Background
The combination of the qualitative fetal fibronectin test and cervical length measurement has a high negative predictive value for preterm birth within 7 days; however, positive prediction is poor. A new bedside quantitative fetal fibronectin test showed potential additional value over the conventional qualitative test, but there is limited evidence on the combination with cervical length measurement.
Objective
The purpose of this study was to compare quantitative fetal fibronectin and qualitative fetal fibronectin testing in the prediction of spontaneous preterm birth within 7 days in symptomatic women who undergo cervical length measurement.
Study Design
We performed a European multicenter cohort study in 10 perinatal centers in 5 countries. Women between 24 and 34 weeks of gestation with signs of active labor and intact membranes underwent quantitative fibronectin testing and cervical length measurement. We assessed the risk of preterm birth within 7 days in predefined strata based on fibronectin concentration and cervical length.
Results
Of 455 women who were included in the study, 48 women (11%) delivered within 7 days. A combination of cervical length and qualitative fibronectin resulted in the identification of 246 women who were at low risk: 164 women with a cervix between 15 and 30 mm and a negative fibronectin test (<50 ng/mL; preterm birth rate, 2%) and 82 women with a cervix at >30 mm (preterm birth rate, 2%). Use of quantitative fibronectin alone resulted in a predicted risk of preterm birth within 7 days that ranged from 2% in the group with the lowest fibronectin level (<10 ng/mL) to 38% in the group with the highest fibronectin level (>500 ng/mL), with similar accuracy as that of the combination of cervical length and qualitative fibronectin. Combining cervical length and quantitative fibronectin resulted in the identification of an additional 19 women at low risk (preterm birth rate, 5%), using a threshold of 10 ng/mL in women with a cervix at <15 mm, and 6 women at high risk (preterm birth rate, 33%) using a threshold of >500 ng/mL in women with a cervix at >30 mm.
Conclusion
In women with threatened preterm birth, quantitative fibronectin testing alone performs equal to the combination of cervical length and qualitative fibronectin. Possibly, the combination of quantitative fibronectin testing and cervical length increases this predictive capacity. Cost-effectiveness analysis and the availability of these tests in a local setting should determine the final choice.
Preterm birth, defined as birth at <37 weeks of gestation, occurs worldwide in 15 million babies and accounts for 11% of all live births. In 1.1 million of these births, prematurity results in death of the child, thus making preterm birth the leading cause of neonatal deaths; in case of survival, preterm birth is an important cause of morbidity. Accurate identification of women who will deliver in a short time allows targeted interventions (such as corticosteroids, magnesium sulphate, and in utero transfer to a perinatal center) that improve outcome among those who indeed deliver preterm, thus avoiding unnecessary interventions with potential side-effects for women at low risk. However, the large majority of women who have symptoms of preterm labor will not deliver within 7 days, and 50% will deliver at term.
Among various methods to assess the risk of preterm birth, fetal fibronectin (fFN) testing and cervical length measurement are used widely; fFN is a glycoprotein that is found at the choriodecidual interface and traditionally is used as a binary bedside test that provides a positive or negative result based on a threshold of 50 ng/mL. The combination of cervical length measurement and fFN testing has a high negative predictive value (>98%) for delivery within 7 days; however, positive prediction is poor. The best strategy to combine the 2 tests is additional fFN testing in women with a cervical length of 15–30 mm, which reduces the number of unnecessary referrals and admissions to perinatal centers. This approach would also be a cost-saving without compromising neonatal health outcomes.
A new bedside quantitative fFN test showed potential additional value over the conventional qualitative test with a higher risk for preterm birth with increasing levels of fibronectin. The positive predictive value for preterm birth on short-term and preterm birth at <34 weeks of gestation increased by changing the threshold from 50 ng/mL to 200 ng/mL or 500 ng/mL, with minimal effect on the negative predictive value.
Here, we prospectively evaluated whether, in women with symptomatic preterm birth, the combination of quantitative fFN testing and cervical length measurement has better predictive accuracy than qualitative fFN testing with cervical length measurement or than quantitative fFN testing alone.
Materials and Methods
We conducted a European multicenter cohort study in 10 centers in 5 countries (4 centers in The Netherlands, 2 in Switzerland, 2 in Belgium, 1 in Germany, and 1 in Austria). They are all perinatal centers that serve as tertiary referral centers for high-risk obstetric patients with an annual number of women delivering between 1000 (Antwerp University Hospital) and 4000 (University Hospitals of Geneva). The study protocol was approved by the ethics committee of the Academic Medical Centre Amsterdam, the University Hospitals of Geneva, and the University Hospital Basel and by the board of directors of the other participating centers in Germany, Austria, and Belgium. Written informed consent was obtained from all participants before inclusion.
