The ovaries have an outer cortex covered by ‘germinal’ epithelium (the most common carcinoma derives from this layer). The inner medulla contains connective tissue and blood vessels. The cortex contains the follicles and theca cells. Oestrogen is secreted by granulosa cells in the growing follicles and also by theca cells. The rare tumours of these cells secrete oestrogens. A few follicles start to enlarge every month [→ p.11] under the influence of pituitary follicle-stimulating hormone (FSH), but only one will reach about 20 mm in size and rupture in response to the mid-cycle surge of pituitary luteinizing hormone (LH) to release its oocyte (see Fig. 2.3). After ovulation, the collapsed follicle becomes a corpus luteum, which continues to produce oestrogen and progesterone to support the endometrium whilst awaiting fertilization and implantation. If none occurs then the corpus luteum involutes, hormone levels decline and menstruation begins. If fertilization and implantation occur then human chorionic gonadotrophin (hCG) produced from trophoblast maintains corpus luteum function and hormone production until 7–9 weeks’ gestation when the fetoplacental unit takes over. Follicular and lutein cysts result from persistence of these structures in non-pregnant women.
Ovarian Symptoms
Ovarian masses are often silent and detected either when they are very large and cause abdominal distension, or on ultrasound scan. Acute presentation is associated with ‘accidents’.
Ovarian Cyst ‘Accidents’
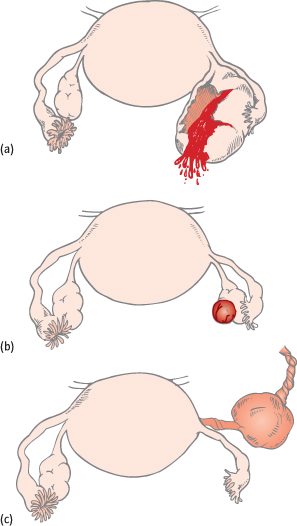
Rupture of the contents of an ovarian cyst into the peritoneal cavity causes intense pain, particularly with an endometrioma or dermoid cyst (Fig. 5.2a). Haemorrhage into a cyst (Fig. 5.2b) or the peritoneal cavity often causes pain. Peritoneal cavity haemorrhage is occasionally so severe as to cause hypovolaemic shock. Torsion of the pedicle (bulky due to the cyst) causes infarction of the ovary ± tube and severe pain (Fig. 5.2c). Urgent surgery and detorsion is required if the ovary is to be saved.
Fig. 5.2 (a) Rupture of an ovarian cyst. (b) Haemorrhage into an ovarian cyst (view from the abdomen). (c) Cyst twisting on its blood supply.
Disorders of Ovarian Function
Polycystic ovary syndrome (PCOS) is a common disorder that causes oligomenorrhoea, hirsutism and subfertility [→ p.83]. The ‘cysts’ are actually small, multiple, poorly developed follicles.
Premature menopause is when the last period is reached before the age of 40 years [→ p.109].
Problems of gonadal development include the gonadal dysgeneses, the most common of which is Turner’s syndrome [→ p.17].
Classification of Ovarian Tumours
Primary Neoplasms
These can be benign or malignant. They are classified together because a benign cyst may undergo malignant change. They fall into three main groups.
Epithelial Tumours
Derived from the epithelium covering the ovary, these are most common in postmenopausal women. Uniquely, histology may demonstrate ‘borderline’ malignancy, when malignant histological features are present but invasion is not. Such tumours may become frankly malignant: surgery is advised but their optimum management is disputed. In younger women with a borderline cyst, close observation may be offered following removal only of the cyst or affected ovary to retain fertility. Recurrence, as a borderline or invasive tumour, can occur up to 20 years later.
Serous Cystadenoma or Adenocarcinoma:
The malignant variety is the most common malignant ovarian neoplasm (50% of malignancies). Benign and ‘borderline’ forms also exist.
Mucinous cystadenoma or adenocarcinoma can become very large and are less frequently malignant (10% of ovarian malignancies). A rare ‘borderline’ variant is pseudomyxoma peritonei, in which the abdominal cavity fills with gelatinous mucin secretions. An appendiceal primary tumour should be excluded.
Endometrioid Carcinoma:
This malignant variant accounts for 25% of ovarian malignancies. It is similar histologically to endometrial carcinoma, with which it is associated in 20% of cases.
