tendon injuries are classified according to timing of presentation (acute or chronic), morphology (complete or partial), and anatomic location. Flexor tendon injuries are divided into zones, each with its own set of particular anatomic and surgical implications (Figure 38-4A; Table 38.1). Similarly, extensor tendon lacerations are divided into zones on the dorsal aspect of the hand (Figure 38-4B; Table 38.2).
Table 38.1 Zones of flexor tendon injury
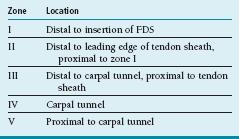
Table 38.2 Zones of extensor tendon injury
Clinical Evaluation
Clinical evaluation begins with a good history. Information regarding the acuity of injury and the mechanism is most important. In older patients, additional questions may be asked about subjective numbness or tingling of the affected digit(s) as well as the quality of bleeding at the time of injury, which suggest concomitant injury to the adjacent neurovascular bundle. (Given the anatomic relationship between the more volar digital nerve and more dorsal digital artery, any volar finger laceration with profuse bright red bleeding should raise concern for a digital nerve laceration.) Chronicity is important, particularly after closed tendon ruptures, as long-standing injuries are associated with greater tendon retraction, myostatic contractures, and the potential need for single- or two-stage flexor tendon grafting and pulley reconstruction.
Physical examination should note the location, orientation, and quality of all lacerations and wounds, however small. Remember that small superficial lacerations may mask larger tendon and soft tissue injuries beneath. The vascularity of the digits should be assessed to determine the integrity of the digital arteries and guide surgical timing. Sensibility can be evaluated using light touch (threshold) or two-point discrimination (innervation density) testing. Discriminatory sensibility is usually present in patients older than 5 to 7 years of age. In rare situations, in a young child, the warm water immersion test can be performed to assess digital nerve function; if after soaking the affected hand in lukewarm water there is no wrinkling of the glabrous skin, a digital nerve injury should be suspected (Figure 38-5)

FIGURE 38-5 The warm water immersion test. This is a 3-year-old male with a transverse laceration through the palm. After warm water immersion, note is made of wrinkling of the thumb, small, and ring fingers but absent wrinkling of the index and long fingers. At the time of surgical exploration, confirmation was made of common digital nerve injuries to the index and long fingers.
Assessment of flexor tendon integrity is performed by observation, passive motion, and active motion. Disruption of the normal digital cascade—in which each digit is slightly more flexed at rest than the adjacent radial digit—suggests flexor tendon laceration. This may be highlighted using the tenodesis effect, whereby passive wrist extension causes obligate passive digital flexion (Figure 38-6). In the young uncooperative or anxious child, compression of the FDS and FDP muscle bellies in the forearm, away from the zone of injury, is a helpful maneuver; again, absence of passive digital flexion should alert the examiner to a flexor tendon disruption. Finally, active distal interphalangeal (DIP) joint and proximal interphalangeal (PIP) joint flexion of each digit should be specifically assessed. Isolated DIP flexion is performed to test FDP function. For FDS testing, isolated PIP flexion with the other digits held in an extended position is needed to prevent the FDP—with its shared muscle belly—from flexing the tested digit. In cases of partial tendon lacerations, active flexion may be intact, but there will be pain with flexion against resistance.

FIGURE 38-6 Disruption of tenodesis, indicative of a flexor tendon injury. Note the abnormally extended position of the long finger, combined with the small, seemingly innocuous laceration in the palm. Subsequent exploration confirmed flexor tendon injury to the long finger.
Extensor tendon injuries are similarly assessed by observation and passive and active motion. Tenodesis and passive wrist extension are helpful, as is specific testing of metacarpophalangeal (MCP) joint (sagittal bands), PIP (central slip), and DIP (terminal tendon) extension. Furthermore, it is important to recognize that in the case of an isolated central slip injury (the boutonniere deformity), the digit can still be actively extended, due to the pull of the extrinsic extensors through the lateral bands to the terminal tendon. To specifically test central slip integrity, the so-called Elson’s test is used.3 The PIP joint is flexed, and the patient is then asked to extend the PIP joint. In cases of central slip injuries, the DIP joint goes into rigid extension prior to attempted PIP joint extension.
