FIGURE 28-1 Radiographs show a displaced type III lateral condylar humerus fracture.
CLINICAL QUESTIONS
- How are humeral lateral condylar fractures classified?
- What are the associated injuries?
- What radiographs are most useful for diagnosis and management planning?
- When is a MRI or CT scan indicated?
- What are the indications for closed treatment?
- When is closed reduction percutaneous pinning (CRPP) indicated?
- When is an intraoperative arthrogram useful?
- Which fractures should be treated with open reduction internal fixation (ORIF)?
- What are the risks of ORIF?
- What are the complications of lateral condylar fractures and their treatment?
THE FUNDAMENTALS
Etiology and Epidemiology
Lateral condylar fractures of the distal humerus occur less frequently than supracondylar fractures, accounting for 15% to 20% of all pediatric elbow fractures. Like most children’s upper limb injuries, they occur secondary to a fall or traumatic collision with another person or immobile (ground, building, tree) or mobile (car, bike) solid object. There is some debate as to whether during the injury the radial head “pushes off” the lateral condyle with a compression force or the forearm and extensor-supinator muscle origins “pull off” the lateral condyle with valgus-extension stress. The controversy makes for interesting academic discussion and paper publications1–3 but really matters little in the simple “bone be broke, bone needs to be fixed” clinical scenario that we, the surgeon, the affected child, and his or her family confront.
Clearly understanding the distal humeral articular anatomy and soft tissue attachments about the elbow is key to proper diagnosis and management of this problem. The extensor-supinator muscle mass of the forearm, wrist, and hand originates from the metaphysis of the lateral condyle of the humerus. The lateral collateral ligament complex consists of the radial collateral ligament (from the isometric point on the lateral epicondyle to the annular ligament), lateral ulnar collateral ligament (from the lateral epicondyle to the crista supinatoris), and annular ligament (Figure 28-2).
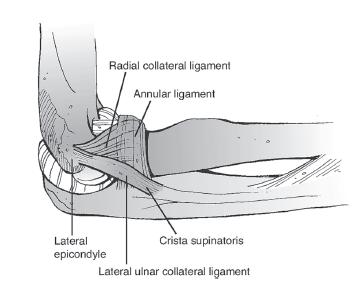
FIGURE 28-2 Ligamentous anatomy of the radiocapitellar joint and proximal radioulnar joint (PRUJ). The lateral collateral ligament extends from the isometric point on the lateral epicondyle to the crista supinatoris on the proximal ulna. The radial collateral ligament and the annular ligament stabilizing the PRUJ are noted. (From Bucholz RW, Court-Brown CM, Heckman JD, Tornetta P. Rockwood & Green’s Fractures in Adults.7th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2010, with permission.)
Clinical Evaluation
A child with an elbow fracture invariably presents with a swollen, tender elbow. The lateral condylar fracture patients do not have as much deformity as the supracondylar fracture or elbow dislocation patients. Tenderness and ecchymosis on the lateral elbow are very helpful in proper clinical diagnosis, especially in the stable and/or minimally displaced fractures.4 There may be crepitus with range of motion, though most children will not tolerate movement of the elbow in the acute setting. The diagnosis is really made by radiographs, with specific anteroposterior (AP), lateral, and internal oblique views of the distal humerus being necessary for accurate diagnosis of fracture displacement and risk of further displacement with cast treatment.5
The capitellum is the first secondary center of ossification to appear, usually between 1 and 2 years of age. The diagnosis of a lateral condylar fracture can be made accurately by plain radiographs. It can be confused with a posterolateral elbow dislocation, distal humerus physeal, or supracondylar fracture if the clinician does not properly define the alignment of the radius and ulna, distal humerus articular and physeal structures, and distal humerus metaphyseal region to one another. The fracture starts in the lateral condylar metaphyseal region and extends distally and medially to or through the articular surface. The radiographic classification systems are based on the path of the fracture through the distal humerus and the degree of displacement. The Milch classification (Figure 28-3) distinguishes a type I fracture directly through the secondary center of ossification from a type II fracture that extends over medially and exits through the ulnartrochlear groove. Mirsky et al.6 have added a third type of fracture that extends even more medially and exits through the physis. The transphyseal fracture is harder to distinguish by x-ray due to the lack of ossification medially at a young age. We rarely use the Milch system but teach it to our trainees, as certifying exams continue to ask about it, and it does help trainees better understand the distal humeral articular anatomy. The Jakob classification1 (Figure 28-4) is more useful for treatment decision making as it is based on the degree of displacement and, therefore, implies fracture stability and defines articular alignment. Type I fractures are displaced <2 mm; with type II fractures, the articular surface is displaced >2 mm but is not malrotated; and type III fractures have more marked displacement including malrotation. The accuracy of articular malalignment has been confirmed using magnetic resonance imaging (MRI) and computed tomography (CT).7–10 It can be difficult to define fracture stability with minimally displaced fractures. Oblique radiographs will reveal maximum displacement and should be obtained in all lateral condylar humerus fractures. Besides initial and serial radiographs, ultrasounds, MRI, and CT scans have been used to better define stability in order to avoid malunion or nonunion consequences in unclear situations.10–13 The treating surgeon has to define the articular displacement and fracture instability in order to make the appropriate treatment decisions for each patient with a lateral condylar humerus fracture.