Clear cell carcinoma is a malignant variant that accounts for less than 10% of ovarian malignancies but has a particularly poor prognosis.
Brenner tumours are rare and usually small and benign.
Germ Cell Tumours
These originate from the undifferentiated primordial germ cells of the gonad.
Teratoma or dermoid cyst is a common benign tumour usually arising in young premenopausal women. It may contain fully differentiated tissue of all cell lines, commonly hair and teeth. They are commonly bilateral, seldom large and often asymptomatic. However, rupture is very painful. A malignant form, the solid teratoma, also occurs in this age group but is very rare.
Dysgerminoma is the female equivalent of the seminoma. Although rare, it is the most common ovarian malignancy in younger women. It is sensitive to radiotherapy.
Sex Cord Tumours
These originate from the stroma of the gonad.
Granulosa cell tumours are usually malignant but slow growing. They are rare and are usually found in postmenopausal women. They secrete high levels of oestrogens and inhibin: stimulation of the endometrium can cause bleeding, endometrial hyperplasia, endometrial malignancy and, rarely, in young girls, precocious puberty. Serum inhibin levels are used as tumour markers to monitor for recurrence.
Thecomas are very rare, usually benign, and can secrete both oestrogens or androgens.
Fibromas are rare and benign. They can cause Meigs’ syndrome, whereby ascites and a (usually) right pleural effusion are found in conjunction with the small ovarian mass. The effusion is benign and cured by removal of the mass.
Common Ovarian Masses
| Premenopausal: | Follicular/ lutein cysts |
| Dermoid cysts | |
| Endometriomas | |
| Benign epithelial tumour | |
| Postmenopausal: | Benign epithelial tumour |
| Malignancy |
Secondary Malignancies
The ovary is a common site for metastases, particularly from the breast and gastrointestinal tract. Secondaries account for 10% of malignant ovarian masses. A few contain ‘signet-ring’ cells and if from the gut are called Krukenberg tumours. The primary malignancy may be difficult to detect and the prognosis is very poor.
Tumour-Like Conditions
The word ‘cyst’ can include anything from the malignant to the physiological, but is often interpreted as cancer by patients.
Endometriotic Cysts:
Endometriosis commonly causes altered blood to accumulate in ‘chocolate cysts’. In the ovary, such cysts are called endometriomas. Rupture is very painful though uncommon.
Functional Cysts:
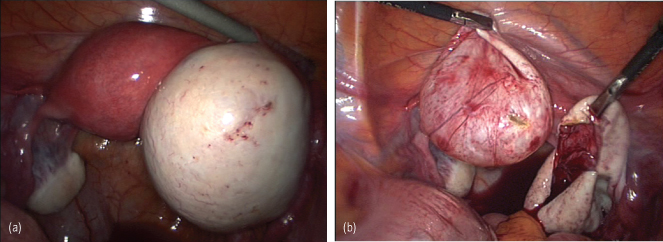
Follicular cysts and lutein cysts are persistently enlarged follicles and corpora lutea, respectively. They are therefore only found in premenopausal women. The combined pill protects against functional cysts by inhibiting ovulation. Lutein cysts tend to cause more symptoms. If symptoms are absent, treatment is not required and the cyst is observed using serial ultrasound scans. However, because of the remote possibility of malignancy, if an apparently functional cyst >5 cm persists beyond 2 months, the serum cancer antigen 125 (CA 125) level is measured and a laparoscopy considered to remove or drain the cyst (Fig. 5.3).
Fig. 5.3 (a) Laparoscopic photograph of a right ovarian benign epithelial cyst. (b) The cyst stripped and taken from within the ovary. The ovary returns to normal size within weeks of the operation.
Ovarian Cancer
The silent nature of this malignancy causes it to present late. The 5-year survival rate is therefore below 35%.
Epidemiology
There are over 6600 new cases per year in the UK, causing 4400 deaths. The lifetime risk of developing ovarian cancer in the UK is 1 in 48. Rates increase with age and over 80% of cases occur in women over 50 years of age, with the highest age-specific incidence rates in women aged 80–84. There is marked geographical variation. After decades of increasing incidence, a steady slow fall has been noted in the UK and many other European countries since the early 2000s. This may be due to widespread use of the oral contraceptive pill (OCP), which reduces risk.
Histological Types of Primary Ovarian Malignancy
| Serous cystadenocarcinoma | 50% |
| Endometrioid carcinoma | 20% |