The diagnosis of tendon disruption is made clinically, though radiographic imaging may be helpful. Both ultrasound and magnetic resonance imaging (MRI) scans may be used to assess tendon integrity as well as the degree of retraction (Figure 38-7). This is particularly helpful in chronic injuries or postsurgical patients with limited motion in whom rerupture is suspected.
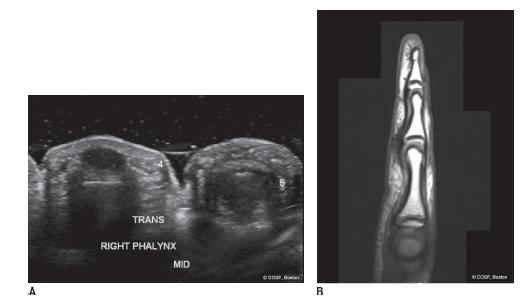
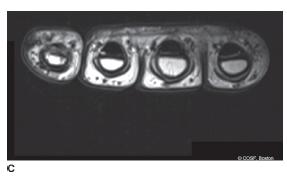
FIGURE 38-7 Radiographic imaging of a suspected flexor tendon rerupture after attempted primary tenorraphy in an 8-year-old male. A: Transverse (axial) ultrasound images depicting normal flexor tendon within the ring finger sheath (left) but absence of flexor tendon within the small finger fibro-osseous canal. B: Sagittal proton density MRI images depicting absence of the flexor tendon in zone II. C: Corresponding axial images, depicting absence of tendon within the small finger (far left) flexor tendon sheath.
Surgical Indications
Surgical repair is indicated in all patients with open extensor tendon injuries and acute complete flexor tendon lacerations. Furthermore, flexor tendon repair or reconstruction is indicated in chronic flexor tendon disruptions in patients with significant functional limitations who are willing and able to comply with postoperative rehabilitation and activity restrictions.
Hitting is timing.
—Warren Spahn
Treatment of flexor tendon injuries is dependent upon the timing from injury to surgery. In acute flexor tendon lacerations, primary tenorrhaphy is performed using minimum four-strand core suture repair supplemented by an epitendinous suture repair. When surgery is delayed >4 weeks from injury the myostatic contractures and tendon retraction may not allow for primary repair; in these cases, surgical treatment options include single-stage tendon grafting or staged flexor tendon reconstruction, depending upon the status of the fibro-osseous canal.
 Closed Treatment of Mallet Fingers and Open Mallet Finger Extensor Repair
Closed Treatment of Mallet Fingers and Open Mallet Finger Extensor Repair
Mallet finger refers to the characteristic extensor lag associated with disruption of the terminal tendon’s insertion onto the dorsal distal phalanx. In children, due to the presence of the physis, clinical mallet fingers may actually represent Salter-Harris type III fractures of the dorsal epiphysis of the distal phalanx. Radiographs of the affected digit are needed to distinguish fractures (bony mallet finger) from true soft tissue extensor tendon injuries. The standard of care for closed soft tissue mallet fingers is continuous extension splinting of the DIP joint for 6 weeks; the PIP joint is left free and PIP motion encouraged to avoid lateral band and PIP joint adhesions and stiffness, respectively. After 6 weeks, part-time extension splinting is recommended for an additional 4 weeks during sleep and sporting activities.
Occasionally, patients will present late with chronic mallet injuries. This situation is commonly seen in pediatric patients, due to either missed diagnosis or failure to comply with acute splinting. Usually, this is not painful or functionally limiting, and observation alone may be recommended. In the rare situation of the painful or functionally limiting chronic mallet finger, soft tissue reconstruction by tenodermodesis technique may be performed (Figure 38-8).4,5
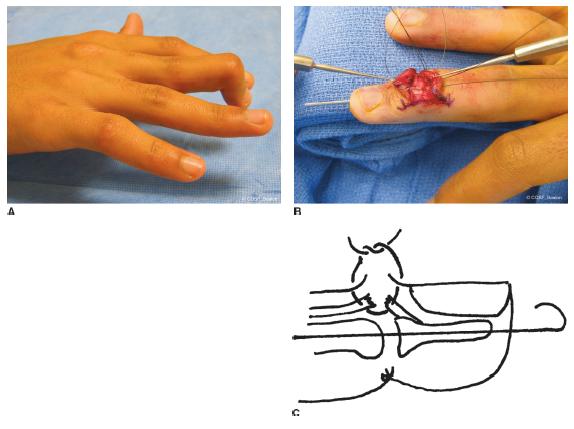
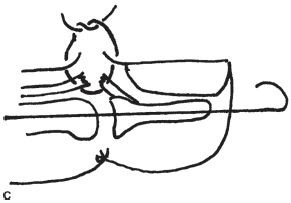
FIGURE 38-8 Tenodermodesis for chronic soft tissue mallet fingers. A: Clinical photograph of a chronic, severe long finger mallet digit. B: Intraoperative photograph depicting suture passage for tenodermodesis reconstruction. C: Schematic diagram of the tenodermodesis reconstruction.