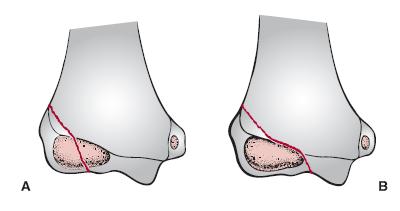
FIGURE 28-3 Milch classification of lateral condylar humerus fractures with type I (A ) extending into the joint through the capitellar os-sification center and type II (B ) entering the joint at the ulnartrochlear groove. (From Beaty JH, Kasser JR. Rockwood & Wilkins Fractures in Children. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2010, with permission.)
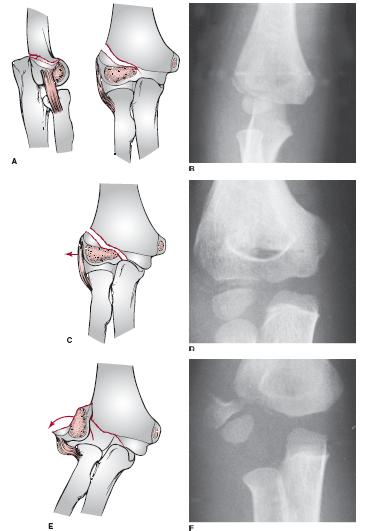
FIGURE 28-4 Jakob classification of lateral condylar humerus fractures in children with type I (<2 mm displacement) hinging the joint but not entering the joint; type II entering the joint with displacement of >2 mm but no malrotation; type III with complete displacement and malrotation. (From Beaty JH, Kasser JR. Rockwood & Wilkins Fractures in Children. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2010, with permission.)
Associated injuries need to be defined. Although rare, radial neck, olecranon, and Monteggia fractures; elbow dislocations; and floating elbow injuries all do occur in conjunction with lateral condylar humerus fractures. Finally, the capitellar shear fracture is a seindentte entity that can be missed on plain radiographs (Figure 28-5). This fracture is high risk for long-term complications, even with early accurate diagnosis and appropriate ORIF. Analysis with CT scan is very helpful to define the fracture location, pattern, and size of the fracture fragment in preindenttion for surgery.

FIGURE 28-5 A: Lateral x-ray of a displaced capitellar shear fracture. B, C: Tomograms of displaced capitellar shear fracture on AP (B ) and lateral (C ) views.
Surgical Indications
A lateral condylar humerus fracture with articular incongruity >2 mm (Jakob II and III fractures) needs surgical reduction and stabilization. Often the reduction and stabilization can be anatomically performed by percutaneous techniques in the mild type II fracture. With the very unstable type II fracture or with marked articular surface malrotation (type III), ORIF is indicated.
It isn’t the mountains ahead to climb that wear you out; it’s the pebble in your shoe.
—Muhammad Ali
 Nonoperative Treatment
Nonoperative Treatment
Minimally displaced (<2 mm) lateral condylar fractures (Jakob type I) as confirmed by AP, lateral, and oblique radiographic views are ideal candidates for closed treatment. Bivalved long-arm cast, collar and cuff, splint and sling have all been used successfully14–16 The fracture will heal in 3 to 6 weeks. Immobilization in forearm supination and wrist extension has been used to lessen muscle tension on the lateral condyle and therefore the risk of fracture displacement. These nondisplaced fractures should be stable, and supination and wrist extension positioning may be overkill. However, there will be a rare fracture that you never expected to displace, yet it does.17 Vigilant use of close, follow-up radiographs is necessary to catch the “rule breaker.” The false assumptions in these rare situations are that: (1) the articular surface is always intact and stable and (2) the soft tissue injury is minor. Protective immobilization should continue until there are clinical and radiographic signs of bony healing. If the fracture displaces or fails to heal in a timely manner, then CRPP is required (Figure 28-6).
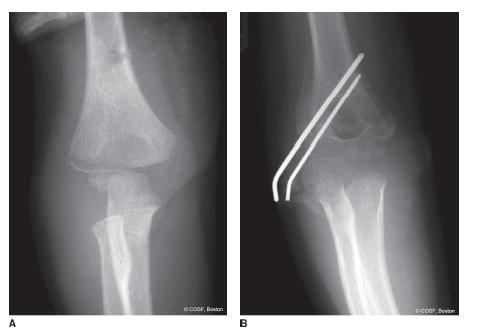
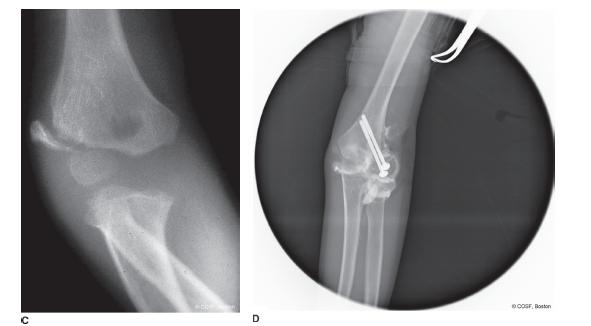
FIGURE 28-6 A: Minimally displaced type II lateral condyle fracture, preoperative for CRPP with arthrogram to confirm anatomic joint reduction. B: Similar healed fracture treated with CRPP. C: Type II fracture presenting late with delayed union. Plan is preoperative MRI to assess joint alignment and, if feasible, intraoperative CRPP or percutaneous screw fixation with arthrogram. D: Another case of delayed malunion treated with percutaneous screw fixation and arthrogram.
 CRPP or Screw Fixation with Arthrogram
CRPP or Screw Fixation with Arthrogram
If you make every game a life-and-death proposition, you’re going to have problems. For one thing, you’ll be dead a lot.
—Dean Smith
Closed reduction of almost all type II and some rare, malrotated type III lateral condylar fractures is feasible.5 Varus stress with the forearm supinated is utilized for reduction. Elbow extension with the varus stress and supination position is most reliable for reduction of most fractures. After successful closed reduction, percutaneous pin fixation is performed to stabilize the fracture. The results of CRPP are better than closed reduction and immobilization in terms of malunion and nonunion.18 Two divergent, lateral entry pins that penetrate the far cortex (similar to supracondylar fractures [see Chapter 27]) are used (Figure 28-7).19 A third pin indentllel to the joint from the lateral to the medial condyle helps with articular reduction and stability. In situations when there is uncertainty about the articular reduction and/or stability, an arthrogram for confirmation and stress testing is indicated.20


FIGURE 28-7 A: AP and lateral radiographs of type II displaced lateral condylar humerus fracture. B: CRPP with two pins. C: Radiographs after pin removal. There is a small lateral spur present. D: Displaced lateral condylar fracture in an older child treated with (E ) three-pin CRPP and arthrographic confirmation of joint reduction.
If the metaphyseal fracture is large enough, cannulated compression screw fixation can be used.21 There is usually only room enough for one screw, and it should never violate the olecranon fossa. A second smooth pin separate from the compression screw guide pin will prevent malrotation of the fragment during compression of the screw and fracture. That second pin can be removed in the operating room or later depending on the stability of the fracture fixation. We use a washer for broad compression. These screws usually need to be removed in 6 months in the day surgery unit due to local irritation.
Some surgeons will even violate the lateral condylar physis with a screw as they do not consider lateral physeal growth arrest a risk or a problem. There is insufficient evidence to be completely reassuring on that point.
 Open Reduction Internal Fixation
Open Reduction Internal Fixation
Most ball games are lost, not won.