Women with symptoms of preterm labor (>3 contractions per 30 minutes, vaginal blood loss, or abdominal or back pain) who were at 24–34 weeks of gestation and who had intact membranes were eligible for participation in the study. Gestational age was based on first-trimester ultrasound assessment. The women either presented themselves directly at 1 of the participating centers or were referred by their primary gynecologist from a general hospital (secondary care) or by a general practitioner or midwife (primary care). Women who had received tocolytic treatment for >18 hours were excluded from the study. Women with contraindications for tocolysis (such as a lethal congenital abnormality, suspected intrauterine infection, nonreassuring fetal status, or maternal distress that required immediate intervention such as placental abruption or severe vaginal blood loss) were excluded. Other exclusion criteria were cervical dilation of >3 cm and triplet or higher order pregnancies. Women who had iatrogenic delivery within 7 days after study entry for hypertensive disorders, fetal distress, or other reasons for immediate delivery were excluded. We intended to include 500 women (ie, 100 women per country). We derived a sample size with the aim to estimate the sensitivity of the quantitative fFN test with sufficient precision. If the performance of the quantitative fFN test would resemble the qualitative fFN test with a cut off value of 50 ng/mL, the expected sensitivity would be 91% (based on a Dutch cohort study from 2009). Inclusion of 100 patients with subsequent preterm delivery would produce a 2-sided 95% confidence interval, with a width equal to 0.112 around the expected sensitivity of 91%. In view of an expected prevalence of preterm birth of 20%, we would have to include a total of 500 women with complaints of threatened labor.
After study enrolment, all women underwent cervical length measurement and fFN testing. Cervical length was measured by transvaginal ultrasound scanning. FFN testing was performed with the use of the quantitative Rapid fFN 10Q analyzer (Hologic Inc, Marlborough, MA) according to manufacturer’s instructions. A 50-ng/mL cut-off was used for the qualitative result of the fFN test (positive, negative). The qualitative fFN result was available immediately for the use in patient care, but the quantitative fFN result remained blinded until after delivery (the analyzer generated a random 3-letter result code). When the study started, both cervical length measurement and the qualitative fFN test were standard care for risk stratification in women with symptoms of preterm labor in all participating centers. Clinicians were trained in transvaginal ultrasonography and performed cervical length measurements themselves. Furthermore, all involved personnel were trained in the use of the specimen collection and the fFN analyzer. Preferably, a specimen had to be collected before the vaginal examination or cervical length measurement. Furthermore, additional information on the maternal condition was obtained and included vaginal digital examination, maternal serum for C-reactive protein and leukocytes, urine and vaginal culture, and blood pressure. In addition, data collection included information on factors that might influence the fFN result, such as the use of vaginal soap or sexual intercourse within 24 hours before the performance of the fFN test and vaginal bleeding during testing.
Treatment recommendations were based on previous research. We recommended starting tocolysis and steroids for fetal lung maturation in high-risk women, who were defined as women with a cervical length of <15 mm and as women with a cervical length of 15–30 mm with a positive fFN result. For low-risk women with a cervical length of >30 mm, we recommended to withhold steroids and tocolysis. For women with a cervical length of 15–30 mm in combination with a negative fFN test, the clinician on-call decided whether to start tocolysis and steroids. Tocolytic drugs that could be prescribed were beta-sympathomimetics, nifedipine, atosiban, and indomethacin. Magnesium sulphate for neuroprotection and antibiotics were given on consideration of the attending physician.
The primary outcome was spontaneous preterm birth within 7 days after study entry. We used logistic regression analyses with an interaction term to assess the relationship between potential influencing factors and the quantitative fFN result, such as transvaginal ultrasound, vaginal examination, the use of vaginal soap or sexual intercourse within 24 hours before performance of the fFN test and vaginal bleeding during testing. Quantitative fFN was analyzed as a continuous variable; all other factors were analyzed as dichotomous variables. Linearity of the association between quantitative fFN and the risk of preterm birth was assessed with the use of restricted cubic spline analyses, with 3 knots. If 1 of the interaction terms was significant, the factor was considered to have a confounding relation with the quantitative fFN result, and women with that factor were excluded from the analyses Descriptive statistics were calculated for baseline demographics and obstetric characteristics.
