Thoracic Trauma
David W. Tuggle
Department of Surgery, Section of Pediatric Surgery, Paula Milburn Miller/Children’s Medical Research Institute, Oklahoma City, Oklahoma 73104.
EPIDEMIOLOGY
Thoracic trauma is an important cause of morbidity and mortality in children. It accounts for from 4% to 25% of pediatric trauma injuries; however, these chest injuries are associated with a greater mortality rate when compared with other system injuries (1,2,3,4,5,6,7). Isolated thoracic trauma in a child is associated with a mortality rate of approximately 5% (1), largely due to penetrating trauma. The mortality rate of head and abdominal trauma in association with thoracic trauma in children increases to 25%. Children with neurosurgical trauma, thoracic trauma, and abdominal trauma may have a mortality rate that approaches 40%. Thoracic trauma can be anticipated to be present in children who present with a low systolic blood pressure, an elevated respiratory rate, abnormalities on thoracic physical examination, including abnormal chest auscultation findings, and femur fractures (4). Eighty to 95% of thoracic injuries in children are the result of blunt trauma, typically a motor vehicle collision (2,8). Older children and adolescents are more likely to be victims of penetrating trauma, which has a higher mortality rate (5).
The child’s thorax has unique anatomic and physiologic properties that are salient to the diagnosis and management of thoracic trauma. The child’s trachea is shorter relative to body size, more anterior, narrower, and more easily compressed compared with the adult. The subglottic region is the narrowest part of the airway in children because of its small cross-sectional diameter, the pediatric airway is more susceptible to mucus plugging and small amounts of airway edema. The chest wall is more compliant in children, with less muscle mass for soft tissue protection. This allows for a greater transmission of energy to underlying organs when injury occurs. In children, the mediastinum is more mobile than in older patients, particularly in young children. Unilateral changes in thoracic pressure, such as with a pneumothorax, can lead to a tension pneumothorax. This can shift the mediastinum to the extent that venous return is markedly reduced. The pathophysiologic effect is similar to hypovolemic shock. This response is more pronounced than typically seen in an adult.
Children compensate for a decrease in cardiac output by increasing heart rate. In the infant, improvement in stroke volume provides little in the way of compensation in the hypotensive child. Children have a higher oxygen consumption per unit body mass, making them more likely to become hypoxic with injury.
RIB FRACTURES—CHEST WALL
Young children have a compliant thorax and become more adultlike at 8 to 10 years of age. As a consequence, rib fractures are relatively uncommon in young children and occur more frequently in adolescents. Rib fractures are often suspected with physical examination and identified on a chest radiograph during the initial assessment. By themselves, rib fractures are infrequently a cause of major morbidity or mortality, but they are indicators of significant energy transfer (9). If a rib fracture is found in a child less than 3 years of age, child abuse should be considered dependent on the history obtained and purported mechanism of injury (10,11). Bone scans and bone surveys are useful in diagnosing remote fractures of the bony thorax in abused children, and follow-up studies improve identification of these injuries (12). In older children, rib fractures should draw attention to the risk of associated underlying injury. Fractures and dislocations of the bony thorax and joints may cause significant long-term pain. In addition to pneumothorax and hemothorax, children with first rib fractures may have fractures of the clavicle, central nervous system (CNS) injury, facial fractures, pelvic fractures, extremity injuries, and major vascular trauma (13,14). In
the context of multiple rib fractures, careful survey of the child may reveal multiple significant injuries in other regions of the body. The management of rib fractures is typically supportive. Good pain relief will prevent atelectasis and pneumonia. Because rib fractures can be associated with hemothorax or pneumothorax, immediate drainage of fluid and blood collections or air with a tube thoracostomy is appropriate.
the context of multiple rib fractures, careful survey of the child may reveal multiple significant injuries in other regions of the body. The management of rib fractures is typically supportive. Good pain relief will prevent atelectasis and pneumonia. Because rib fractures can be associated with hemothorax or pneumothorax, immediate drainage of fluid and blood collections or air with a tube thoracostomy is appropriate.