—Casey Stengel
Although many lateral condylar fractures can be treated with CRPP, type III fractures with marked malrotation and fragment instability are still best treated with ORIF by most surgeons. There is marked soft tissue disruption with the type III fracture that makes percutaneous reduction difficult. Arthroscopic techniques are not for every surgeon or every patient.22,23 Articular congruity and stability must be restored, and an open reduction has the highest likelihood of a successful outcome in the type III fracture.
The patient is positioned supine with the arm abducted on a fluoroscopic arm table. Doing this operation on the fluoroscopic image intensifier as one would for a supracondylar fracture is too limiting and runs the risk of fracture malreduction. The entire arm is prepped, and, if necessary, a sterile rather than nonsterile tourniquet is used for maximum visualization. A direct posterolateral approach directly over the fracture is used.24,25 The incision can be extensile but generally is in the 4- to 8- cm range. There is always a large fracture hematoma that leads directly to the joint. Blunt finger dissection will usually find the path into the joint without extensive dissection beyond the skin and subcutaneous incision. Gently untwisting the malrotated lateral condyle while maintaining soft tissue blood supply to the fracture fragment is critical. While the fragment is unkinked but not reduced, the joint is cleansed of all hema-toma. Repeat irrigation and suctioning are very helpful. The articular surfaces are inspected for other injuries. The soft tissues, including neurovascular bundles, are lifted off the anterior humeral surface. Retractors are placed subperiosteally across the front to visualize the joint reduction. An anatomic ulnartrochlear groove reduction has to be felt and seen. Posterior soft tissue dissection of the fragment is not performed to avoid increasing the risk of avascular necrosis (AVN). Once manually reduced (our young partners will attest that this is not always an easy task), the fracture needs to be held anatomically in place during pin fixation. Some use a bone-holding towel clamp. We often continue the Dr. John Hall tradition of a “dinner fork” reduction with a large double skin hook or truly adapted fork with two missing central prongs. Divergent pins are placed in sequence while manually maintaining reduction. One pin is indentllel to the joint; one extends up the lateral column. Both need to penetrate the medial cortex while avoiding the neighboring neurovascular structures. A third pin can be added across the olecranon fossa as necessary. After completion of the pinning, anatomic articular reduction is again confirmed by palpation and limited direct visualization. Arthrographic or arthroscopic confirmation can be used. You cannot leave the operating room with a malreduced fracture. Stay until it is verified anatomically. Limited soft tissue repair and stabilization are performed to reattach the extensor-supinator origin. This can be performed before or after pinning depending on rotational fracture stability. The pins are left out of the skin as doing this carries less risk of pin track infection than with buried pins.
 Delayed Union CRPP or Screw Fixation
Delayed Union CRPP or Screw Fixation
Some untreated or immobilized treated patients will present late with impending nonunion or malunion. If the joint is aligned, then cast treatment until healing can be successful in many cases.26–28 However, pin or screw fixation is most expedient and has the lowest risk of malunion or nonunion. A preoperative MRI scan will define the articular alignment. Most patients will merely have diastasis but not malangulation or malrotation. Manual reduction and pin fixation or compression screw reduction and fixation will reduce and secure the joint. Arthrographic confirmation is appropriate if a closed technique is used. The methods are similar to the description of CRPP or screw fixation above (Figure 28-8).
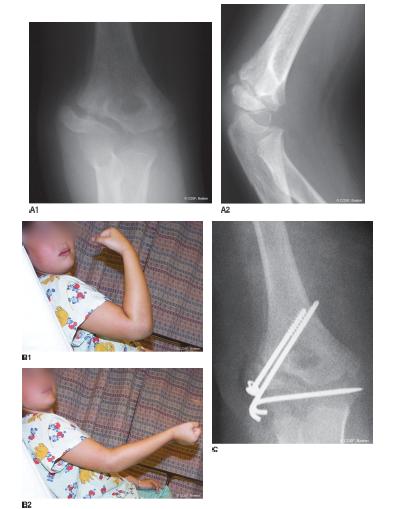
FIGURE 28-8 A: AP and lateral radiographs of a delayed union, early malunion. B: Preoperative clinical photographs of maximum flexion of this patient. C: Reduction and hybrid screw and pin fixation method to achieve union.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