Open mallet fingers are an indication for surgical treatment. After formal irrigation and debridement of the traumatic wound, the extensor tendon ends are mobilized, with care being taken to avoid iatrogenic injury to the germinal matrix during exposure and soft tissue dissection. The tendon ends are then reapproximated with interrupted figure-of-eight, cruciate, or core-grasping sutures; due to the thin, flat, often diaphanous consistency of the terminal tendon, traditional core-grasping sutures with heavy (3-0) braided nonabsorbable suture material may not be technically feasible. Tenodermodesis sutures may similarly be used in acute open mallet injuries if the quality of the tendon stumps is insufficient. After tendon repair, a single retrograde percutaneous pin is placed into the distal phalanx and across the DIP joint, holding the fingertip in full extension. A mallet splint or cast is applied. The pin is removed and splinting and therapy are initiated as described above 4 weeks postoperatively.
 Primary Tenorrhaphy of Acute Flexor Tendon Laceration
Primary Tenorrhaphy of Acute Flexor Tendon Laceration
Under loupe magnification, flexor tenorrhaphy begins with adequate exposure. Although a variety of incisions have been advocated, we favor a volar zigzag Bruner approach, which is extensile, allows access to the radial and ulnar neurovascular structures, and can easily incorporate traumatic wounds.6 This is particularly useful, as both the distal and proximal flexor tendon stumps may retract and reside far from the initial traumatic laceration. For example, when a flexor tendon laceration is caused by a child grasping a knife with a closed fist, the position of the tendon laceration is digital flexion; during surgery, as the finger is extended, the distal stump will lie more distal than the original wound, and the proximal tendon will retract due to the effect of the proximal muscle bellies. Skin flaps are carefully raised, and the tendon sheath and adjacent digital arteries and nerve are exposed.
Access to the flexor tendon is achieved by judicious opening of the flexor tendon sheath using the A1, C1–A3, and C3–A5 windows (Figure 38-9). Even prior to opening the sheath, tendon stumps may be localized by the characteristic hematoma that forms in the zone of injury and at the tendon ends. The A2 and A4 pulleys are preserved in an effort to avoid subsequent bowstringing. Working within these intervals, the flexor tendon stumps are identified.
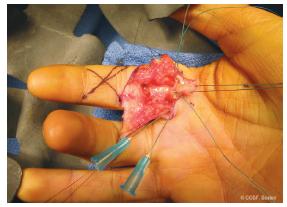
FIGURE 38-9 Clinical exposure of index finger FDS and FDP tendon lacerations. The proximal tendon stumps have been retrieved in the A1 pulley window, and core sutures have been placed. Distally, the C1–A3 interval has been opened and will be used for subsequent tenorraphy.