Multiple rib fractures in series (flail chest) are not commonly seen in children (15). However, when flail chest does occur, respiratory effort can be depressed with paradoxic motion of the flail segment. Treatment of the pediatric flail chest includes good pain relief, adjusted to avoid respiratory depression. Nonsteroidal antiinflammatory drugs (NSAIDs) are useful to treat rib fracture pain after the acute phase. Occasionally, positive pressure ventilation may be required in children with a flail chest and respiratory insufficiency. In the case of a severe flail chest, there is some evidence to suggest that operative fracture stabilization of a flail chest will decrease morbidity and improve outcome in selected cases (16). In the adult, where a rib fracture or multiple rib fractures are identified, one’s index of suspicion for concomitant injuries is elevated. Examples include a pulmonary contusion and spleen or liver injury. Of note, in adults with a splenic injury, there is a 40% association with left inferior rib fractures. In children, with a splenic injury, only 10% have similar rib fractures. Therefore, the lack of rib fractures should not decrease the surgeon’s concern regarding associated internal injuries.
Chylothorax caused by injury to thoracic lymphatic channels is an uncommon complication of thoracic trauma. Chylothorax usually becomes evident 3 to 7 days after injury. Diagnosis is made by obtaining a sample of the pleural fluid and identifying the lymphatic and lipid content. Treatment includes tube thoracostomy and either enteral feedings with medium-chain triglycerides or parenteral nutrition.
Posttraumatic causalgia, or reflex sympathetic dystrophy, may be caused by an injury to a peripheral nerve in the chest. NSAID therapy is the first line of treatment. Prolonged or severe pain might require regional nerve blocks for control. This form of pain includes intercostal radicular pain, which may occur after rib fractures, chest tube placement, or thoracotomy.
LUNG INJURY
One of the most common thoracic injuries in children is a pulmonary contusion, which can occur with blunt or penetrating trauma (1) (Fig. 25-1). The flexible chest wall of the child allows contusion of the lung without rib fracture,
resulting in areas of lung consolidation and chest wall contusion. Microscopically, pulmonary contusions show alveolar hemorrhage, consolidation, and edema. The presence of a pulmonary contusion contributes to decreased pulmonary compliance, hypoxia, hypoventilation, and a ventilation perfusion mismatch. A chest radiograph taken during the initial assessment may demonstrate a pulmonary contusion. However, because this is invariably a supine film, it is sometimes difficult to differentiate fluid/blood free in the pleural space from a lung contusion. To this end, a chest computed tomography (CT) scan can show areas of pulmonary contusion not appreciated in the radiograph and differentiate a parenchymal process (contusion) from free fluid (17). Because the degree of impaired oxygenation after pulmonary contusion is related to the volume of the lung injury (18), a significant percentage of children with pulmonary contusion will require ventilatory support. The overall injury severity, associated injuries, and outcomes in these patients are similar to those seen in adults (19). Treatment includes appropriate fluid resuscitation, supplemental oxygen, pain management, and strategies to prevent atelectasis and pneumonia.
resulting in areas of lung consolidation and chest wall contusion. Microscopically, pulmonary contusions show alveolar hemorrhage, consolidation, and edema. The presence of a pulmonary contusion contributes to decreased pulmonary compliance, hypoxia, hypoventilation, and a ventilation perfusion mismatch. A chest radiograph taken during the initial assessment may demonstrate a pulmonary contusion. However, because this is invariably a supine film, it is sometimes difficult to differentiate fluid/blood free in the pleural space from a lung contusion. To this end, a chest computed tomography (CT) scan can show areas of pulmonary contusion not appreciated in the radiograph and differentiate a parenchymal process (contusion) from free fluid (17). Because the degree of impaired oxygenation after pulmonary contusion is related to the volume of the lung injury (18), a significant percentage of children with pulmonary contusion will require ventilatory support. The overall injury severity, associated injuries, and outcomes in these patients are similar to those seen in adults (19). Treatment includes appropriate fluid resuscitation, supplemental oxygen, pain management, and strategies to prevent atelectasis and pneumonia.
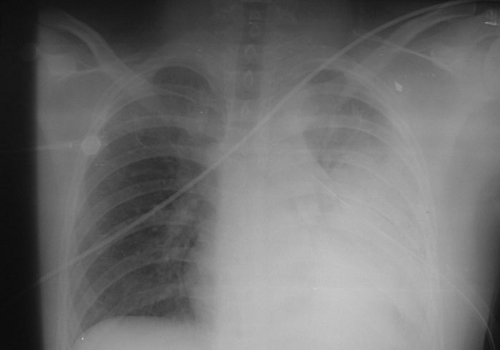 FIGURE 25-1. Gunshot wound to the left chest in a 16-year-old male after tube thoracostomy. Note the persistence of the pulmonary contusion after drainage of the hemothorax. |
A significant percentage of patients may develop pneumonia or adult respiratory distress syndrome (ARDS) after pulmonary contusion (17). In an occasional patient, pulmonary contusion may cause life-threatening hypoxia that cannot be supported with conventional ventilation, including high-frequency oscillation. Extracorporeal life support has been used in extreme circumstances to support patients with severe pulmonary contusion or ARDS (20). Children with pulmonary contusions may have prolonged changes in respiratory function and radiographic abnormalities. These changes may persist for an extended period of time after the resolution of the symptoms (21).
PNEUMOTHORAX—PULMONARY LACERATIONS
Pneumothorax is a relatively common finding in children with blunt and penetrating thoracic trauma. Blunt trauma can cause a pneumothorax if the lung is lacerated by a rib fracture or if sudden pressure causes disruption of an alveolus or any part of the airway more proximally. Trauma to the chest can cause a hemothorax, in addition to a pneumothorax more commonly seen with a penetrating injury. Air leaking from the injury may dissect under the pleura to cause pneumomediastinum and subcutaneous emphysema. A simple pneumothorax is often asymptomatic because the lack of increased intrathoracic pressure limits the recognition of symptoms. For this reason, a screening chest radiograph is an important component of the evaluation of pediatric thoracic injury. Air within the pleural cavity can layer anteriorly, posteriorly, or in the subpulmonic space, and a simple pneumothorax can be easily missed on chest film, but can be identified in a subsequent CT scan (22). The need for intervention in the presence of simple pneumothorax will depend on the degree of pneumothorax and the patient’s ongoing clinical condition. Some authors suggest that if the volume of the pneumothorax is greater than 20% of the pleural space, then chest tube drainage is indicated (23). Although insertion of a chest tube can be considered appropriate in almost every circumstance of traumatic pneumothorax, there are alternatives to conventional chest tubes, such as pigtail catheters (24). In addition, there may be a benefit to treating with supplemental oxygen alone. The rationale for this therapy is that atmospheric gas (78% nitrogen) comprises the entrapped air collection. If the nitrogen level in the blood is “washed out” by increased inspired oxygen, a nitrogen gradient will be created that will cause accelerated absorption of the air collection. Oxygen can be delivered by way of nasal cannula, a hood, or by mask. Treatment with supplemental oxygen is usually only required for 24 to 48 hours.
In contrast, tension pneumothorax is a life-threatening condition that requires expeditious decompression of the involved hemithorax. A tension pneumothorax likely causes symptoms initially due to hypoxemia (25), and later due to increased intrapleural pressure. If the clinician suspects a tension pneumothorax in a patient with appropriate signs and symptoms, it is reasonable to proceed with needle decompression of the pneumothorax without waiting for a chest X-ray to confirm the clinical suspicion. If rapid drainage of intrapleural air can be accomplished with a needle, subsequent pigtail catheter or a tube thoracostomy should be performed. A tension pneumothorax initially treated with needle decompression will usually require placement of a chest tube due to the continuing collection of air under pressure in the involved hemithorax. If one or both lungs have been under compression due to a prolonged tension pneumothorax, the risk of reexpansion pulmonary edema should be considered (26).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