For risk stratification, thresholds of 10, 50, 200, and 500 ng/mL for the quantitative fFN test were predefined before analysis, and cervical length was divided into groups of <15, 15–29, and 30–50 mm. These thresholds were based on previous studies. The rates of preterm birth within 7 days were calculated within the corresponding strata. We considered a <5% risk of delivery as low risk. This threshold has been derived from the interpretation of cervical length, because this currently is used in clinical decision-making in women with signs of preterm labor. A cervical length measurement with a threshold of 20–30 mm corresponds to a post-test probability of delivery within 7 days of 4-5%, compared with a pretest probability of 11% if cervical length measurement is not performed. To assess whether more low-risk women could be identified with the use of the quantitative fFN test with various thresholds, we compared the accuracy to that of the qualitative fFN test (threshold, 50 ng/mL) in combination with cervical length measurement. Because the fFN test may behave differently according to parity and obstetric history, we additionally performed subgroup analyses for nulliparous women and women without a history of preterm birth.
We used logistic regression analyses to assess the univariable association between cervical length and qualitative and quantitative fFN and preterm birth within 7 days. Furthermore, we constructed 2 multivariable prediction models to predict preterm birth within 7 days: 1 model included the variables cervical length and qualitative fFN, and 1 model included the variables cervical length and quantitative fFN. Both cervical length and quantitative fFN were analyzed as continuous variables. Linearity of the association between the variables cervical length and quantitative fFN and the risk of preterm birth was assessed with restricted cubic spline analyses. We used bootstrapping techniques for internal validation of the models to correct for overfitting. Two hundred samples with the same size of the original data set were drawn from the original data set with replacement. A shrinkage factor was derived from these analyses and used to adjust regression coefficients. We compared the models in terms of overall fit using Nagelkerke R 2 and discrimination that used the area under the receiver operating characteristics curve (AUC). To determine whether quantitative fFN, as compared with qualitative fFN in combination with cervical length, improves the capability of the model to identify low-risk women (<5% risk), we compared the 2 models in terms of reclassification.
Data analyses were performed in SPSS software (version 20.0; SPSS Inc, Chicago, IL) and R (version 2.10.0; The R foundation for Statistical Computing, 2009).
Results
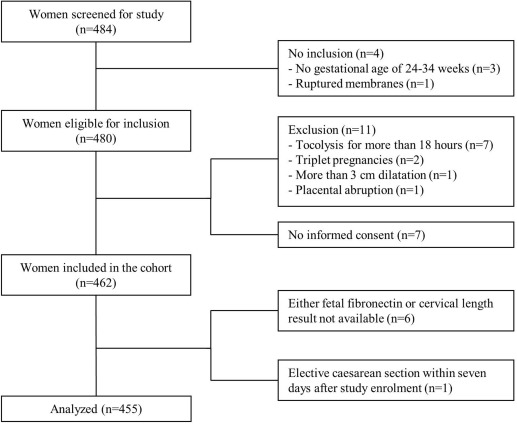
Between January 2013 and May 2014, a total of 532 women were potentially eligible for study enrolment, of whom 52 women did not meet the inclusion criteria, 11 women had ≥1 exclusion criteria, and 7 women did not give their consent to participate in the study. In the remaining 462 participating women, we performed fFN testing and cervical length measurement. The fFN result and cervical length were both not recorded in 3 women. We excluded 1 woman who had an elective cesarean delivery within 7 days after enrollment because of fetal distress. In total, 455 women were available for analysis ( Figure 1 ): 192 included in The Netherlands; 146 included in Switzerland; 55 included in Belgium; 47 included in Germany, and 15 included in Austria. Baseline demographics and obstetric characteristics for the study participants are shown in Table 1 .
| Characteristics | Values |
|---|---|
| Maternal age, y a | 29.5±5.2 |
| Gestational age at study entry, wk b | 29.6 (26.7–31.6) |
| Body mass index (n=429), kg/m 2 b , c | 24.5 (22.0–28.0) |
| White race, n (%) | 352 (77) |
| Maternal smoking (n=413), n (%) c | 41 (9) |
| Nulliparous, n (%) | 249 (55) |
| Previous preterm birth at <37 wk, n (%) | 72 (16) |
| Previous preterm birth at <34 wk, n (%) | 50 (11) |
| Multifetal gestation, n (%) | 67 (15) |
| Symptoms of preterm labor, n (%) | |
| Contractions | 395 (87) |
| Vaginal blood loss | 64 (14) |
| Abdominal or back pain | 320 (70) |
| Last prenatal visit, n (%) | |
| Perinatal center | 225 (51) |
| General hospital | 120 (26) |
| Primary care practices | 108 (24) |
| Fetal fibronectin | |
| Qualitative positive result, n (%) | 197 (43) |
| Quantitative result, ng/mL b | 34.0 (8.0–215) |
| Cervical length, mm a | 21.3±9.5 |
a Data are given as mean ± standard deviation
b Data are given as median (interquartile range)
Logistic regression analysis showed no interaction between quantitative fFN and cervical length at transvaginal ultrasound scanning (n=211; P =.98), vaginal examination (n=110; P =.44), the use of vaginal soap (n=90; P =.21), or sexual intercourse (n=20; P =.76) within 24 hours before the fFN test was performed. Similarly, there was no interaction with vaginal bleeding during testing (n=64; P =.91). Therefore, women with 1 of these characteristics were not excluded from the analyses.
Table 2 shows the risk stratification. The risk of preterm birth within 7 days increased with increasing fFN concentration (from 2% when fFN was <10 ng/mL to 38% when ≥500 ng/mL) and shortening of the cervix (from 2% when cervical length was ≥30 mm to 28% when cervical length was <15 mm). With the use of the conventional threshold of 50 ng/mL when cervical length was 15–30 mm, 164 women were identified as low risk, of whom 3 (2%) delivered within 7 days. Changing the threshold from 50–200 ng/mL in women with a cervical length of 15–30 mm would label 45 women as high risk, because 4 women (9%) delivered within 7 days. In 103 women with a cervical length <15 mm, the use of a threshold of 10 ng/mL resulted in the identification of 19 women as low risk, of whom 1 woman (5%) delivered within 7 days. Comparison of this proportion to women with an fFN concentration of >10 ng/mL with the use of a Fisher’s exact test showed the difference to be statistically significant ( P =.01). Two of 82 women (2%) with a cervical length of >30 mm delivered within 7 days. Both women had an fFN concentration of >500 ng/mL (33% of this group), which showed to be significantly different from the women with an fFN concentration of <500 ng/mL ( P =.001).
| Cervical length groups, mm | Fetal fibronectin groups, n | Total | ||||
|---|---|---|---|---|---|---|
| <10 ng/mL | 10–49 ng/mL | 50–199 ng/mL | 200–499 ng/mL | ≥500 ng/mL | ||
| <15 | 19 (1 PTB, 5%) | 18 (1 PTB, 6%) | 19 (5 PTB, 26%) | 33 (13 PTB, 39%) | 14 (9 PTB, 64%) | 103 (29 PTB, 28%) |
| 15–29 | 78 (2 PTB, 3%) | 86 (1 PTB, 1%) | 45 (4 PTB, 9%) | 44 (7 PTB, 16%) | 17 (3 PTB, 18%) | 270 (17 PTB, 6%) |
| 30–50 | 37 (0 PTB) | 20 (0 PTB) | 12 (0 PTB) | 7 (0 PTB) | 6 (2 PTB, 33%) | 82 (2 PTB, 2%) |
| T otal | 134 (3 PTB, 2%) | 124 (2 PTB, 2%) | 76 (9 PTB, 12%) | 84 (20 PTB, 24%) | 37 (14 PTB, 38%) | 455 (48 PTB, 11%) |
Tables 3 and 4 show the risk stratification for nulliparous women only (n=249) and women without a history of preterm birth (n=383), respectively. The results were similar to those of the complete group, which showed an increased risk of preterm birth within 7 days with increasing fFN concentration and shortening of the cervix. Women with a long cervix were still identified as high risk with a threshold of >500 ng/mL, although this did not show to be significant ( Table 3 : P =.14; Table 4 : P =.07). A threshold of 10 ng/mL in women with a short cervix did not help to identify more women who were at low risk.
| Cervical length groups, mm | Fetal fibronectin groups, n | Total | ||||
|---|---|---|---|---|---|---|
| <10 ng/mL | 10–49 ng/mL | 50–199 ng/mL | 200–499 ng/mL | ≥500 ng/mL | ||
| <15 | — | 14 (1 PTB, 7%) | 10 (2 PTB, 20%) | 23 (9 PTB, 39%) | 12 (8 PTB, 67%) | 73 (21 PTB, 29%) |
| 15–29 | 47 (1 PTB, 2%) | 43 (1 PTB, 2%) | 22 (2 PTB, 9%) | 22 (2 PTB, 9%) | 14 (1 PTB, 7%) | 148 (7 PTB, 5%) |
| 30–50 | 11 (0 PTB) | 7 (0 PTB) | 3 (0 PTB) | 3 (0 PTB) | 4 (1 PTB, 25%) | 28 (1 PTB, 4%) |
| Total | 72 (2 PTB, 3%) | 64 (2 PTB, 3%) | 35 (4 PTB, 11%) | 48 (11 PTB, 23%) | 30 (10 PTB, 33%) | 249 (29 PTB, 12%) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