One of the first intraoperative challenges is reapproximating the tendon ends within the same tendon sheath window. If there has been minimal retraction—often the vincula will prevent tendon migration, particularly in the acute setting—reapproximation is straightforward. In cases of greater tendon retraction, a number of retrieval methods have been described. First, a milking maneuver is performed. With the wrist and digit flexed, pressure on the volar surface of the wrist, hand, and digit is applied in a proximal to distal fashion. Often this will provide a glimpse of the proximal tendon stump, which may then be brought into the appropriate tendon sheath window. Second, a single blind pass with a small skin hook may be attempted.7 The hook is passed into the tendon sheath with the curvature of the hook flat. After the tendon stump is felt, the skin hook is rotated 90 degrees to engage the tendon end and pull it into the window of repair. This technique should be attempted only once, as repeated passes will only increase the local trauma and thus risk of subsequent fibrosis and tendon adhesions. Finally, a pediatric feeding catheter (typically 5 or 8 Fr in diameter) can be used as a tendon shuttle. The catheter is passed retrograde from the tendon gap, through the tendon sheath, proximally, into a region where the flexor tendon is identifiable (usually beneath the A1 pulley).8 The tip of the catheter is then temporarily sewn to the intact flexor tendon with a fine 5-0 or 4-0 nylon suture. Once secured, the catheter is withdrawn, delivering the flexor tendon into the zone of intended repair. The flexor tendon is held in place by a transverse 25-gauge hypodermic needle passed across the sheath and flexor tendon.
After the tendon stumps have been identified and retrieved, preparations are made for suture passage. It is clear that thicker suture material and a greater number of strands crossing the tenorrhaphy site increase the strength of the repair. While in adults, six- or eight-strand repairs have been performed, our practice is to perform four-strand repairs using either 3-0 or 4-0 nonabsorbable braided core sutures (Ethibond, Ethicon, Inc., Somerville, NJ) supplemented by a running locked, 6-0 monofilament epitendinous stitch (Prolene, Ethicon, Inc., Somerville, NJ). This is in part due to the small size of the tendons in children as well as our choice of postoperative rehabilitation. Currently, we perform a Strickland-type repair, which utilizes a Tajima core suture and horizontal mattress9 (Figure 38-10). The back wall (dorsal) running epitendinous suture is placed first, followed by the core sutures. Core sutures are then tied at the tenorrhaphy site or outside the zone of injury, and the epitendinous sutures are completed around the front (volar) wall. Epitendinous sutures are critical in tenorrhaphies performed in tendon sheaths, due to the increase in strength and decrease in the friction/work of flexion achieved by the tidying of the repair site.10,11 In situations where the tendon ends are easily reapproximated without undue tension, an “epitendinous first” repair may be done.
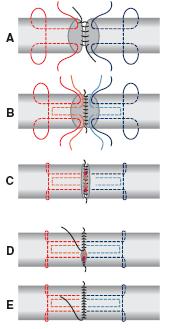
FIGURE 38-10 Schematic diagram of a four-strand core suture repair supplemented by a running epitendinous suture.
While both the FDP and FDS tendons are repaired in this manner, special considerations are made regarding injuries to the FDS slips distal to their bifurcation within zone II. Anatomically, the FDS slips are smaller, thinner, and flatter than the FDP or more proximal FDS tendon. Furthermore, given the passage of the FDP tendon through the FDS slips, excessive bulk or constriction may lead to limitations in FDP excursion and digital motion. We advocate repair of both the FDS and FDP whenever possible. Due to the small size of the FDS slips, tenorrhaphy is often performed using figure-of-eight or cruciate sutures. If excursion of both tendons is limited after completion of the repairs, a single FDS slip is considered.
After primary tenorrhaphy, every effort is made to avoid tendon gapping at the repair site as well as excessive girth or “bulging” of the repair. With passive digital flexion and extension, there should be no triggering or block to motion.
The wound is then closed using interrupted absorbable simple skin sutures (Chromic, Ethicon, Inc., Somerville, NJ). A bulky sterile bandage is applied, followed by a dorsal splint or more commonly a hand-based cast, holding the wrist in approximately 30-degree flexion, MCP joints at about 70-degree flexion, and IP joints straight. We avoid placement of cast material on the palmar aspect of the hand to prevent giving our pediatric patients a firm surface against which they may grasp and flex, thereby increasing the risk of rerupture.
 Flexor Tenolysis
Flexor Tenolysis
Persistent limited range of motion following flexor tendon repair can be a vexing and challenging problem in children. The differential diagnosis of persistent stiffness following flexor tenorrhaphy includes tendon rerupture, adhesions, and joint contractures. These three clinical conditions may be distinguished through careful physical examination. If the digit has incomplete passive motion, the presumption is that joint contracture is the cause; indeed, no comment can be made upon tendon adhesions or rerupture in the setting of a rigidly stiff digit. Aggressive therapy is needed to reestablish tissue homeostasis and passive joint motion. If passive motion is intact but active flexion is limited, the distinction should be between rerupture and adhesions. If the patient is able to resist passive flexion or demonstrates isolated active flexion through the allowable arc of motion, the tendon is intact and adhesions are the cause. If no active flexion is noted, rerupture is a concern. As cited above, ultrasound or MRI may be a helpful adjunct to the clinical diagnosis.
Although children generally do not demonstrate the same propensity to postoperative adhesions and longstanding loss of passive digital motion as adults, tendon adhesions do occur. While tenolysis can be performed, the results of tenolysis in children are more unpredictable than in adults.12–14 This is in part due to limitations in surgical technique (e.g., the need for general anesthesia, small size of the anatomic structures) as well as persistent obstacles in compliance with postoperative therapy, which may result in recurrent adhesion formation. Therefore, the indications are very specific, and tenolysis should not be performed without thorough discussion with both patient and family.
Indications for tenolysis include persistent functionally limiting digital stiffness or contractures despite maximization of hand therapy. Tenolysis should only be performed after wound healing, scar management, and soft tissue homeostasis has been normalized, usually 6 months after the index procedure.15–17 Furthermore, tenolysis is generally contraindicated in patients <10 years of age, due to the unpredictability of the results.13
Despite the advantages of tenolysis under local anesthesia, which have been well documented in adults, release of tendon adhesions is commonly performed under general anesthesia in children18,19 (Figure 38-11). Under tourniquet control, an extensile volar zigzag Bruner incision is utilized, incorporating prior surgical incisions whenever possible. The tendon sheath is identified, and confirmation is made that the pulley system is intact. (Whenever flexor tenolysis is performed, the surgeon should be prepared for the possible need for pulley reconstruction and/or first-stage tendon reconstruction; care should be taken to have the appropriate equipment and implants available if needed.) The flexor tendons are identified distal and proximal to the zone of prior injury/surgery, typically requiring release of the A1 pulley and identification of the tendon in the palm. A vessel loop or other elastic is placed around the FDS and FDP to provide traction.20 The A1, C1–A3, and C3–A5 windows within the tendon sheath may be utilized if necessary, but the A2 and A4 pulleys should be preserved and as little surgical dissection and sacrifice of the tendon sheath should be performed as possible. Adhesions between the FDS and FDP and between the tendons and the tendon sheath are released in a gradual, circumferential, and systematic fashion. While tenolysis knives and suture/wire loops have been used, our preference is to use appropriate-size blunt elevators (Freer elevator, Cottle elevator) for adhesion release. Serial dilation of the tendon sheath can also be performed using pediatric feeding catheters ranging from 3 to 8 Fr in caliber. With surgical patience and persistence, adhesions can be released without disrupting tendon continuity or tendon sheath integrity. Confirmation of adequate release is made by proximal traction on the tendons, which should allow for full digital flexion.
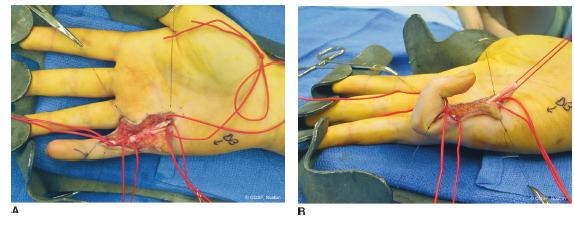
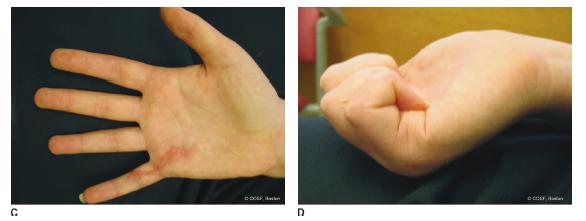
FIGURE 38-11 Flexor tenolysis in a 14-year-old female with persistent tendon adhesions following prior zone II flexor tenorraphy. A: Surgical exposure via a volar, zigzag incision and preservation of the A2 and A4 pulleys. B: After tenolysis and release of all adhesions, passive traction of the flexor tendons allows for full passive digital flexion. C: Postoperative appearance of surgical incisions in full digital extension. D: Postoperative digital active flexion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree